Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 6(4); 2015 > Article
-
Original Article
Phenotypic Assays to Determine Virulence Factors of UropathogenicEscherichia coli (UPEC) Isolates and their Correlation with Antibiotic Resistance Pattern - Mohsen Tabasia, Mohammad Reza Asadi Karama, Mehri Habibia, Mir Saeed Yekaninejadb, Saeid Bouzaria
-
Osong Public Health and Research Perspectives 2015;6(4):261-268.
DOI: https://doi.org/10.1016/j.phrp.2015.08.002
Published online: August 13, 2015
aDepartment of Molecular Biology, Pasteur Institute of Iran, Tehran, Iran
bDepartment of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
- ∗Corresponding authors. m_asadi12@yahoo.comsaeidbouzari@yahoo.com
- ∗Corresponding authors. m_asadi12@yahoo.comsaeidbouzari@yahoo.com
Copyright © 2015 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC. All rights reserved.
Abstract
-
Objectives
- Urinary tract infection caused by uropathogenic Escherichia coli (UPEC) strains is one of the most important infections in the world. UPEC encode widespread virulence factors closely related with pathogenesis of the bacteria. The purpose of this study was to evaluate the presence of different phenotypic virulence markers in UPEC isolates and determine their correlation with antibiotic resistance pattern.
-
Methods
- UPEC isolates from patients with different clinical symptoms of UTI were collected and screened for biofilm and hemolysin production, mannose resistant, and mannose sensitive hemagglutination (MRHA and MSHA, respectively). In addition, antimicrobial resistance pattern and ESBL-producing isolates were recorded.
-
Results
- Of the 156 UPEC isolates, biofilm and hemolysin formation was seen in 133 (85.3%) and 53 (34%) isolates, respectively. Moreover, 98 (62.8%) and 58 (37.2%) isolates showed the presence of Types 1 fimbriae (MSHA) and P fimbriae (MRHA), respectively. Our results also showed a relationship between biofilm formation in UPEC isolated from acute cystitis patients and recurrent UTI cases. Occurrence of UTI was dramatically correlated with the patients' profiles. We observed that the difference in antimicrobial susceptibilities of the biofilm and nonbiofilm former isolates was statistically significant. The UPEC isolates showed the highest resistance to ampicillin, tetracycline, amoxicillin, and cotrimoxazole. Moreover, 26.9% of isolates were ESBL producers.
-
Conclusion
- This study indicated that there is a relationship between the phenotypic virulence traits of the UPEC isolates, patients' profiles, and antibiotic resistance. Detection of the phenotypic virulence factors could help to improve understanding of pathogenesis of UPEC isolates and better medical intervention.
- Urinary tract infections (UTIs) including cystitis and pyelonephritis are considered to be the second most common type of infections in humans. They account for ∼150–250 million cases globally per year 1, 2. More than 50% of women will have at least one episode of UTI during their lifetime 3, 4. Furthermore, after an initial episode of UTI, women are more likely (20–40%) to get recurrent UTIs 4, 5. UTI patients are classified as either asymptomatic or symptomatic cases. Asymptomatic bacteriuria (ABU) occurs in a small number of healthy individuals and may not need treatment, which makes it different from symptomatic bacteriuria. It often affects pregnant women, with varying prevalence among different populations, depending on factors such as age, sex, sexual activity, and the presence of genitourinary abnormalities 3, 4, 6. Uropathogenic Escherichia coli (UPEC) is the most common cause of urinary tract infections (UTIs) both in community and hospital settings with significant morbidity and mortality worldwide 7, 8, 9. Previous investigations have shown that UPEC strains encode widespread virulence factors closely related to colonization, persistence, and pathogenesis of bacteria in the urinary tract 8, 10. The most important of these factors include adhesins or fimbriae, biofilm formation, and toxins such as hemolysin 8, 10. Fimbriae are categorized serologically by their hemagglutination pattern and receptor specificities as mannose sensitive (MSHA) or mannose resistance hemagglutination (MRHA) 7, 11. Despite the vast subclass of adhesins that have been reported in UPEC, Type I (MSHA) and P (MRHA) are the most common fimbriae found in UPEC strains. They play an important role in binding and invasion to bladder (cystitis) and kidney (pyelonephritis) epithelial cells 12, 13.
- Biofilm of UPEC provides a nutrient-rich environment which promotes growth and persistence of microorganisms at the site of infection, and protects bacteria from antimicrobial substances 1, 14. Moreover, UPEC strains often express and secrete a labile pore-forming toxin known as α- hemolysin production that is mainly associated with more virulent UPEC strains 15, 16.
- Emergence of drug resistance to broad-spectrum beta lactams mediated by extended spectrum beta lactamases (ESBLs) and especially multi-drug resistant (MDR) clonal groups among UPEC strains increase the serious threat to global public health 1, 17. Therefore, to optimize the use of effective antibiotics for appropriate treatment of UTI patients, it is important for physicians to be aware of the etiological agents and antimicrobial resistance trends of UTI pathogens in their geographic area.
- This investigation is aimed to determine the prevalence and correlation of phenotypic virulence traits and antibiotic resistance profile among the UPEC isolated from UTIs, with regard to patients' profiles in Tehran, Iran.
Introduction
- 2.1 Organism collection and identification
- The present study was conducted in the Department of Molecular Biology, Pasteur Institute of Iran, Tehran, Iran. Random samples of 156 clinical isolates of UPEC were collected from urine samples of symptomatic and asymptomatic cases of UTIs with significant counts (≥ 105 CFU/mL) in various hospitals of Tehran, Iran between March 2013 and February 2014. Only patients aged ≥ 20 years who were not on antimicrobial therapy at sample collection or had not taken antibiotic drugs 1 month prior to sampling time, were included in this study. Isolated organisms were identified and characterized on the basis of standard microbiological tests such as Gram staining, catalase, indole, methyl red, voges-proskauer, citrate utilization, motility, fermentation, and utilization of glucose, lactose, and sucrose. All isolates were suspended in 15% glycerol-supplemented Luria-Bertani (LB) medium and preserved frozen at −80°C.
- 2.2 Patient demographics
- Clinical symptoms, infection history, treatment summary, and all of the necessary relevant information from patients were obtained from hospital records, laboratory reports, and interviewing patients.
