Abstract
-
Objectives
- This study aimed to disseminate information on coronavirus disease 2019 (COVID-19) vaccine safety among adolescents aged 12 to 17 years in the Republic of Korea.
-
Methods
- Two databases were used to assess COVID-19 vaccine safety in adolescents aged 12 to 17 years who completed the primary Pfizer-BioNTech vaccination series. Adverse events reported to the web-based COVID-19 vaccination management system (CVMS) and collected in the text message-based system were analyzed.
-
Results
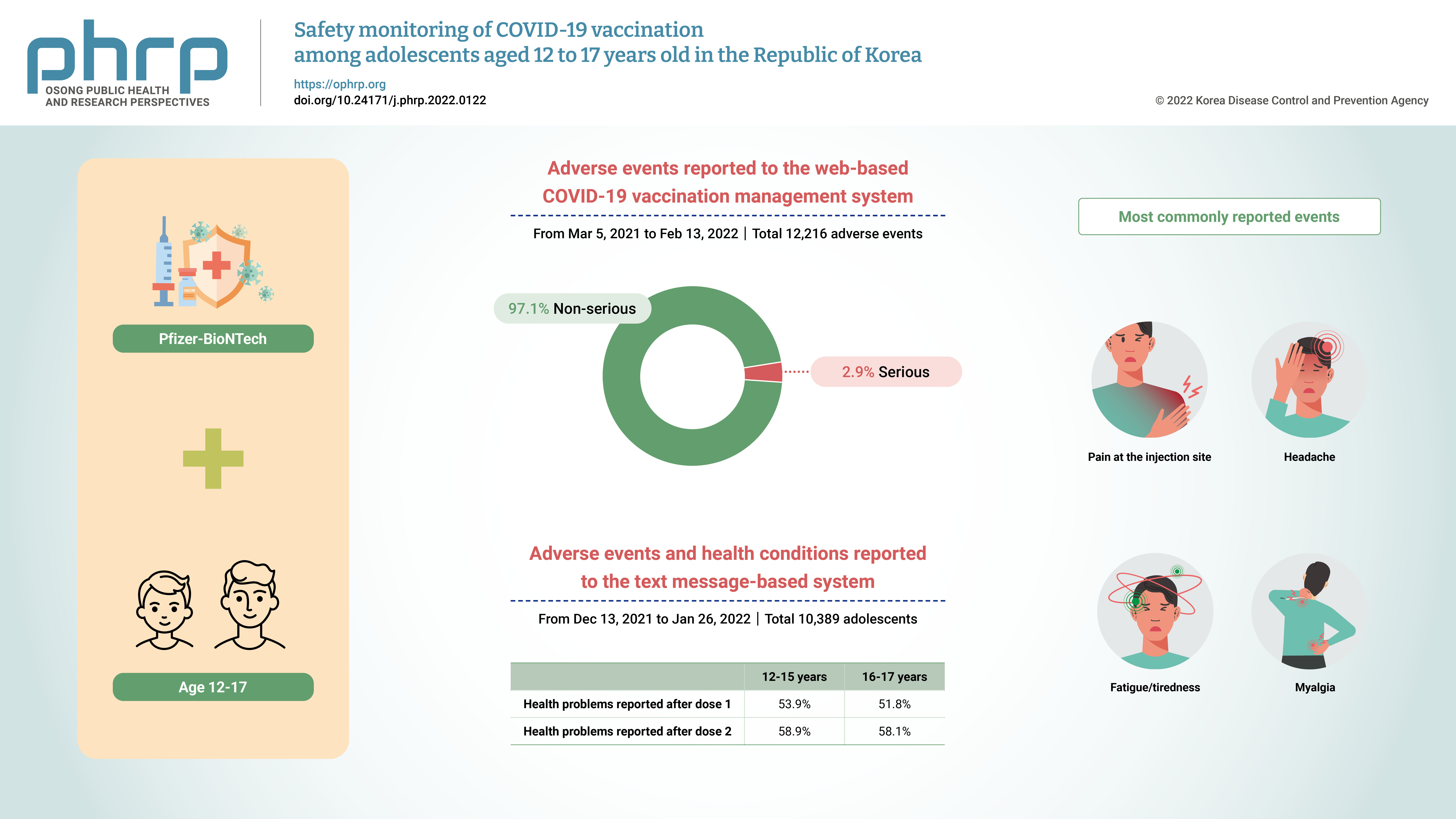
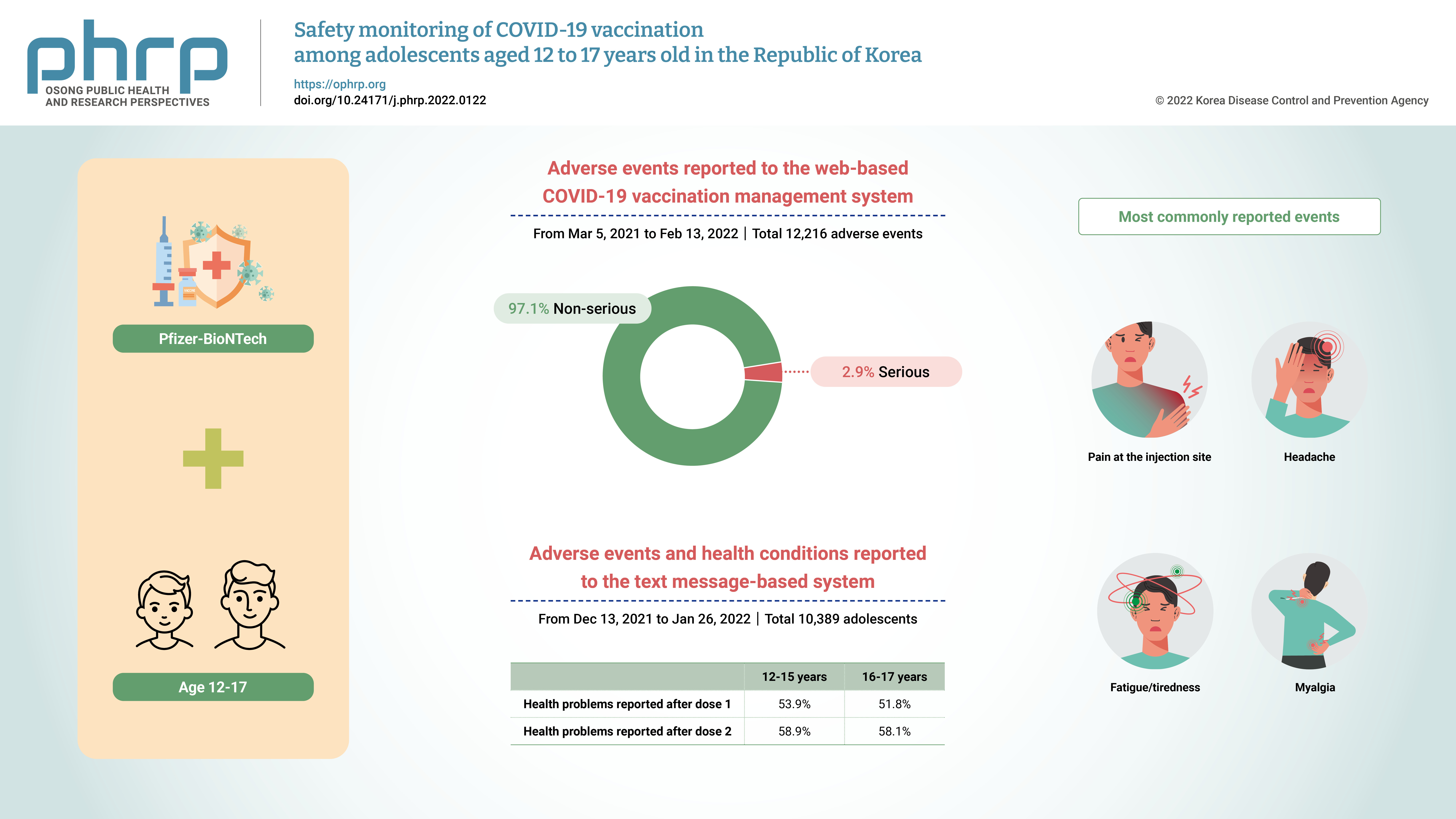
- From March 5, 2021 to February 13, 2022, 12,216 adverse events among 12- to 17-year-olds were reported to the CVMS, of which 97.1% were non-serious adverse events and 2.9% were serious adverse events, including 85 suspected cases of anaphylaxis, 74 suspected cases of myocarditis and/or pericarditis, and 2 deaths. From December 13, 2021 to January 26, 2022, 10,389 adolescents responded to a text message survey, and local/systemic adverse events were more common after dose 2 than after dose 1. The most commonly reported events following either vaccine dose were pain at the injection site, headache, fatigue/tiredness, and myalgia.
-
Conclusion
- The overall results are consistent with previous findings; the great majority of adverse events were non-serious, and serious adverse events were rare among adolescents aged 12 to 17 years following Pfizer-BioNTech COVID-19 vaccination.
-
Keywords: Adolescent; COVID-19; Safety; Vaccination; Vaccines
Graphical abstract
Introduction
- Coronavirus disease 2019 (COVID-19) vaccination has been available since February 26, 2021 in the Republic of Korea (ROK) to prevent the occurrence of severe cases leading to hospitalization and death by reducing the risk of infection and transmission [1]. To date, only the Pfizer-BioNTech mRNA COVID-19 vaccine has been authorized for use in adolescents aged 12 to 17 years by the Korea Ministry of Food and Drug Safety (MFDS), on the basis of safety and efficacy data from