Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 10(3); 2019 > Article
-
Original Article
Comparison of Purgative Manna Drop and Phototherapy with Phototherapy Treatment of Neonatal Jaundice: A Randomized Double-Blind Clinical Trial - Amirreza Monsef, Fatemeh Eghbalian, Neda Rahimi
-
Osong Public Health and Research Perspectives 2019;10(3):152-157.
DOI: https://doi.org/10.24171/j.phrp.2019.10.3.06
Published online: June 30, 2019
Pediatric Department, Hamadan University of Medical Sciences, Hamadan, Iran
- *Corresponding author: Fatemeh Eghbalian, Pediatric Department, Hamadan University of Medical Sciences, Hamadan, Iran, E-mail: fatemeh.eghbalian.hums@gmail.com; eghbalian_fa@yahoo.com
• Received: December 28, 2019 • Revised: April 23, 2019 • Accepted: May 22, 2019
Copyright ©2019, Korea Centers for Disease Control and Prevention
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
This article has been corrected. See "Corrigendum to “Comparison of Purgative Manna Drop and Phototherapy with Phototherapy Treatment of Neonatal Jaundice: A Randomized Double-Blind Clinical Trial” [Osong Public Health Res Perspect 2019;10(3):152–7]" in Volume 11 on page 265.
Abstract
-
Objectives
- Herbal remedies such as purgative manna are used to treat neonatal jaundice. In this study Bilineaster drop (purgative manna) and phototherapy, and phototherapy treatment alone were compared by assessing phototherapy duration and number of days in hospital.