- 2.3 Biofilm formation assay
- We analyzed the ability of the UPEC isolates to produce the biofilm according to the protocols described by O'Toole and Kolter [18] and Dusane et al [19]. We used the E. coli ATCC 25922 strain as a positive control. Briefly, UPEC isolates were grown in LB broth at 37°C overnight, then the cultures were diluted 1:100 with Tryptic Soy Broth (Merck, Darmstadt, Germany) and incubated in a 96-well polyvinyl chloride (PVC) microtiter plate at room temperature (RT) for 48 hours. Wells were washed thoroughly with double-distilled water (DDW) and 150 μL of 0.1 % (w/v) aqueous solution of crystal violet was added to each well. After 15–20 minutes of incubation at RT, the excess crystal violet dye was washed three times with DDW. Then, 200 μL of 33% acetic acid was added to each well and absorbance was measured at optical density 590 nm (OD590) with an enzyme-linked immunosorbent assay (ELISA) reader. Each assay was performed in triplicate and the mean values of crystal violet absorbance ± SD was calculated for all repetitions of the experiments.
- 2.4 Hemolysin production
- The ability of the UPEC isolates to induce hemolysis on blood agar (Merck) was evaluated to detect the hemolysin producer isolates. The bacteria were inoculated into 5% sheep blood agar and incubated overnight at 37°C. Hemolysin production was detected by the presence of a complete clearing zone of the erythrocytes around the colonies.
- 2.5 Hemagglutination assay (HA)
- UPEC isolates were screened for MRHA and MSHA by using 96-well round bottom plates as described by Hultgren et al [20] and Snyder et al [21]. Approximately, 109 CFU/mL of the UPEC bacteria was serially diluted in phosphate-buffered saline (PBS; pH 7.4) and bacterial suspensions were standardized at OD600 nm of 1.0 and added to the wells. An equal volume of 3% (v/v) solution of guinea pig erythrocytes was added to each well with or without 2% D-mannose (Sigma, St. Louis, MO, USA) and gently mixed with the bacterial suspensions. After incubation at RT for 10 minutes, the hemagglutination results were observed according to the clumping of erythrocytes. Hemagglutination was designated as MRHA when it occurred in the presence of D-mannose and MSHA when it was inhibited by D-mannose. Wells with only the suspension of erythrocytes with or without D-mannose served as negative control and E. coli ATCC 25922 was used as a positive control for MRHA.
- 2.6 Antimicrobial susceptibility patterns
- Antibiotic susceptibility patterns of 20 traditional and conventional antibiotics against UPEC isolates was interpreted as recommended by the Clinical and Laboratory Standards Institute (CLSI) by the disk-diffusion method [22]. The following antibiotics (Mast, Co., Merseyside, UK) were included in this study: piperacillin (100 μg), imipenem (10 μg), neropenem (10 μg), piperacillin–tazobactam (100/10μg), ampicillin–sulbactam (10/10 μg), amikacin (30 μg), cotrimoxazole (25 μg), ciprofloxacin (5 μg), ceftazidime (30 μg), nitrofurantoin (300 μg), gentamicin (10 μg), ceftriaxone (30 μg), nalidixic Acid (30 μg), norfloxacin (10 μg), cefotaxime (30 μg), cefixime (5 μg), cefepime (30 μg), amoxicillin (25 μg), tetracycline (30 μg), and ampicillin (10 μg). Inhibition zone diameter (mm) of each antimicrobial disc was measured, and the isolates were classified as resistant and susceptible. The E. coli ATCC 25922 was used as control strain.
- 2.7 Detection of ESBL producers
- All of the UPEC isolates that were resistant to third-generation cephalosporins (3GCs) by disc diffusion test, ceftazidime (zone diameter of ≤ 22 mm), ceftriaxone (zone diameter of ≤ 25 mm), or cefotaxime (zone diameter of ≤ 27 mm) were selected for confirmation of ESBL production by double disk synergy test (DDST) as described by CLSI guidelines [22]. E. coli ATCC 25922 and Klebsiella pneumoniae ATCC 700603 were used as nonESBL and ESBL producing organisms, respectively.
- 2.8 Statistical analysis
- Data analysis was performed by using SPSS software version 19.0 for windows (IBM, Chicago, IL, USA). Chi-square test, independent sample t test, odd ratio (OR) analysis, two-tailed Fisher's exact tests, and one-way ANOVA analysis test were used to compare the occurrence of phenotypic markers in UPEC and describe the associations of the potential virulence factors with other described factors. A p value < 0.05 was considered as statistical significant.
Materials and methods
- 3.1 Prevalence of UTI in relationship with profiles of patients
- Of the 156 UTI patients, the rate of UTI in females (79.5%) was higher than males (20.5%). The incidence of UTI in female patients with age group of 31–40 years (45.2%) and 51–60 years (29.8%) was highest while the age group 41–50 years had the lowest incidence of UTI (8.9%). Among male patients, the highest prevalence of UTI was observed in the age group of 51–60 years (46.9%) and the lowest was seen in the age group of 31–40 years (12.5%). The prevalence of UTI in relation to other important patients' profiles is shown in Table 1. Our results showed that occurrence of UTI were dramatically correlated with the socioeconomic status, educational level, and sexual activity (Table 1).
- 3.2 Virulence characteristics of UPEC isolates 3.2.1
- On the basis of our investigations, biofilm formation capacity of all UPEC isolates was classified into four groups, strong biofilm producers (17.3%), moderate biofilm producers (18.6%), weakly biofilm producers (49.4%), and nonbiofilm producers (14.7%). 3.2.2
- According to our results, hemolysin production was observed in 34% of the UPEC isolates. The remaining 66% isolates showed no hemolysis. 3.2.3
- The ability of UPEC isolates to cause agglutination of erythrocytes is an indirect evidence of the presence of fimbriae [23]. In the present study, 62.8% and 37.2% isolates showed the presence of Type 1 (MSHA) and P fimbriae (MRHA), respectively.