controlled trials conducted in the United States (US) [2,3]. The Korea MFDS initially approved the use of the Pfizer-BioNTech vaccine for persons aged ≥16 years on March 5, 2021 [4], and expanded it to include adolescents aged ≥12 years on July 16, 2021 [5]. Following the 19th Korea Advisory Committee on Immunization Practices (KACIP), the Pfizer-BioNTech vaccine was offered to adolescents aged 16 to 17 years starting on October 18, 2021 and to adolescents aged 12 to 15 years starting on November 1, 2021, with a 3-week interval between dose 1 and dose 2 [6,7].
- Since then, COVID-19 vaccines have been widely distributed to adolescents aged 12 to 17 years across the nation, and vaccination coverage in this population trended upward, reaching 46.9% for dose 1 and 24.9% for dose 2 as of December 1, 2021 [8]. To make COVID-19 vaccinations more accessible and boost the vaccinations rate for adolescents, the Korea Disease Control and Prevention Agency (KDCA) announced a 2-week mass vaccination strategy during December 13–24, 2021, to vaccinate adolescents aged 12 to 17 years at schools, vaccination centers, public health centers in cooperation with the Korea Ministry of Education [8]. In addition, a text message survey for those aged 12 to 17 years was launched when the mass vaccination strategy was initiated to monitor and investigate adverse events or health conditions after COVID-19 vaccination.
- As information on COVID-19 vaccine safety for adolescents aged 12 to 17 years is currently limited in real-world settings, this study aimed to identify and disseminate information on COVID-19 vaccine safety for adolescents aged 12 to 17 years in the ROK who completed the primary Pfizer-BioNTech vaccination series, including the first and second doses. This study analyzed data on adverse events reported to the COVID-19 vaccination management system (CVMS; a web-based passive vaccine safety surveillance system) and a web-based passive vaccine safety surveillance system) and the text message-based vaccine safety surveillance system.