-
Methods
- There were 150 consecutive term neonates with jaundice, weighting from 2,500 g to 4,000 g enrolled in this randomized double blind clinical trial. The neonates were randomly assigned to intervention and control groups. The control patients received only phototherapy and the intervention group underwent phototherapy treatment and purgative manna drop (5 drops per kg of body weight, 3 times a day). Direct and total measurements of bilirubin concentration in the serum were measured and the reduction in concentration of bilirubin was calculated.
-
Results
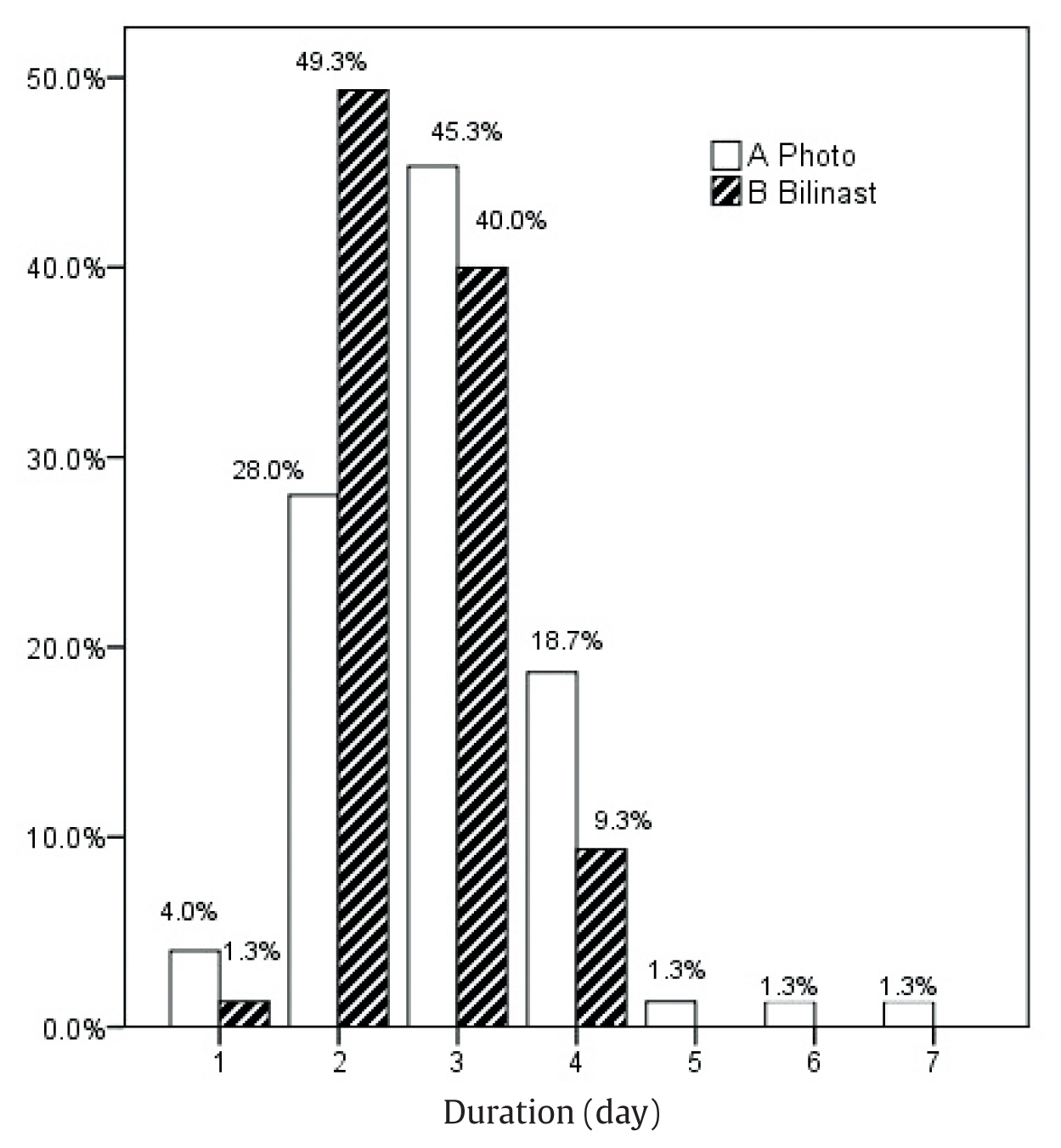
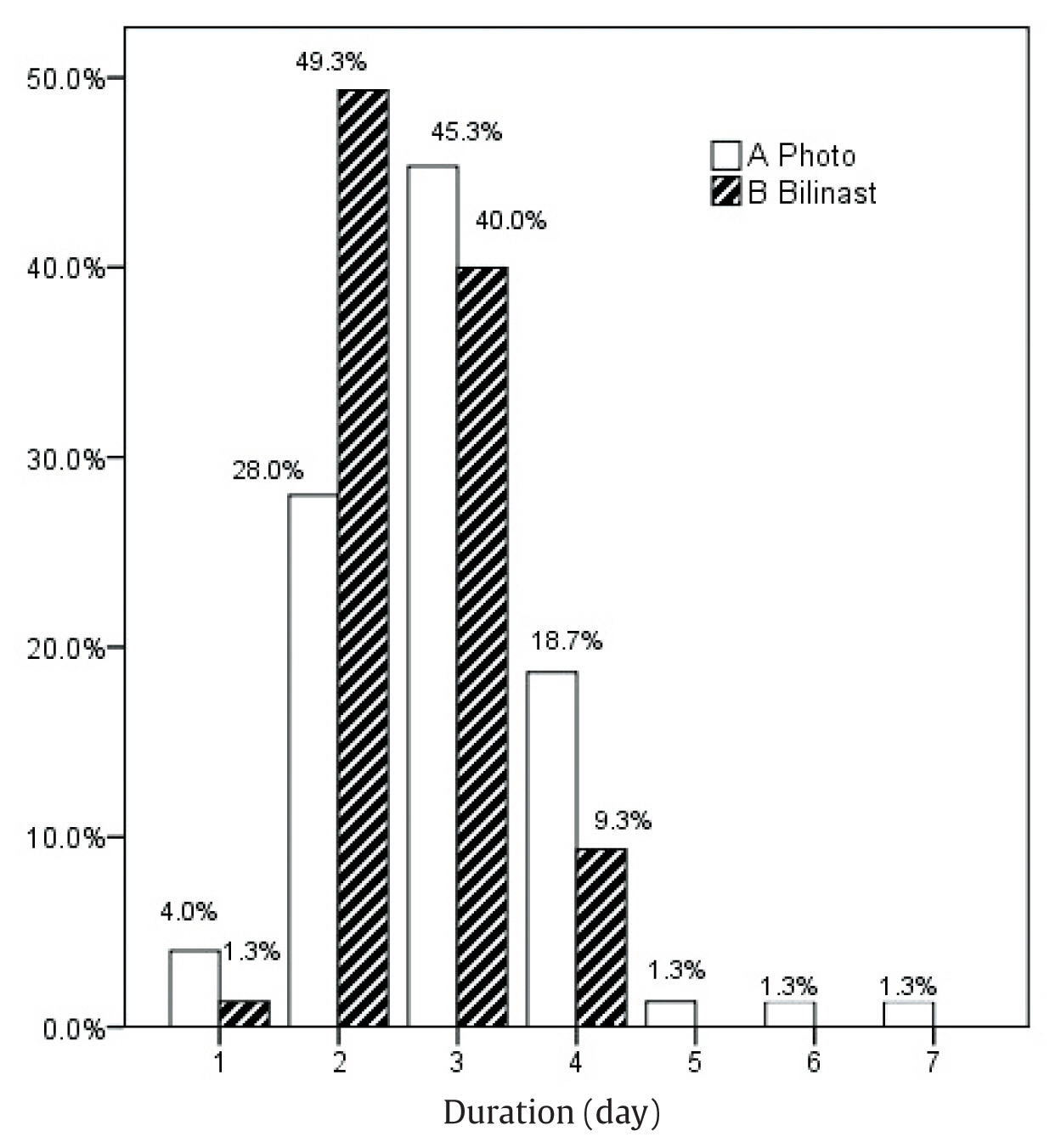
- There were 28% of patients whose hospital duration following phototherapy was 2 days, for Bilineaster and phototherapy treatment this was 49.3% of patients. At 48 hours and 72 hours the reduction in the concentration of total bilirubin in the serum was statistically significantly different across groups (p < 0.05) but at 24 hours and 96 hours there were no significant differences between groups (p > 0.05). The reduction in direct bilirubin concentration in the serum was significantly different between groups at 72 hours and 96 hours (p > 0.001).
-
Conclusion