- 3.3 Antimicrobial resistance profile of UPEC
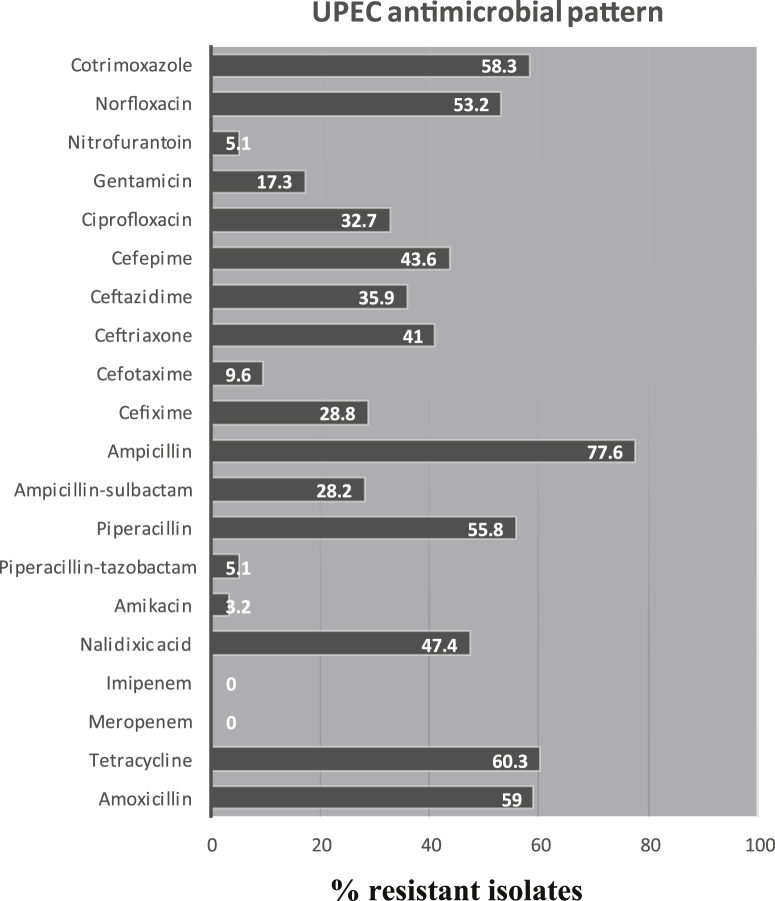
- The resistance pattern of UPEC isolates to the different antimicrobial agents is shown in Fig. 1. Among the antibiotics tested, ampicillin resistance prevalence was the highest (77.6%), followed by tetracycline (60.3%), amoxicillin (59%), cotrimoxazole (58.3%), and piperacillin (55.8%). The isolates showed the highest sensitivity to antibiotics such as imipenem and meropenem (100%), amikacin (96.8%), piperacillin/tazobactum, and nitrofurantion (94.9%). Double disc synergy test (DDST) showed that 26.9% of the UPEC isolates were positive for ESBL production. Totally, 123 isolates tested (79%) were multidrug-resistant (isolates with resistance to three or more different classes of antibiotics).
- 3.4 Relation of antimicrobial resistance with virulence determinants of UPEC and patients' profiles
- According to our results, overall resistance rates of the antibiotics tested among the UPEC isolated from male patients were higher than those of female patients (p = 0.04), although the differences in distribution of antimicrobial resistance in different age groups of UTI patients were not statistically significant (p > 0.05). We also found that overall resistance rates were higher among inpatients isolates compared to outpatients (p = 0.039). Among the isolates, resistance to ampicillin, cefepime, and ceftazidime were significantly more prevalent in inpatients than outpatients (p = 0.037, p = 0.008, and p = 0.047, respectively). There was also a significant correlation between higher levels of resistance to multiple antibiotics such as nalidixic acid (p = 0.038), ceftriaxone (p = 0.041), cotrimoxazole (p = 0.029), and acute cystitis patients compared with the pyelonephritis and asymptomatic bacteriuria patients (Table 2).
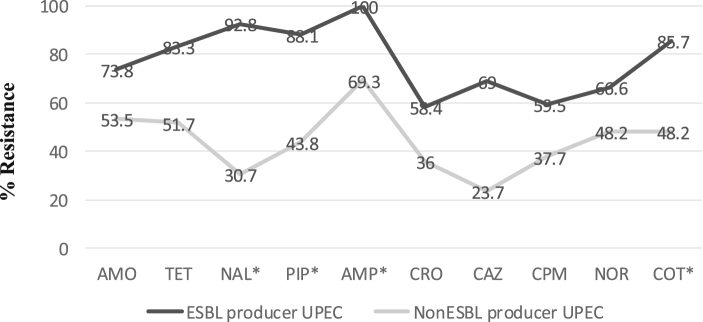
- In addition, our results showed that there was no significant difference between resistance to the antibiotics, other than cotrimoxazole (p = 0.015), and history of recurrent in the UTI patients. Relationship between antimicrobial resistance and phenotypic virulence markers of the UPEC isolates is shown in Table 3. As shown in Table 3, there was a significant correlation between intensity of biofilm formation and resistance to antibiotics such as ampicillin, norfloxacin, and cotrimoxazole (p < 0.05). Moreover, hemolysin producing isolates were significantly less resistant to tetracycline, nalidixic acid, and cotrimoxazole than in nonhemolysin isolates (p < 0.05). No relationship was found between MRHA, MSHA isolates, and resistance to the antibiotics used (p > 0.05). As shown in Fig. 2, although all of the antibiotic resistance occurred at a higher rate among ESBL producer isolates than nonESBL producer isolates, only resistance to nalidixic acid, piperacillin, ampicillin, and cotrimoxazole was statistically significant (p < 0.05).
- 3.5 Phenotypic virulence patterns of UPEC isolates in relation to clinical symptoms
- Based on the distribution of the phenotypic virulence traits, all of the UPEC isolates exhibited 16 virulence patterns, referred to as UPEC patterns (UP) in Table 4. The majority of the isolates shared some similarities in most virulence markers, but several differences were also observed. UP 12 was characterized by the presence of the biofilm and MSHA phenotypic markers only, and was the most common pattern found in 46 isolates. Moreover, some of the UPEC patterns were only observed in single type of clinical symptoms in UTI patients (Table 4). Occurrence of multiple urovirulence markers (isolates with three or more virulence markers) observed in 58 (37.2%) of the UPEC isolates (Table 4). It has been observed that pyelonephritis and cystitis cases were more associated with multiple urovirulence markers compared to asymptomatic bacteriuria cases (p = 0.022 and p = 0.038, respectively; Table 4).