Materials and Methods
- COVID-19 Vaccination Management Systemm
- In order to monitor adverse events following immunization (AEFIs) and identify potential safety signals for further evaluation, the KDCA manages the CVMS, in which doctors and forensic pathologists can report AEFIs regardless of a causal association between the events and the vaccines in accordance with the Infectious Disease Control and Prevention Act [9]. From March 5, 2021 to February 13, 2022, a total of 4,340,710 primary doses of the Pfizer-BioNTech vaccination series were administered to adolescents aged 12 to 17 years in the ROK, and 12,216 adverse events after vaccination were reported to the CVMS. Data on an additional dose (dose 3) and vaccines other than the Pfizer-BioNTech vaccine were excluded as they were not authorized for use in adolescents aged 12 to 17 years during the study period in the ROK. Adverse events reported to the CVMS are classified into non-serious and serious events as per the Guidelines for Adverse Events Following COVID-19 Immunization in the ROK [9]. Non-serious events include common symptoms, such as redness at the injection site, pain, swelling, myalgia, fever, headache, chills, and others. The following adverse events are classified as serious: death, suspected anaphylaxis, adverse events of special interest (AESIs), intensive care unit admission, life-threatening events, permanent disability or sequelae, and others. The characteristics of adverse events reported in the CVMS among adolescents aged 12 to 17 years were stratified by sex, age groups, and vaccine doses, and the types of symptoms and signs reported as adverse events were described in descending order of the number of cases. Since adverse events reported to the CVMS are suspected cases, the events do not indicate medically confirmed diagnoses.
- Text Message-Based Vaccine Safety Surveillance System
- The KDCA operates a text message-based vaccine safety surveillance system that surveys adverse events and health conditions after COVID-19 vaccination for specific population groups, such as pregnant women who consent to receive text message surveys through their smartphones on the day of their first vaccination [9]. Text messages were sent on a daily basis until day 7 post-vaccination to check health conditions. In total, 10,398 adolescents aged 12 to 17 years in the ROK who received the primary series of the Pfizer-BioNTech vaccine responded to text message surveys from December 13, 2021 to January 26, 2022. The surveys included questions about any health problems experienced after vaccination, fever, local and systemic adverse events, limits to normal daily activities, and visits to medical facilities. The respondents were able to report multiple adverse events on various days. The characteristics of 10,398 respondents aged 12 to 17 years were described according to sex and age, and adverse events and health conditions were assessed in terms of age groups and vaccine doses.
- SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA) was used to conduct all the analyses in this study. The passive surveillance activity was conducted and authorized by the KDCA; the study was not subject to the institutional review board approval under government regulations. The study with the text message-based surveillance was exempted from review by the Korea Public Institutional Review Board designated by the Ministry of Health and Welfare (P01-202203-01-035).
Results
- COVID-19 Vaccination Management System
- From March 5, 2021 to February 13, 2022, the CVMS confirmed 12,216 adverse events among adolescents aged 12 to 17 years after primary doses of the Pfizer-BioNTech vaccination series (Table 1); 11,867 (97.1%) were non-serious and 349 (2.9%) were serious. Serious adverse events included death (2, 0%), suspected anaphylaxis (85, 0.7%) and major adverse events, including AESIs for COVID-19 vaccines (262, 2.1%). In total, 4,340,710 doses were administered to adolescents aged 12 to 17 years during the study period and the overall reporting rate per 100,000 doses was 281.4 (295.8 after receipt of dose 2 and 268.1 after receipt of dose 1). The reporting rate per 100,000 doses after the primary vaccination series was 271.5 in males and 291.9 in females, and 16- to 17-year-olds (370.0) showed a higher reporting rate than 12- to 15-year-olds (224.6). Two deaths were reported in males aged 16 to 17 years after receipt of dose 2. Among 11,867 (97.1%) non-serious adverse events, the most commonly reported symptoms based on the reporting rate per 100,000 doses were headache (74.0), chest pain (72.0), myalgia (42.5), dizziness (39.9), and nausea (36.2) (Table 2). Among 349 (2.9%) serious adverse events, acute cardiovascular injury (2.1), including 74 cases of suspected myocarditis and/or pericarditis, showed the highest reporting rate per 100,000 doses, followed by anaphylaxis, including anaphylactoid reactions (2.0), convulsions or seizures (0.9), acute paralysis (0.8), and vaccine-associated enhanced disease (0.7).
- Text Message-Based Vaccine Safety Surveillance System
- From December 13, 2021 to January 26, 2022, a total of 10,389 adolescents aged 12 to 17 years responded to at least 1 text message survey on days 0 to 7 after Pfizer-BioNTech COVID-19 vaccination (Table 3); 8,909 (85.8%) were 12- to 15-year-olds and 1,480 (14.2%) were 16- to 17-year-olds. Among them, 4,828 (46.5%) were male and 5,561 (53.5%) were female. During days 0 to 7 post-vaccination, health problems among those aged 12 to 15 years were more common after dose 2 (58.9%) than after dose 1 (53.9%) (Table 4). The reporting trend was similar for those aged 16 to 17 years: health problems were reported by 58.1% of respondents after dose 2 and 51.8% after dose 1. Fewer than one-quarter of adolescents in both age groups reported fever or a sensation of heat after dose 2. Among those aged 12 to 15 years, local adverse events (53.2%) and systemic adverse events (52.3%) were reported more frequently after dose 2 than after dose 1. The reporting trends were similar for those aged 16 to 17 years, of whom 52.6% reported local adverse events and 53.8% reported systemic adverse events after dose 2. The most commonly reported adverse events among both age groups following either dose 1 or dose 2 were as follows: pain at the injection site, headache, fatigue or tiredness, myalgia, and fever or a sensation of heat. Almost one-fifth (18.6%) of adolescents aged 12 to 15 years responded that they were unable to perform normal daily activities after dose 2. This reporting rate was slightly higher in those aged 16 to 17 years (25.6%). More than 1% of adolescents aged 12 to 17 years visited medical facilities, including emergency departments, clinics, or hospitals, during days 0 to 7 after receiving either dose.