- Purgative manna and phototherapy, can statistically significantly reduce total bilirubin concentration at 48 hours and 72 hours compared with phototherapy alone, and reduce the length of hospital stay for jaundiced neonates at 2 days compared with phototherapy treatment.
- Neonatal hyperbilirubinemia is a common problem observed in approximately 60% of term and 80% of preterm newborns [1–3] and may lead to kernicterus in severe cases [1,4]. The treatment is usually phototherapy or exchange transfusion [2]. In less severe cases (the vast majority), phototherapy is the most commonly used treatment method [2,5,6]. However in more severe cases, intensive phototherapy methods are used which may result in some adverse effects in neonates [7]. This would require monitoring of the neonates for therapeutic treatment response and adverse events [8,9].
- Categorization of neonates hyperbilirubinemia into mild, moderate, and severe according to the bilirubin concentration would be useful for treatment selection [10,11]. The main mechanism of action of phototherapy is transformation of bilirubin to conjugated forms [12–14]. There are side effects of phototherapy treatment including retinal damage, diarrhea, and skin rashes in neonates [15,16]. In addition, the rate of nosocomial infections may be increased due to phototherapy [16,17]. The use of alternative therapeutic methods offered by traditional medicine such as herbal remedies may be beneficial in the recovery of infants from hyperbilirubinemia [18–22].