Results
3.2.1 Biofilm formation
3.2.2 Hemolysin production
3.2.3 Prevalence of Type 1 (MSHA) and P fimbriae (MRHA)
- Phenotypic characteristics of UPEC isolates and their correlation with antibiotic resistance patterns in patients with UTI are not well known and few data have been reported in Iran. Identification of virulence markers of UPEC will help to understand their contribution with the antimicrobial resistance 1, 2.
- Our findings in accordance with other studies indicated that females have a notable frequency of UTI versus males 3, 24. This difference in frequency could be due to several clinical factors, including anatomic differences, hormonal effects, and behavioral patterns 3, 24. Moreover, our investigations reveal that overall resistance rates of antimicrobial drugs were higher in men than women (p = 0.04). These observations were similar to the findings of Yilmaz et al [25]. In the current study, most recurrent UTIs in women presented as acute cystitis, as occurred in nonrecurrent women.
- We observed that resistance rates were higher among antimicrobials that have been used for a long time as empirical therapy such as ampicillin and cotrimoxazole. Similar findings were reported in Iran and other countries 2, 26. This may be due to increased consumption of these antibiotics, self-medication, and transfer of resistant isolates [27]. Thus, the use of other antibiotics such as nitrofurantoin and imipenem is recommended for treatment of UTI patients.
- Our results showed that the percentage of nalidixic acid resistant isolates causing acute cystitis is more than those causing acute pyelonephritis and asymptomatic baceriuria (p = 0.038). A similar observation was reported by Velasco et al [28]. These data suggest that the nalidixic acid resistant UPEC isolates may have lost the ability to attach the kidney epithelial cells. Moreover, UPEC isolates that produced hemolysin or biofilm were less resistant to nalidixic acid than in nonhemolysis (p = 0.011) and nonbiofilm formers (p = 0.043). These findings in accordance with other studies suggest that resistance to nalidixic acid may be associated with marked reduction in the virulence severity of UPEC isolates 29, 30, 31. Also, this is in accordance with the observation of Johnson et al [32] that UPEC strains with greater antibiotic resistance tended to express lower virulence traits.
- The present study showed that hemolysin producer isolates had a higher ability of biofilm formation. This finding is similar to the study of Soto et al [29] and in contrary to observations of Marhova et al [33].
- According to our results, some urovirulence markers were closely associated with a specific anatomical site of infection. In this regard, we observed that hemolysin production is more frequent in UPEC isolated from patients with pyelonephritis than in isolates from patients with other clinical symptoms of UTI (p = 0.01). This finding reveals that hemolysin may be contributing to the severity of UPEC infections. Moreover, our results showed a higher potency of biofilm production among UPEC isolates causing acute cystitis than isolates from acute pyelonephritis and, in particular, those causing asymptomatic bacteriuria (p = 0.04). In fact, biofilm formation seems to be one of the most important virulence factors among the UPEC isolated from patients with acute cystitis. Also, these biofilm producing UPEC isolates showed a significantly greater expression of Type 1 fimbriae (MSHA) than nonbiofilm producing isolates (p = 0.021). This could be explained by the important role of Type 1 fimbriae in the first steps of biofilm formation [12]. One-way analysis of variance indicated that the difference in antimicrobial susceptibilities of the biofilm and nonbiofilm producing isolates was statistically significant (p < 0.05). Murugan et al [34] have reported the correlation between biofilm formation and multiple drug resistance among UPEC strains. We also found a remarkable correlation between biofilm and ESBL producing UPEC.
- In this study, production of MRHA and MSHA was in relation to clinical symptoms of UTI patients. MRHA isolates were significantly higher among the UPEC isolated from pyelonephritis patients (p = 0.025), whereas MSHA isolates were more prevalent in patients with cystitis and asymptomatic bacteriuria (p < 0.05). Association of P fimbriae (MRSA) of UPEC with acute pyelonephritis in UTI patients suggests that P fimbriae are required for colonization and invasion of the human upper urinary tract 35, 36.
- Our results showed that UPEC isolated from patients with symptomatic bacteriuria are characterized by higher virulence characteristics than those isolated from patients with asymptomatic UTI (Table 4). This observation reflects the important role of virulence factors of UPEC in severity of clinical symptoms of UTI patients.
- In our study, biofilm producing UPEC isolates were strongly linked to recurrent UTI (p = 0.001). These data suggest that the tropism of UPEC isolates for the recurrent infections may depend on the biofilm formation.
- In conclusion, the present study provides novel epidemiological information relevant to the UPEC isolated from UTI patients. These findings indicate that there is a correlation between the most important phenotypic virulence traits of the UPEC isolates and antibiotic resistance. Also, we believe that detection of the phenotypic virulence factors could be valuable in investigations on the pathogenesis of UPEC isolates and management of UTI therapy. However, further studies of genotypic and phenotypic characteristics of UPEC isolates may help us to get novel insights into pathogenesis of UPEC isolates.
Discussion
- There is no conflict of interest.
Conflicts of interest
-
Acknowledgements
- This article is part of the work by Mohsen Tabasi to fulfill the requirement for a Master of Science. This work was financially supported by Pasteur Institute of Iran.
Acknowledgments
-
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License (http://creativecommons.org/licenses/by-nc-nd/4.0) which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
Article information
- 1. Ponnusamy P., Nagappan R.. Extended spectrum beta-lactamase, biofilm-producing uropathogenic pathogens and their antibiotic susceptibility patterns from urinary tract infection-an overview. Int J Microbiol Res 4(2). 2013 Jan;101−118.
- 2. Asadi S., Kargar M., Solhjoo K.. The association of virulence determinants of uropathogenic escherichia coli with antibiotic resistance. Jundishapur J Microb 7(5). 2014 May;1−5.
- 3. Miller II O., Hemphill R.R.. Urinary tract infection and pyelonephritis. Emerg Med Clin N Am 19(3). 2001 Aug;655−674.Article
- 4.
- 5. Kodner C.M., Thomas Gupton E.K.. Recurrent urinary tract infections in women: diagnosis and management. Am Fam Physician 82(6). 2010 Sep;638PMID: 20842992.PubMed
- 6. Nicolle L.E., Bradley S., Colgan R.. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005 Mar;643−654. PMID: 15714408.ArticlePubMed
- 7. Davis N.F., Flood H.D.. The pathogenesis of urinary tract infections. Clinical management of complicated urinary tract infection. 2011. InTech; pp 101−120.