Discussion
- The results of the text message survey on AEFIs and subjective health problems among adolescents aged 12 to 17 years after the primary series of Pfizer-BioNTech COVID-19 vaccination are consistent with the safety data including adolescents aged 12 to 17 years reported in the US [10] and a controlled trial [2]; local and systemic adverse events, including fever, following vaccination were more common after dose 2 and were mostly mild and did not limit daily activities. Moreover, similar to the findings reported in the US and a controlled trial [2,10], the most common local adverse event was pain at the injection site, and the most common systemic adverse events were headache, fatigue, and myalgia in this study. Those adverse events were more frequently reported in 16- to 17-year-olds than in 12- to 15-year-olds in both the ROK and the US [10].
- Among the adverse events reported to the CVMS for adolescents aged 12 to 17 years after Pfizer-BioNTech COVID-19 vaccination, 97.1% were non-serious and 2.9% were serious. These proportions are slightly different from those in safety data in adolescents reported in the US, where 90.7% were non-serious reports and 9.3% were serious reports [10]. This might be attributed to different standards used in the 2 surveillance systems to assess and define non-serious and serious adverse events. However, the great majority of adverse events reported by adolescents aged 12 to 17 years following vaccination were non-serious in both the ROK and the US.
- Based on the early safety monitoring for adolescents aged 12 to 17 years after Pfizer-BioNTech COVID-19 vaccination, serious adverse events, including 85 cases of suspected anaphylaxis (2.0 cases per 100,000 doses administered) and acute cardiovascular injury (including 74 cases of suspected myocarditis and/or pericarditis; 1.7 cases per 100,000 doses administered) appear to be rarely reported. Reviewing these 2 major serious adverse events, the number of suspected anaphylaxis reports in adolescents after vaccination was greater after dose 1 (71, 83.5%) than after dose 2 (14, 16.5%), but similar between females (47, 55.3%) and males (38,44.7%). In previous reports from the ROK and the US, most cases of confirmed anaphylaxis based on the Brighton Collaboration case definition criteria among all age groups after Pfizer-BioNTech COVID-19 vaccination were reported in women (70.9%–93.6%) [11,12]. Moreover, the number of suspected myocarditis and/or pericarditis reports was higher in males (59, 79.7%) than in females (15, 20.3%), and after dose 2 (50, 67.6%) than after dose 1 (24, 32.4%) in this study; these findings are consistent with a meta-analysis showing that the incidence of myopericarditis was significantly higher in males and after receiving dose 2 [13]. However, since the current study is based on reports of suspected cases including anaphylaxis and myocarditis and/or pericarditis due to limited information available in early safety monitoring, diagnostic bias might exist and the assessment of causality between adverse events and vaccines is constrained at this stage. Therefore, we suggest that follow-up work should be conducted with the confirmation of suspected cases in adolescents after COVID-19 vaccination for further evaluation.
- Although a few COVID-19 vaccine-associated myocarditis and/or pericarditis cases have been reported among adolescents aged 12 to 17 years, predominantly among males, after dose 2 of Pfizer-BioNTech vaccination, most cases were mild [14–18]. Since those cases are rarely reported and patients can recover quickly if responded to and treated well, the benefits of COVID-19 vaccination, including for adolescents, are considered to outweigh the risks of myocarditis and/or pericarditis [19–22]. Furthermore, a systematic review concluded that the COVID-19 vaccine for children and adolescents is effective with no major safety issues based on 36 clinical studies [23], and a meta-analysis also demonstrated that the incidence of myopericarditis after COVID-19 vaccination was not higher than that reported after other standard vaccinations including smallpox and influenza vaccines [13]. In this respect, this study does not support actions to exclude adolescents aged 12 to 17 years from vaccination; instead, we recommend that adverse events, including myocarditis and/or pericarditis after COVID-19 vaccination, should be closely monitored to respond and provide further information on COVID-19 vaccine safety [24].
- The number of deaths reported among adolescents aged 12 to 17 years after Pfizer-BioNTech COVID-19 vaccination was 2, and both were among males aged 16 to 17 years after receipt of dose 2 in this study. For rapid responses in the ROK, the Vaccine Injury Investigation Committee (VIIC) has been reviewing all death reports to evaluate the causality between death and vaccination [11]. These 2 deaths were assessed not to be associated with the vaccination based on medical records, death certificates, autopsy, and epidemiological investigation results.
- This study has some limitations. First, data were calculated using information on suspected adverse events after COVID-19 vaccination; thus, the results do not indicate an accurate diagnosis or causality between the events and the vaccines. Second, since adverse events reported to the CVMS are based on persons who visit medical institutions, the reports might have been subject to underreporting. Third, the results of text message surveys solely relied on self-reported responses; thus, the number of adverse events reported might have been overestimated due to the likelihood of responding by their parents or guardians. Fourth, as text messages were sent to adolescents aged 12 to 17 years during a particular period of time, the findings cannot be generalized to the entire adolescent population in the ROK; therefore, caution needs to be exercised in interpreting the results. Nevertheless, to the best of our knowledge, this is the first study on COVID-19 vaccine safety in adolescents aged 12 to 17 years in real-world settings in the ROK using national vaccine safety surveillance data managed by the Korean government. This study found consistent safety information on Pfizer-BioNTech COVID-19 vaccination with the US and a controlled trial; serious adverse events following vaccination were extremely rare among adolescents aged 12 to 17 years. No deaths associated with the vaccine were demonstrated as a result of the causality assessment conducted by the VIIC. We will continue to closely monitor any adverse events, including anaphylaxis and myocarditis and/or pericarditis cases, after COVID-19 vaccination for adolescents and share up-to-date information on vaccine safety with policymakers and committees to support the development of evidence-based guidelines.
Article information
-
Ethics Approval
The passive surveillance activity was conducted and authorized by the public health authority; the study was not subject to institutional review board approval under government regulations. The study with the text message-based surveillance was exempted from review by the Public Institutional Review Board designated by the Korea Ministry of Health and Welfare (No. P01-202203-01-035).
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The data used in this study are protected under the Personal Information Protection Act.