- Bilineaster solution is an extract of purgative manna from the cotoneaster isocolor herb. Each mL of this herbal remedy contains 300 mg manitol. It is administered orally and absorbed minimally from alimentary tract leading to osmotic diarrhea aiding the excretion of different isomers of bilirubin. This diarrhea results in decreased serum levels of bilirubin; there were no serious adverse effects of Bilineaster [23]. In this study, the effect of Bilineaster drop and phototherapy was compared with phototherapy alone to determine whether phototherapy duration and the hospital stay could be reduced for in newborns with jaundice.
Introduction
- The study was approved by the Iranian Registry of Clinical Trials (IRCT2013110710933N2), on the 12th May 2014. This interventional study was performed as a randomized clinical trial. There were 150 consecutive term neonates (37 weeks to 40 weeks) that had developed jaundice (after 36 hours to 14 days of age), weighed 2,500 g to 4,000 g, and who were candidates for phototherapy, were enrolled in this trial. Patients who met the inclusion criteria were randomized using sequentially numbered, opaque sealed envelopes. In this system, the envelope containing the treatment allocation was opened by the clinician at the time of registration of the participant, (the clinician did not open the envelope before randomizing the participant) [24,25]. The exclusion criteria applied when there was a need to perform exchange transfusion or intensive phototherapy, or the neonates were; preterm, postdate, had congenital malformations or comorbidity (such as sepsis and infections), weighed < 2,500 g or > 4,000 g, developed jaundice after 2 weeks, had reduced neonatal reflexes, were ABO/Rh mismatch, had direct hyperbilirubinemia, or were fed with formula milk. In this study neonates who were born assisted via vacuum or forceps vaginal delivery were not excluded and the number of assisted births were comparable between groups. The neonates were randomly assigned to intervention or control group [26]. The control patients received only phototherapy (Philips Co., Tehran, Iran) and the intervention group underwent treatment with both phototherapy and Bilineaster drop (Sobhan Daru CO., Tehran, Iran) at a dose of 5 drops per kilogram of body weight, 3 times a day.
- The bilirubin serum levels were measured at the time of admission as a baseline measurement, and every 24 hours across the groups using bilirubin-specific kits (Abnova CO.), and this data was compared across groups. The phototherapy was continued until the level of bilirubin in the serum was 10 mg/dL and if the neonate was generally healthy they were discharged from hospital. The length of hospital stay was determined and compared as a mean value between groups. The bilirubin molecule absorbs visible light (irradiance) ranging from 400 nm to 500 nm, with peaks around 460 nm [27,28]. Therefore, a phototherapy lamp with visible light (irradiance) ranging from 400 nm and 460 nm was used for all neonates across groups.
- 1. Ethical considerations
- This study was approved be Hamadan University of Medical Sciences under the grant number of 16/35/9/3569 in January 2014. Written informed consent was given by all parents. The study was approved by the ethics committee and registration in Iranian Registry of Clinical Trials (IRCT2013110710933N2). All procedures involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments.
- 2. Statistical analysis
- The Kolmogorov-Smirnov test was applied to determine the normal distribution of variables [27,29–32]. Data analysis was performed for 150 neonates including 75 patients in the control group and 75 newborns in the intervention group. Data analysis was performed by Statistical Package for the Social Sciences, version 20 software (IBM Corp., Armonk, NY, USA) [26,28,33–36]. Independent-Sample-T and repeated-measure ANOVA tests were used [37–41] and were considered statistically significant when p < 0.05.
Materials and Methods
- The control and intervention group were similar at baseline for all variables except birth weight and direct bilirubin concentration in the serum but these differences were not statistically significant (Table 1). As shown in Figure 1, > 90% of the patients in the intervention group, and < 80% in the control group were discharged within the first 3 days of admission. The mean length of time for hospital stay was 2.95 ± 1.01 days and 2.57 ± 0.68 days in the control and intervention groups respectively, but there was no statistically significant difference between groups (p = 0.06).