- 8. Slavchev G., Pisareva E., Markova N.. Virulence of uropathogenic Escherichia coli. 2013 Oct.
- 9. Bien J., Sokolova O., Bozko P.. Role of uropathogenic Escherichia coli virulence factors in development of urinary tract infection and kidney damage. Int J Nephrol 2012:2012 Mar;1−15.ArticlePDF
- 10. Dhakal B., Kulesus R., Mulvey M.. Mechanisms and consequences of bladder cell invasion by uropathogenic Escherichia coli. Eur J Clin Invest 38(s2). 2008 Oct;2−11. PMID: 18616559.ArticlePubMed
- 11. Blumenstock E., Jann K.. Adhesion of piliated Escherichia coli strains to phagocytes: differences between bacteria with mannose-sensitive pili and those with mannose-resistant pili. Infect Immun 35(1). 1982 Jan;264−269. PMID: 6119294.ArticlePubMed
- 12. Ulett G.C., Mabbett A.N., Fung K.C.. The role of F9 fimbriae of uropathogenic Escherichia coli in biofilm formation. Microbiology 153(7). 2007 Jul;2321−2331. PMID: 17600076.ArticlePubMed
- 13. Wullt B., Bergsten G., Connell H.. P fimbriae enhance the early establishment of Escherichia coli in the human urinary tract. Mol Microbiol 38(3). 2000 Nov;456−464. PMID: 11069670.ArticlePubMed
- 14. Hancock V., Dahl M., Klemm P.. Abolition of biofilm formation in urinary tract Escherichia coli and Klebsiella isolates by metal interference through competition for fur. Appl Environ Microbiol 76(12). 2010 Jun;3836−3841. PMID: 20418434.ArticlePubMed
- 15. Laura B., Sabina M., Romina V.. E. coli alpha hemolysin and properties. Biochemistry 4:2012 Jan;107−140.Article
- 16. Justice S.S., Hunstad D.A.. UPEC hemolysin: more than just for making holes. Cell Host Microbe 11(1). 2012 Jan;4−5. PMID: 22264508.ArticlePubMed
- 17. Hilbert D.W.. Antibiotic resistance in urinary tract infections: current issues and future solutions. Urinary tract infections. 2011. InTech; Rijeka: pp 194−206.
- 18. O'Toole G.A., Kolter R.. Initiation of biofilm formation in Pseudomonas fluorescens WCS365 proceeds via multiple, convergent signalling pathways: a genetic analysis. Mol Microbiol 28(3). 1998 May;449−461. PMID: 9632250.ArticlePubMed
- 19. Dusane D., Rajput J., Kumar A.. Disruption of fungal and bacterial biofilms by lauroyl glucose. Lett Appl Microbiol 47(5). 2008 Nov;374−379. PMID: 19146524.ArticlePubMed
- 20. Hultgren S.J., Porter T.N., Schaeffer A.J.. Role of type 1 pili and effects of phase variation on lower urinary tract infections produced by Escherichia coli. Infect Immun 50(2). 1985 Nov;370−377. PMID: 2865209.ArticlePubMed
- 21. Snyder J.A., Haugen B.J., Lockatell C.V.. Coordinate expression of fimbriae in uropathogenic Escherichia coli. Infect Immun 73(11). 2005 Nov;7588−7596. PMID: 16239562.ArticlePubMed
- 22. Clinical and Laboratory Standards Institute . Performance standards for antimicrobial disc diffusion tests approved standards. 9th ed.2006. Wayne.
- 23. Hogan J., Todhunter D., Smith K.. Hemagglutination and hemolysis by Escherichia coli Isolated from bovine intramammary infections. J Dairy Sci 73(11). 1990 Nov;3126−3131. PMID: 2273142.ArticlePubMed
- 24. Foxman B.. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 113(1). 2002 Jul;5−13.Article
- 25. Yilmaz N., Agus N., Yurtsever S.G.. Prevalence and antimicrobial susceptibility of Escherichia coli in outpatient urinary isolates in Izmir, Turkey. Med Sci Monit 15(11). 2009 Nov;65.
- 26. Farshad S., Japoni A., Hosseini M.. Low distribution of integrons among multidrug resistant E. coli strains isolated from children with community-acquired urinary tract infections in Shiraz, Iran. Iran Pol J Microbiol 57(3). 2008 Jul;193−198. PMID: 19004239.PubMed
- 27. Byarugaba D.. Antimicrobial resistance in developing countries and responsible risk factors. Int J Antimicrob Agents 24(2). 2004 Aug;105−110. PMID: 15288307.ArticlePubMed
- 28. Velasco M., Horcajada J.P., Mensa J.. Decreased invasive capacity of quinolone-resistant Escherichia coli in patients with urinary tract infections. Clin Infec Dis 33(10). 2001 Oct;1682−1686. PMID: 11595990.Article
- 29. Soto S.M., Smithson A., Martinez J.. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J Urol 177(1). 2007 Jan;365−368. PMID: 17162092.ArticlePubMed
- 30. Da Silva G.J., Mendonça N.. Association between antimicrobial resistance and virulence in Escherichia coli. Virulence 3(1). 2012 Jan–Feb;18−28. PMID: 22286707.ArticlePubMed
- 31. Kawamura-Sato K., Yoshida R., Shibayama K.. Virulence genes, quinolone and fluoroquinolone resistance, and phylogenetic background of uropathogenic Escherichia coli strains isolated in Japan. Jpn J Infec Dis 63(2). 2010 Mar;113−115. PMID: 20332573.