-
Authors’ Contributions
Conceptualization: YK, YKL; Data curation: SK, IH, MK; Formal analysis: SK, IH; Investigation: SK, MK; Methodology: all authors; Validation: YK, YKL; Writing-original draft: SK, YKL; Writing-review & editing: all authors.
Acknowledgements- We thank the relevant ministries including the Ministry of Interior and Safety, cities and provinces, and medical staff in health centers and medical facilities for their efforts in responding to the vaccine safety surveillance.
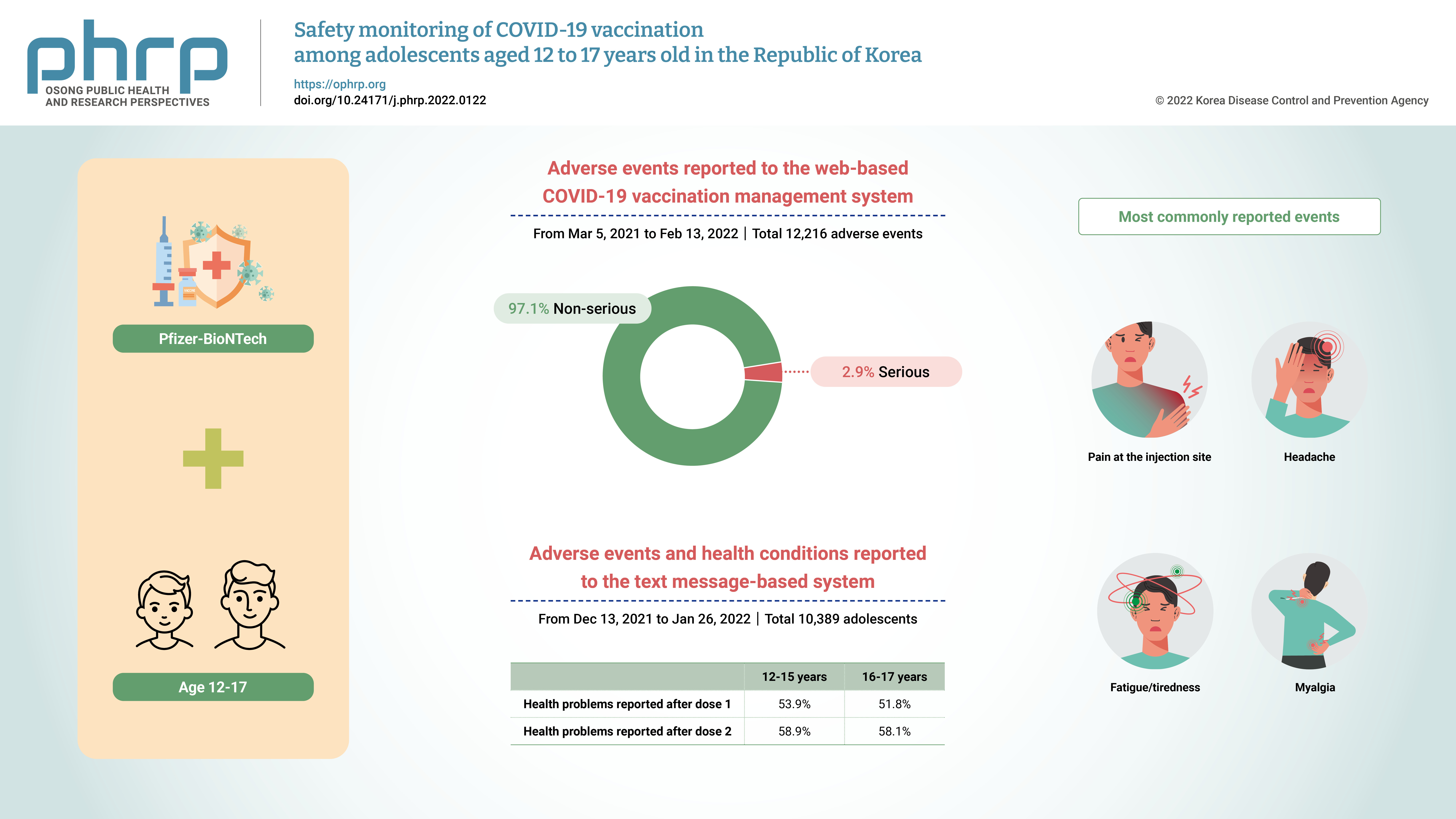
Table 1.Characteristics of adverse events reported to the CVMS for adolescents aged 12 to 17 years after Pfizer-BioNTech COVID-19 vaccination, Republic of Korea, March 5, 2021 to February 13, 2022
|
Variable |
Number of doses administered |
Adverse events (n=12,216)a)
|
|
Total |
Non-serious adverse eventsb)
|
Serious adverse eventsc)
|
|
Sub-total |
Death |
Anaphylaxis |
Others |
|
Total |
4,340,710 |
12,216 (281.4) |
11,867 (273.4) |
349 (8.0) |
2 (0) |
85 (2.0) |
262 (6.0) |
|
Dose 1 |
2,254,487 |
6,044 (268.1) |
5,845 (259.3) |
199 (8.8) |
0 |
71 (3.1) |
128 (5.7) |
|
Dose 2 |
2,086,223 |
6,172 (295.8) |
6,022 (288.7) |
150 (7.2) |
2 (0.1) |
14 (0.7) |
134 (6.4) |
|
Sex |
|
|
|
|
|
|
|
|
Male |
2,229,864 |
6,055 (271.5) |
5,854 (262.5) |
201 (9.0) |
2 (0.1) |
38 (1.7) |
161 (7.2) |
|
Dose 1 |
1,158,684 |
2,915 (251.6) |
2,809 (242.4) |
106 (9.1) |
0 |
30 (2.6) |
76 (6.6) |
|
Dose 2 |
1,071,180 |
3,140 (293.1) |
3,045 (284.3) |
95 (8.9) |
2 (0.2) |
8 (0.7) |
85 (7.9) |
|
Female |
2,110,846 |
6,161 (291.9) |
6,013 (284.9) |
148 (7.0) |
0 |
47 (2.2) |
101 (4.8) |
|
Dose 1 |
1,095,803 |
3,129 (285.5) |
3,036 (277.1) |
93 (8.5) |
0 |
41 (3.7) |
52 (4.7) |
|
Dose 2 |
1,015,043 |
3,032 (298.7) |
2,977 (293.3) |
55 (5.4) |
0 |
6 (0.6) |
49 (4.8) |
|
Age (y) |
|
|
|
|
|
|
|
|
12–15 |
2,644,362 |
5,940 (224.6) |
5,762 (217.9) |
178 (6.7) |
0 |
42 (1.6) |
136 (5.1) |
|
Dose 1 |
1,424,052 |
3,026 (212.5) |
2,918 (204.9) |
108 (7.6) |
0 |
36 (2.5) |
72 (5.1) |
|
Dose 2 |
1,220,310 |
2,914 (238.8) |
2,844 (233.1) |
70 (5.7) |
0 |
6 (0.5) |
64 (5.2) |
|
16–17 |
1,696,348 |
6,276 (370.0) |
6,105 (359.9) |
171 (10.1) |
2 (0.1) |
43 (2.5) |
126 (7.4) |
|
Dose 1 |
830,435 |
3,018 (363.4) |
2,927 (352.5) |
91 (11.0) |
0 |
35 (4.2) |
56 (6.7) |
|
Dose 2 |
865,913 |
3,258 (376.3) |
3,178 (367.0) |
80 (9.2) |
2 (0.2) |
8 (0.9) |
70 (8.1) |
Table 2.Types of symptoms and signs reported to the CVMS for adolescents aged 12 to 17 years after Pfizer-BioNTech COVID-19 vaccination, Republic of Korea, March 5, 2021 to February 13, 2022
|
Symptoms and signs (n=12,216)a)
|
Case (per 100,000) |
|
Non-serious adverse events (n=11,867) |
|
|
Headache |
3,214 (74.0) |
|
Chest pain |
3,127 (72.0) |
|
Myalgia |
1,845 (42.5) |
|
Dizziness |
1,732 (39.9) |
|
Nausea |
1,573 (36.2) |
|
Fever |
1,183 (27.3) |
|
Vomiting |
754 (17.4) |
|
Abdominal pain |
748 (17.2) |
|
Allergy reactions |
745 (17.2) |
|
Chills |
692 (15.9) |
|
Pain, redness or swelling at the injection site within 3 days after |
455 (10.5) |
|
Diarrhea |
451 (10.4) |
|
Lymphadenitis |
381 (8.8) |
|
Abnormal uterine bleeding |