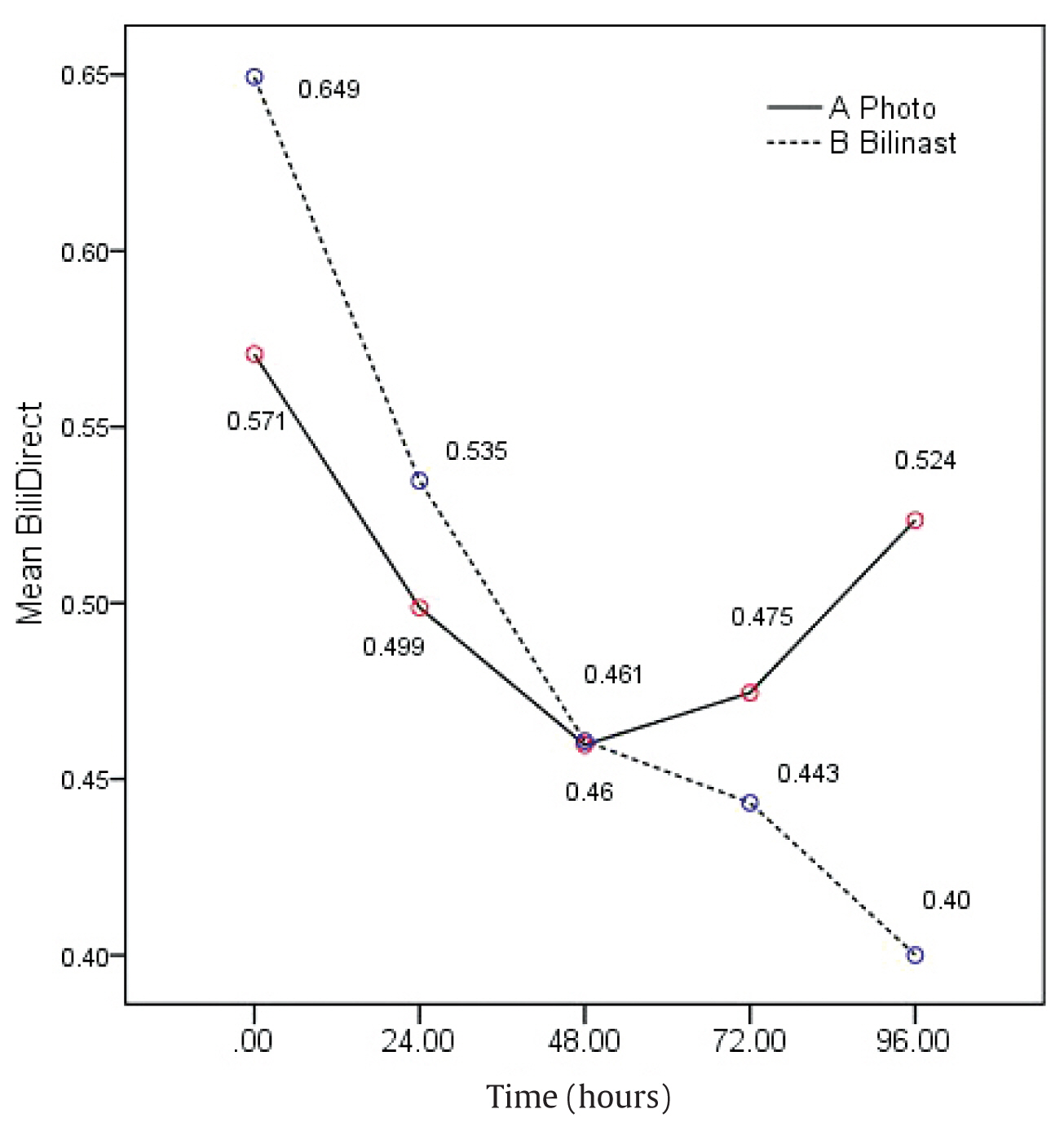
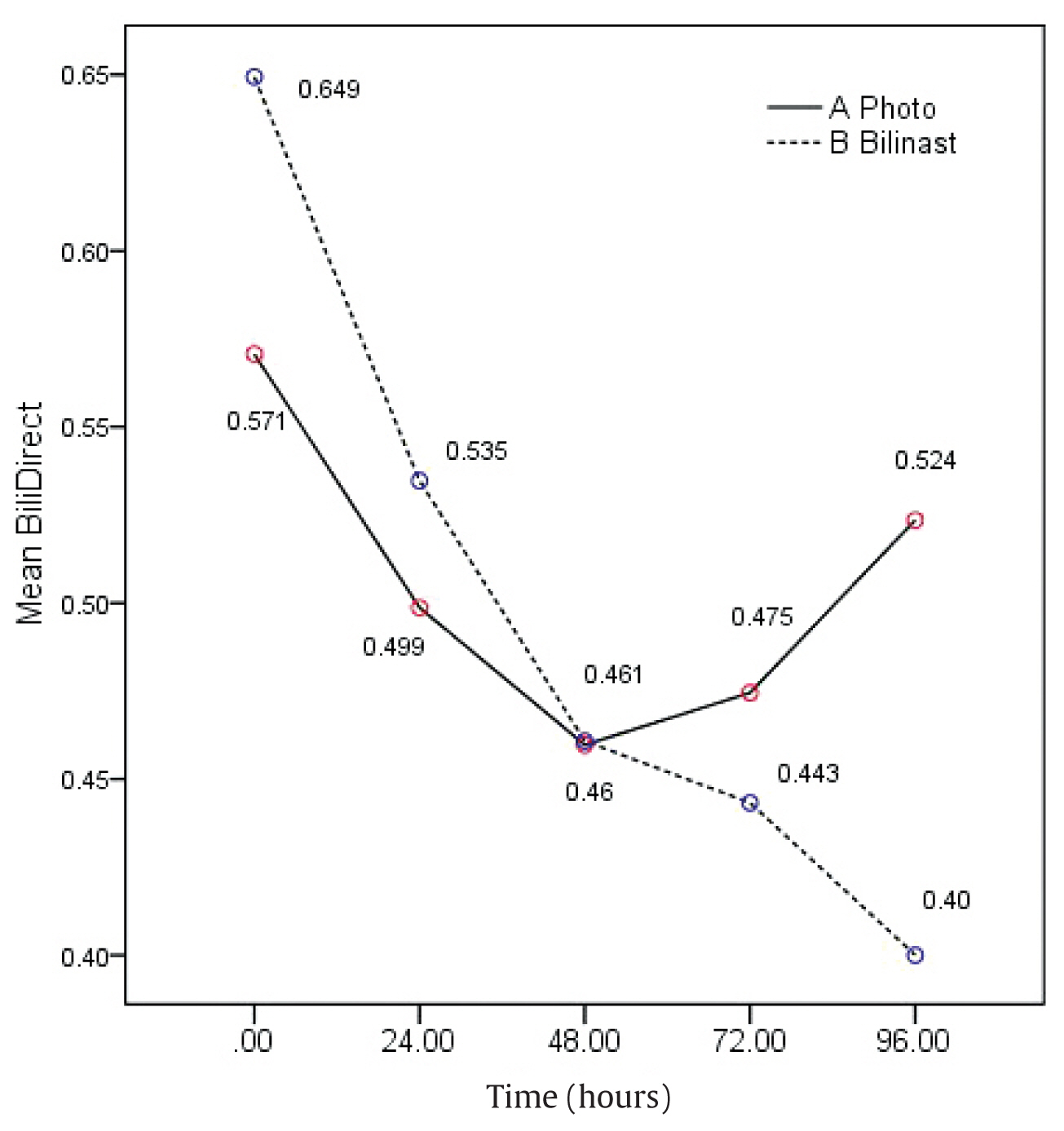
- The serum concentration for total and direct bilirubin levels are shown as mean values in Figures 2 and 3, respectively. The reduced concentration of bilirubin in each group is shown in Table 2 as a mean value. The reduction in total bilirubin concentration from baseline was statistically significantly different across the groups at 48 hours (p < 0.001) and 72 hours (p < 0.001) but, not at 24 hours and 96 hours (Figure 2). The reduction in direct bilirubin concentration from baseline was statistically significantly different across the groups at 72 hours (p < 0.001) and 96 hours (p < 0.001) but, not at 24 hours and 48 hours (Figure 3).