- 32. Johnson J.R., Kuskowski M.A., Gajewski A.. Virulence characteristics and phylogenetic background of multidrug-resistant and antimicrobial-susceptible clinical isolates of Escherichia coli from across the United States, 2000–2001. J Infect Dis 190(10). 2004 Nov;1739−1744. PMID: 15499527.ArticlePubMed
- 33. Marhova M., Kostadinova S., Stoitsova S.. Biofilm-forming capabilities of urinary Escherichia coli isolates. Biotechnol Biotec Eq 24(Suppl. 1). 2010;589−593.Article
- 34. Murugan S., Devi P.U., John P.N.. Antimicrobial susceptibility pattern of biofilm producing Escherichia coli of urinary tract infections. Curr Res Bacteriol 4(2). 2011;73−80.Article
- 35. Johnson J.R.. Virulence factors in Escherichia coli urinary tract infection. Clin Microbiol Rev 4(1). 1991 Jan;80−128. PMID: 1672263.ArticlePubMed
- 36. Hull R.A., Rudy D.C., Wieser I.E.. Virulence factors of Escherichia coli isolates from patients with symptomatic and asymptomatic bacteriuria and neuropathic bladders due to spinal cord and brain injuries. J Clin Microbiol 36(1). 1998 Jan;115−117. PMID: 9431932.ArticlePubMed
References
* Significant at p < 0.05.
ABU = asymptomatic bacteriuria; AMO = amoxicillin; AMP = ampicillin; CAZ = ceftazidime; COT = cotrimoxazole; CPM = cefepime; CRO = ceftriaxone; NAL = nalidixic acid; NOR = norfloxacin; NS = not significant; PIP = piperacillin; TET = tetracycline; %R = percentage of resistance to antimicrobial agents.
* Significant at p < 0.05.
AMO = amoxicillin; AMP = ampicillin; CAZ = ceftazidime; COT = cotrimoxazole; CPM = cefepime; CRO = ceftriaxone; HA = hemagglutination; MRHA = mannose resistant hemagglutination; MSHA = mannose sensitive hemagglutination; NAL = nalidixic acid; NOR = norfloxacin; NS = not significant; PIP = piperacillin; TET = tetracycline; UPEC = uropathogenic Escherichia coli; %R = percentage of resistance to antimicrobial agents.
Figure & Data
References
Citations

- Multi-drug-resistant Escherichia coli in adult male patients with enlarged prostate attending general hospitals in Benue state
Cornelius Iwodi, Grace M. Gberikon, Innocent Okonkwo Ogbonna, Emmanuel O. Agada
Brazilian Journal of Microbiology.2024; 55(1): 447. CrossRef - Phylogenetic analysis, biofilm formation, antimicrobial resistance and relationship between these characteristics in Uropathogenic Escherichia coli
Talieh Mostaghimi, Abazar Pournajaf, Ali Bijani, Mohsen Mohammadi, Mehdi Rajabnia, Mehrdad Halaji
Molecular Biology Reports.2024;[Epub] CrossRef - Type 1 fimbrial phase variation in multidrug-resistant asymptomatic uropathogenic Escherichia coli clinical isolates upon adherence to HTB-4 cells
Arunita Ghosh, Mandira Mukherjee
Folia Microbiologica.2024;[Epub] CrossRef - The Characteristics of Extended-Spectrum β-Lactamases (ESBLs)-Producing Escherichia coli in Bloodstream Infection
Rongrong Li, Huaming Xu, Hao Tang, Jilu Shen, Yuanhong Xu
Infection and Drug Resistance.2023; Volume 16: 2043. CrossRef - Phenotypic Detection of Virulence Factors of Uropathogenic Enterobacteriaceae
Betu Rama Soujanya, G.S. Banashankari
Journal of Pure and Applied Microbiology.2023; 17(2): 931. CrossRef - Uropathogenic bacteria and deductive genomics towards antimicrobial resistance, virulence, and potential drug targets
Aaima Amin, Ramisha Noureen, Ayesha Iftikhar, Annam Hussain, Wadi B. Alonazi, Hafiz Muhammad Zeeshan Raza, Ifra Ferheen, Muhammad Ibrahim
International Microbiology.2023; 27(1): 325. CrossRef - Regarding the prospects of using Lactobacillus-based probiotics, D-mannose and cranberry extracts in therapy of urinary tract infections
O. A. Gromova, I. Yu. Torshin
Obstetrics, Gynecology and Reproduction.2023; 17(4): 485. CrossRef - The Impact of Gold Nanoparticle Susceptibility on Drug Resistance Phenotypes in Uropathogenic Escherichia coli
Iman Hosseinpour, Leila Fozouni, Morteza Khademi, Mehdi Movaghari, Mohammad Mehdi Akhoondi
Journal of Medical Microbiology and Infectious Dis.2023; 11(3): 155. CrossRef - Biofilm Formation by Escherichia coli Isolated from Urinary Tract Infections from Aguascalientes, Mexico
Flor Yazmín Ramírez Castillo, Alma Lilian Guerrero Barrera, Josée Harel, Francisco Javier Avelar González, Philippe Vogeleer, José Manuel Arreola Guerra, Mario González Gámez
Microorganisms.2023; 11(12): 2858. CrossRef - Detection of Adhesion Encoding Genes, Antibacterial Susceptibility Test and Biofilm Formation of Uropathogenic Escherichia coli Isolated from Urinary Tract Infections in Children
Rezvan Goodarzi, Rasoul Yousefimashouf, Iraj Sedighi, Abbas Moradi, Fatemeh Nouri, Mohammad Taheri
Journal of Advances in Medical and Biomedical Rese.2022; 30(1): 1. CrossRef - A global systematic review and meta-analysis on correlation between biofilm producers and non-biofilm producers with antibiotic resistance in Uropathogenic Escherichia coli
Mitra Garousi, Sina Monazami Tabar, Hosein Mirazi, Parnia Asgari, Paniz Sabeghi, Astireh Salehi, Azad Khaledi, Mohammad Ghenaat Pisheh Sanani, Hossein Karballaei Mirzahosseini
Microbial Pathogenesis.2022; 164: 105412. CrossRef - Antibiotic resistance, phylogenetic typing, and virulence genes profile analysis of uropathogenic Escherichia coli isolated from patients in southern Iraq
Mohammed Allami, Masoumeh Bahreini, Mohammad Reza Sharifmoghadam