130 (3.0) |
|
Cellulitis |
58 (1.3) |
|
Arthritis |
44 (1.0) |
|
Severe local adverse events |
29 (0.7) |
|
Abscess at the injection site |
2 (0) |
|
Systemic disseminated Bacillus Calmette-Guerin infection |
1 (0) |
|
Severe adverse events (n=349) including reports of death |
|
|
Acute cardiovascular injury |
90 (2.1) |
|
Anaphylaxis (including anaphylactoid reactions) |
85 (2.0) |
|
Convulsions or seizures |
40 (0.9) |
|
Acute paralysis |
33 (0.8) |
|
Vaccine-associated enhanced disease |
30 (0.7) |
|
Acute respiratory distress syndrome |
14 (0.3) |
|
Encephalopathy or encephalitis |
11 (0.3) |
|
Thrombocytopenic purpura |
6 (0.1) |
|
Thrombocytopenia |
5 (0.1) |
|
Acute kidney injury |
4 (0.1) |
|
Osteitis or osteomyelitis |
4 (0.1) |
|
Erythema multiforme |
3 (0.1) |
|
Coagulation disorder |
3 (0.1) |
|
Thrombosis with thrombocytopenia syndrome |
3 (0.1) |
|
Anosmia or ageusia |
3 (0.1) |
|
Acute liver injury |
2 (0) |
|
Meningoencephalitis |
2 (0) |
|
Multisystem inflammatory syndrome |
2 (0) |
|
Single organ cutaneous vasculitis |
2 (0) |
|
Acute disseminated encephalomyelitis |
1 (0) |
|
Chilblains |
1 (0) |
|
Guillain-Barre syndrome |
1 (0) |
Table 3.Characteristics of adolescents aged 12 to 17 years a)
|
Characteristic |
Dose 1 (n=10,389) |
Dose 2 (n=3,147) |
|
Sex |
|
|
|
Male |
4,828 (46.5) |
1,436 (45.6) |
|
Female |
5,561 (53.5) |
1,711 (54.4) |
|
Age (y) |
|
|
|
12–15 |
8,909 (85.8) |
2,744 (87.2) |
|
12 |
1,948 (18.8) |
639 (20.3) |
|
13 |
2,432 (23.4) |
766 (24.3) |
|
14 |
1,857 (17.9) |
584 (18.6) |
|
15 |
2,672 (25.7) |
755 (24.0) |
|
16–17 |
1,480 (14.2) |
403 (12.8) |
|
16 |
864 (8.3) |
247 (7.8) |
|
17 |
616 (5.9) |
156 (5.0) |
Table 4.Adverse events and health conditions reported by adolescents aged 12 to 17 years following Pfizer-BioNTech COVID-19 vaccination, Republic of Korea, December 13, 2021 to January 26, 2022
|
Eventsa)
|
Age group (12–15 y) |
Age group (16–17 y) |
|
Dose 1 (n=8,909) |
Dose 2 (n=2,744) |
Dose 1 (n=1,480) |
Dose 2 (n=403) |
|
Health problemsb)
|
4,803 (53.9) |
1,617 (58.9) |
766 (51.8) |
234 (58.1) |
|
Fever or sensation of heat |
694 (7.8) |
634 (23.1) |
103 (7.0) |
89 (22.1) |
|
Local adverse events |
4,323 (48.5) |
1,460 (53.2) |
686 (46.4) |
212 (52.6) |
|
Pain |
3,978 (44.7) |
1,346 (49.1) |
634 (42.8) |
200 (49.6) |
|
Redness |
195 (2.2) |
88 (3.2) |
39 (2.6) |
20 (5.0) |
|
Swelling |
843 (9.5) |
316 (11.5) |
130 (8.8) |
55 (13.6) |
|
Itching |
232 (2.6) |
95 (3.5) |
44 (3.0) |
12 (3.0) |
|
Urticaria |
42 (0.5) |
13 (0.5) |
9 (0.6) |
1 (0.2) |
|
Others |
506 (5.7) |
164 (6.0) |
86 (5.8) |
31 (7.7) |
|
Systemic adverse events |
3,736 (41.9) |
1,434 (52.3) |
615 (41.6) |
217 (53.8) |
|
Chills |
494 (5.5) |
386 (14.1) |
102 (6.9) |
66 (16.4) |
|
Headache |
1,455 (16.3) |
853 (31.1) |
262 (17.7) |
146 (36.2) |
|
Joint pain |
218 (2.4) |
146(5.3) |
48 (3.2) |
35 (8.7) |
|
Myalgia |
2,070 (23.2) |
729 (26.6) |
404 (27.3) |
136 (33.7) |
|
Fatigue or tiredness |
1,753 (19.7) |
748 (27.3) |
338 (22.8) |
144 (35.7) |
|
Nausea |
577 (6.5) |
267 (9.7) |
103 (7.0) |
55 (13.6) |
|
Vomiting |
35 (0.4) |
24 (0.9) |
12 (0.8) |
4 (1.0) |
|