Journal of Applied Genetics.2022; 63(2): 401. CrossRef - Phylogenetic Group Distribution of Uropathogenic Escherichia coli and Related Antimicrobial Resistance Pattern: A Meta-Analysis and Systematic Review
Mehrdad Halaji, Amirhossein Fayyazi, Mehdi Rajabnia, Donya Zare, Abazar Pournajaf, Reza Ranjbar
Frontiers in Cellular and Infection Microbiology.2022;[Epub] CrossRef - Genotypic assay to determine some virulence factors of Uropathogenic E. coli (UPEC) isolates
Tsahel H. Al-Dulaimi, Ilham A Bunyan, Thikra A. Banimuslem
International journal of health sciences.2022; : 1593. CrossRef - Demonstrating the utility of Escherichia coli asymptomatic bacteriuria isolates’ virulence profile towards diagnosis and management—A preliminary analysis
Lalitha Maniam, Kumutha Malar Vellasamy, Hassan Mahmood Jindal, Vallikannu Narayanan, Mahmoud Danaee, Jamuna Vadivelu, Vinod Pallath, Abdelazeem Mohamed Algammal
PLOS ONE.2022; 17(5): e0267296. CrossRef - Urine Microscopy Score and Neutrophil Lymphocyte Ratio at Presentation are Good Biomarkers of Acute Kidney Injury in Patients with Upper Urinary Tract Infection when Assessed in Correlation with Virulence Factors of Escherichia coli and Blood Group Secret
Shanmugapriya Thiagarajan, Selvaraj Stephen, Santosh Kumar, Priscilla Charles, Sarangapani Kanagamuthu, Stanley Ambroise, Pragasam Viswanathan, Palanivel Chinnakali, Rajesh Nachiappa Ganesh
Journal of Pure and Applied Microbiology.2022; 16(2): 1074. CrossRef - Association between Virulence Factors and Antimicrobial Resistance of Klebsiella pneumoniae Clinical Isolates from North Kerala
Ramya Kumaran, R.V. Geetha, Sabitha Baby
Journal of Pure and Applied Microbiology.2022; 16(2): 867. CrossRef - Molecular Characterization and Mutational Analysis of Fluoroquinolones and Tetracycline Resistant Genes of Escherichia coli Isolated from UTI Patients
Sadiq Azam, Nauman Khan, Noor Rehman, Ibrar khan, Amjad Ali, Muhammad Asghar, Azam Hayat, Gulesehra Mujib, Anila Farid
Brazilian Archives of Biology and Technology.2022;[Epub] CrossRef - Antimicrobial Susceptibility Patterns of Escherichia coli from Urine Isolates
Taher I. Mahmod Shailabi, Osama H. Aldeeb, Abdullah F. Almaedani, Elham O. Borwis, Samar A. Amer
Al-Mukhtar Journal of Sciences.2022; 37(4): 372. CrossRef - Possible Relationship of Novel Phylogenetic Structure With Antimicrobial Resistance, Biofilm Formation, and Hemolytic Activity in Uropathogenic Escherichia coli (UPEC)
Batoul Rahimifard, Vahid Soheili, Gholamreza Hashemitabar, Mahdi Askari Badouei
International Journal of Enteric Pathogens.2022; 10(3): 98. CrossRef - Virulence genes and phylogenetic groups of uropathogenic Escherichia coli isolates from patients with urinary tract infection and uninfected control subjects: a case-control study
Seyedeh Elham Rezatofighi, Mahsa Mirzarazi, Mansour Salehi
BMC Infectious Diseases.2021;[Epub] CrossRef - Virulence factors and antimicrobial resistance of uropathogenic Escherichia coli (UPEC) isolated from urinary tract infections: a systematic review and meta-analysis
Gabriel Kambale Bunduki, Eva Heinz, Vincent Samuel Phiri, Patrick Noah, Nicholas Feasey, Janelisa Musaya
BMC Infectious Diseases.2021;[Epub] CrossRef - Evaluation of Biofilm Formation and Virulence Genes and Association with Antibiotic Resistance Patterns of Uropathogenic Escherichia coli Strains in Southwestern Iran
Mostafa Boroumand, Asghar Sharifi, Mohammad Amin Ghatei, Mohsen Sadrinasab
Jundishapur Journal of Microbiology.2021;[Epub] CrossRef - The urobiome, urinary tract infections, and the need for alternative therapeutics
Jennifer Jones, Craig P. Murphy, Roy D. Sleator, Eamonn P. Culligan
Microbial Pathogenesis.2021; 161: 105295. CrossRef - Clinical cases, drug resistance, and virulence genes profiling in Uropathogenic Escherichia coli
Ali Hozzari, Payam Behzadi, Parisa Kerishchi Khiabani, Mohammad Sholeh, Niloofar Sabokroo
Journal of Applied Genetics.2020; 61(2): 265. CrossRef Prevalence of Virulence Genes and Their Association with Antimicrobial Resistance Among Pathogenic E. coli Isolated from Egyptian Patients with Different Clinical Infections
Rehab Mahmoud Abd El-Baky, Reham Ali Ibrahim, Doaa Safwat Mohamed, Eman Farouk Ahmed, Zeinab Shawky Hashem
Infection and Drug Resistance.2020; Volume 13: 1221. CrossRefIn-vitro Investigation of Antibiotics Efficacy Against Uropathogenic Escherichia coli Biofilms and Antibiotic Induced Biofilm Formation at Sub-Minimum Inhibitory Concentration of Ciprofloxacin
Zara Rafaque, Nasira Abid, Nida Liaquat, Pashmina Afridi, Saima Siddique, Safia Masood, Sehrish Kanwal, Javid Iqbal Dasti
Infection and Drug Resistance.2020; Volume 13: 2801. CrossRef- Relationship between Virulence and Resistance among Gram-Negative Bacteria
Virginio Cepas, Sara M. Soto
Antibiotics.2020; 9(10): 719. CrossRef - In Vitro and In Vivo Biological Activity of Berberine Chloride against Uropathogenic E. coli Strains Using Galleria mellonella as a Host Model
Giulio Petronio Petronio, Marco Alfio Cutuli, Irene Magnifico, Noemi Venditti, Laura Pietrangelo, Franca Vergalito, Antonella Pane, Giovanni Scapagnini, Roberto Di Marco
Molecules.2020; 25(21): 5010. CrossRef - Study of virulence factors and antibiotic susceptibility pattern of extraintestinal pathogenic Escherichia coli
Mahendraswamy B Hiremath, R Lava
Indian Journal of Microbiology Research.2020; 7(4): 330. CrossRef - Virulence factors of uropathogenic Escherichia coli (UPEC) and correlation with antimicrobial resistance