Diarrhea |
188 (2.1) |
68 (2.5) |
36 (2.4) |
13 (3.2) |
|
Abdominal pain |
326 (3.7) |
145 (5.3) |
53 (3.6) |
26 (6.5) |
|
Rash |
25 (0.3) |
11 (0.4) |
10 (0.7) |
5 (1.2) |
|
Armpit tenderness |
347 (3.9) |
286 (10.4) |
65 (4.4) |
41 (10.2) |
|
Others |
450 (5.1) |
152 (5.5) |
73 (4.9) |
28 (6.9) |
|
Unable to perform normal daily activities |
867 (9.7) |
510 (18.6) |
185 (12.5) |
103 (25.6) |
|
Visits to medical facilities |
100 (1.1) |
39 (1.4) |
16 (1.1) |
5 (1.2) |
|
Emergency department visit |
15 (0.2) |
6 (0.2) |
3 (0.2) |
1 (0.2) |
|
Hospitalization |
2 (0) |
0 |
0 |
0 |
|
Clinic visit |
87 (1.0) |
34 (1.2) |
13 (0.9) |
5 (1.2) |
References
- 1. Korea Disease Control and Prevention Agency (KDCA). COVID-19 vaccination [Internet]. Cheongju: KDCA; 2022 [cited 2022 Feb 24]. Available from: https://ncv.kdca.go.kr. Korean.
- 2. Frenck RW Jr, Klein NP, Kitchin N, et al. Safety, immunogenicity, and efficacy of the BNT162b2 covid-19 vaccine in adolescents. N Engl J Med 2021;385:239−50.ArticlePubMedPMC
- 3. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603−15.ArticlePubMedPMC
- 4. Ministry of Food and Drug Safety (MFDS). Press release: authorization for the Pfizer-BioNTech COVID-19 vaccine (BNT162b2) [Internet]. Cheongju: MFDS; 2021 [cited 2022 Feb 24]. Available from: https://www.mfds.go.kr/brd/m_99/view.do?seq=45117&srchFr=&srchTo=&srchWord=&srchTp=&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&page=1. Korean.
- 5. Ministry of Food and Drug Safety (MFDS). Press release: age expansion to use of the Pfizer-BioNTech COVID-19 vaccine (BNT162b2) [Internet]. Cheongju: MFDS; 2021 [cited 2022 Feb 24]. Available from: https://www.mfds.go.kr/brd/m_99/view.do?seq=45566&srchFr=&srchTo=&srchWord=접종+연령+확대&srchTp=0&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&Data_stts_gubun=C9999&page=1. Korean.
- 6. Korea Disease Control and Prevention Agency (KDCA). National immunization program: 2021 the 19th Korea Advisory Committee on Immunization Practices (KACIP) [Internet]. Cheongju: KDCA; 2021 [cited 2022 Feb 24]. Available from: https://nip.kdca.go.kr/irgd/introduce.do?MnLv1=4&MnLv2=1&MnLv3=2. Korean.
- 7. Ministry of Health and Welfare (MOHW). Press release: adolescents (16-17 years old) and pregnant women vaccination start from today (October 18, regular briefing) [Internet]. Cheongju: KDCA; 2021 [cited 2022 Feb 24]. Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=6016&contSeq=6016&board_id=312&gubun=BDJ. Korean.
- 8. Ministry of Education (MOE). Press release: announcement of public recommendations to increase vaccine uptake for adolescents aged 12-17 years old [Internet]. Sejong: MOE; 2021 [cited 2022 Feb 24]. Available from: https://www.moe.go.kr/boardCnts/viewRenew.do?boardID=294&boardSeq=89793&lev=0&searchType=null&statusYN=W&page=1&s=moe&m=020402&opType=N. Korean.
- 9. Korea Disease Control and Prevention Agency (KDCA). Guideline for adverse events following COVID-19 immunization [Internet]. 2nd ed. Cheongju: KDCA; 2021 [cited 2022 Feb 24]. Available from: https://www.kdca.go.kr/upload_comm/syview/doc.html?fn=163463647072000.pdf&rs=/upload_comm/docu/0019/. Korean.
- 10. Hause AM, Gee J, Baggs J, et al. COVID-19 vaccine safety in adolescents aged 12-17 years-United States, December 14, 2020-July 16, 2021. MMWR Morb Mortal Wkly Rep 2021;70:1053−8.ArticlePubMedPMC
- 11. Hwang I, Park K, Kim TE, et al. COVID-19 vaccine safety monitoring in Republic of Korea from February 26, 2021 to October 31, 2021. Osong Public Health Res Perspect 2021;12:396−402.ArticlePubMedPMCPDF
- 12. Shimabukuro TT, Cole M, Su JR. Reports of anaphylaxis after receipt of mRNA COVID-19 vaccines in the US-December 14, 2020-January 18, 2021. JAMA 2021;325:1101−2.ArticlePubMedPMC
- 13. Ling RR, Ramanathan K, Tan FL, et al. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med 2022;Apr 11 [Epub]. https://doi.org/10.1016/S2213-2600(22)00059-5.Article
- 14. Snapiri O, Rosenberg Danziger C, Shirman N, et al. Transient cardiac injury in adolescents receiving the BNT162b2 mRNA COVID-19 vaccine. Pediatr Infect Dis J 2021;40:e360−3.ArticlePubMedPMC
- 15. Minocha PK, Better D, Singh RK, et al. Recurrence of acute myocarditis temporally associated with receipt of the mRNA coronavirus disease 2019 (COVID-19) vaccine in a male adolescent. J Pediatr 2021;238:321−3.ArticlePubMedPMC
- 16. McLean K, Johnson TJ. Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: a case report. Acad Emerg Med 2021;28:918−21.ArticlePubMedPMCPDF
- 17. Marshall M, Ferguson ID, Lewis P, et al. Symptomatic acute myocarditis in 7 adolescents after Pfizer-BioNTech COVID-19 vaccination. Pediatrics 2021;148:e2021052478.ArticlePubMedPDF
- 18. Schauer J, Buddhe S, Colyer J, et al. Myopericarditis after the Pfizer messenger ribonucleic acid coronavirus disease vaccine in adolescents. J Pediatr 2021;238:317−20.ArticlePubMedPMC
- 19. Wise J. Covid-19: should we be worried about reports of myocarditis and pericarditis after mRNA vaccines? BMJ 2021;373:n1635.
- 20. Gargano JW, Wallace M, Hadler SC, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the advisory committee on immunization practices - United States, June 2021. MMWR Morb Mortal Wkly Rep 2021;70:977−82.ArticlePubMedPMC
- 21. Saxena S, Skirrow H, Wighton K. Should the UK vaccinate children and adolescents against covid-19? BMJ 2021;374:n1866.
- 22. Centers for Disease Control and Prevention (CDC). COVID-19: myocarditis and pericarditis after mRNA COVID-19 vaccination [Internet]. Atlanta, GA: CDC; 2021 [cited 2022 Feb 24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html.
- 23. Lv M, Luo X, Shen Q, et al. Safety, immunogenicity, and efficacy of COVID-19 vaccines in children and adolescents: a systematic review. Vaccines (Basel) 2021;9:1102. ArticlePubMedPMC
- 24. Ryan M, Montgomery J. Myopericarditis after COVID-19 vaccination: unexpected but not unprecedented. Lancet Respir Med 2022;Apr 11 [Epub]. https://doi.org/10.1016/S2213-2600(22)00091-1.Article
Citations
Citations to this article as recorded by

- Suspected Myocarditis after mRNA COVID-19 Vaccination among South Korean Adolescents
Mi Jin Kim, Jin Hee Kim, Hyun Ok Jun, Kyung Min Kim, Min Sub Jeung, Jun Sung Park
Journal of Pediatric Infectious Diseases.2024; 19(02): 075. CrossRef - Characterization of Brighton Collaboration criteria for myocarditis and pericarditis following COVID-19 vaccine in Korean adolescents
Jue Seong Lee, HyoSug Choi, Seung Hwan Shin, Myung-Jae Hwang, Sara Na, Jong Hee Kim, Sangshin Park, Yoonsun Yoon, Hyun Mi Kang, Bin Ahn, Kyoungsan Seo, Young June Choe
Vaccine.2024;[Epub] CrossRef - Immunogenicity, effectiveness, and safety of COVID-19 vaccines among children and adolescents aged 2–18 years: an updated systematic review and meta-analysis
Peng Gao, Liang-Yu Kang, Jue Liu, Min Liu
World Journal of Pediatrics.2023; 19(11): 1041. CrossRef - Incidence of myopericarditis after mRNA COVID-19 vaccination: A meta-analysis with focus on adolescents aged 12–17 years
Bao-Qiang Guo, Hong-Bin Li, Li-Qiang Yang
Vaccine.2023; 41(28): 4067. CrossRef - Safety monitoring of COVID-19 vaccines: February 26, 2021, To June 4, 2022, Republic of Korea
Yeon-Kyeng Lee, Yunhyung Kwon, Yesul Heo, Eun Kyoung Kim, Seung Yun Kim, Hoon Cho, Seontae Kim, Mijeong Ko, Dosang Lim, Soon-Young Seo, Enhi Cho
Clinical and Experimental Pediatrics.2023; 66(10): 415. CrossRef - Risk of Coronavirus Disease 2019 Messenger RNA Vaccination-Associated Myocarditis and Pericarditis – A Systematic Review of Population-Based Data
Yen-Ching Lin, Chia-Hsuin Chang, Wei-Ju Su, Chin-Hui Yang, Jann-Tay Wang
Risk Management and Healthcare Policy.2023; Volume 16: 2085. CrossRef - COVID-19 Vaccination in Korea: Past, Present, and the Way Forward
Eliel Nham, Joon Young Song, Ji Yun Noh, Hee Jin Cheong, Woo Joo Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef
 , Insob Hwang1
, Insob Hwang1 , Mijeong Ko1
, Mijeong Ko1 , Yunhyung Kwon1
, Yunhyung Kwon1 , Yeon-Kyeng Lee2
, Yeon-Kyeng Lee2




 PubReader
PubReader Cite
Cite