Chhaya Shah, Ratna Baral, Bijay Bartaula, Lok Bahadur Shrestha
BMC Microbiology.2019;[Epub] CrossRef - Outcome of acute urinary tract infections caused by uropathogenic Escherichia coli with phenotypically demonstrable virulence factors
Unnimaya Pullanhi, Sadia Khan, Vivek Vinod, Karthika Mohan, Anil Kumar
Annals of African Medicine.2019; 18(3): 138. CrossRef - Urinary tract infection: Pathogenicity, antibiotic resistance and development of effective vaccines against Uropathogenic Escherichia coli
Mohammad Reza Asadi Karam, Mehri Habibi, Saeid Bouzari
Molecular Immunology.2019; 108: 56. CrossRef - Systematic analysis of research on D-mannose and the prospects for its use in recurrent infections of the urinary tract in women of reproductive age
O. A. Gromova, I. Yu. Torshin, N. K. Tetruashvili
Obstetrics, Gynecology and Reproduction.2019; 13(2): 119. CrossRef - Evaluation of pap and sfa Genes Relative Frequency P and S Fimbriae Encoding of Uropathogenic Escherichia coli Isolated from Hospitals and Medical Laboratories; Yasuj City, Southwest Iran
Mostafa Boroumand, Asghar Sharifi, Leila Manzouri, Seyed Sajjad Khoramrooz, Seyed Abdolmajid Khosravani
Iranian Red Crescent Medical Journal.2019;[Epub] CrossRef - Extended spectrum β-lactamase producing uropathogenic Escherichia coli and the correlation of biofilm with antibiotics resistance in Nepal
Raju Shrestha, Santosh Khanal, Pramod Poudel, Karan Khadayat, Sajani Ghaju, Anita Bhandari, Sunil Lekhak, Narayan Dutt Pant, Manisha Sharma, Bishnu P. Marasini
Annals of Clinical Microbiology and Antimicrobials.2019;[Epub] CrossRef - Genotyping and Molecular Characterization of Extended-Spectrum Beta-Lactamases-Producing Uropathogenic Escherichia Coli in and Around Coimbatore District, Tamil Nadu, India
Mylsamy Muraleetharan, Thirumoorthy Viswanathan
Urological Science.2019; 30(6): 244. CrossRef - Investigation of P Fimbriae Presence in Escherichia coli Strains Isolated from Urine Samples in Human, and Their Antibacterial Resistance
Emel Inegol Paykoc, Suheyla Turkyilmaz
Jundishapur Journal of Microbiology.2018;[Epub] CrossRef - An evaluation of multidrug-resistant Escherichia coli isolates in urinary tract infections from Aguascalientes, Mexico: cross-sectional study
Flor Y. Ramírez-Castillo, Adriana C. Moreno-Flores, Francisco J. Avelar-González, Francisco Márquez-Díaz, Josée Harel, Alma L. Guerrero-Barrera
Annals of Clinical Microbiology and Antimicrobials.2018;[Epub] CrossRef - Potential Mechanisms Underlying the Increased Excitability of the Bladder Afferent Pathways in Interstitial Cystitis/Bladder Pain Syndrome
Doo Sang Kim
Urogenital Tract Infection.2018; 13(2): 26. CrossRef - Distribution of virulence genes and their association with antimicrobial resistance among uropathogenic Escherichia coli isolates from Iranian patients
Yalda Malekzadegan, Reza Khashei, Hadi Sedigh Ebrahim-Saraie, Zahra Jahanabadi
BMC Infectious Diseases.2018;[Epub] CrossRef - Important Virulence Factors and Related Genes in Uropathogenic E. coli and their Relation to Fluoroquinolone Resistance
Noha Mohammad Gohar, Hanaa Fathy Aly, Magda Ibrahim Ayoub
Journal of Pure and Applied Microbiology.2018; 12(3): 1393. CrossRef - Clonal and Virulence Distribution of UropathogenicEscherichia coliIsolated from Children in Korea
Dong Ho Kim, Chul Hee Choi
Journal of Bacteriology and Virology.2017; 47(1): 54. CrossRef - An Epidemiological Study on the Prevalence and Antibiotic Resistance Patterns of Bacteria Isolated from Urinary Tract Infections in Central Iran
Fahimeh Ghanbari, Farzad Khademi, Shirin Saberianpour, Mojtaba Shahin, Nafiseh Ghanbari, Kourosh Naderi, Tahereh Motalebi-Rad
Avicenna Journal of Clinical Microbiology and Infe.2017; 4(3): 42214. CrossRef - Correlation Between hlyA and cnf1 Virulent Genes with Antibiotic Resistance and non-ESBLs Escherichia coli Isolates Collected from Patient with Urinary Tract Infections in Kerman, Iran
Zahra Hashemizadeh, Davood Kalantar-Neyestanaki, Shahla Mansouri
Archives of Pediatric Infectious Diseases.2017;[Epub] CrossRef - Prevalence and Antibiotic Resistance Profile of Enterobacteria Involved in Urinary Infections in Bamako, Mali
Amadou Hamadoun Babana
MOJ Biology and Medicine.2017;[Epub] CrossRef - Phenotypic and Molecular Characterization of some Virulence Factors in Multidrug Resistance Escherichia coli Isolated from Different Clinical Infections in Iraq
Ahmed Abduljabbar Ja Aljanaby, Qassim Mmuhsin Hashi Alfaham
American Journal of Biochemistry and Molecular Bio.2017; 7(2): 65. CrossRef - Emerging nanotechnology based strategies for diagnosis and therapeutics of urinary tract infections: A review
M.S. Kumar, A.P. Das
Advances in Colloid and Interface Science.2017; 249: 53. CrossRef - Effects of single and combined use of bacteriophages and antibiotics to inactivate Escherichia coli
Nádia Valério, Cristiana Oliveira, Vânia Jesus, Tatiana Branco, Carla Pereira, Catarina Moreirinha, Adelaide Almeida
Virus Research.2017; 240: 8. CrossRef - Crystal Structures of Acyclic Nucleoside Phosphonates in Complex with Escherichia coli Hypoxanthine Phosphoribosyltransferase
Wai Soon Eng, Dana Hocková, Petr Špaček, Ondřej Baszczyňski, Zlatko Janeba, Lieve Naesens, Dianne T. Keough, Luke W. Guddat
ChemistrySelect.2016; 1(19): 6267. CrossRef


 PubReader
PubReader Cite
Cite