- The patients with higher baseline bilirubin concentrations had higher reduction rates due to treatment, and this was a statistically significant direct correlation (p < 0.001). However, age was not statistically significantly associated with reduced bilirubin concentration (p > 0.05), but birth weight in both groups was statistically significantly inversely correlated with reduced concentration of bilirubin (p = 0.001).
Results
- Jaundice is a common clinical condition among newborns and it can be dangerous even among healthy term neonates. Phototherapy is the treatment of choice for jaundice and was given to both intervention and control groups in this study to determine the role of Bilineaster treatment as an intervention in the reduction of bilirubin concentration in the blood. The groups were of similar age and age of onset of jaundice. Only the birth weight was higher in the intervention group in comparison with the control group but this difference was not statistically significant (p = 0.026).
- More than 90% of patients in intervention group and < 80% in control group were discharged during first 3 days of admission. However, the mean hospital stay was not statistically significantly different across the groups (p = 0.06). This lack of difference across the groups may be due to higher direct bilirubin serum concentration at baseline resulting from a higher birth weight in the intervention group. However, it should be mentioned that the baseline direct bilirubin concentration was statistically significantly higher in intervention group, p > 0.05 but the hospital stay was 0.4 days less than the control group. However, this the positive effect of Bilineaster was not statistically significant. In a similar study in Iran [11] where the intervention and control groups had the same baseline concentration of bilirubin, the hospital stay was statistically significantly less in the intervention group. In addition, there was a third group for comparison in that study; mothers that had consumed Bilineaster [11]. A statistically significant reduction in total bilirubin concentration was seen in all groups showing the effect of phototherapy. The decrease in bilirubin concentration in the phototherapy group at 24 hours was slightly greater in the control group compared with the intervention group, but this was not statistically significantly different. This could be due to a shorter half-life of Bilineaster or lack of initiation of effect. The other etiology is a higher initial direct bilirubin concentration in the intervention group. The reduction of bilirubin concentration in the serum at 48 hours and 72 hours revealed a positive additive effect of Bilineaster on bilirubin concentration. This may be due to binding of the resin in Bilineaster and inhibition of entrance to entrohepatic cycle. However, for a better understanding the mechanism of action of this substance, further studies with larger sample size and hematological studies are recommended. At 96 hours, the reduction in bilirubin concentration was greater in the intervention group compared with the control group but there was no statistically significant difference between groups. This could be due to the small sample size [24 patients (7 patients from the intervention group and 17 neonates in control group)] which may be too small to substantiate a statistically significant association. One study reported similar finding to this current study; a reduction of bilirubin concentration in the intervention group (Bilineaster and phototherapy) at 24 hours of treatment which was greater than the control group (phototherapy) [42]. However, in that study reduction of bilirubin concentration with Bilineaster treatment was not statistically significant different between groups. This difference in results between studies may be due to the assessment of therapeutic effect as described this current study rather than the prophylactic effect studied by Raeisi et al [42]. In addition, the dose of Bilineaster used was higher in this current study. So, the use of higher doses of Bilineaster for assessment of prophylactic effects is recommended. Rafieian-Kopaei et al assessed the effect of cotoneaster isocolor herb (an extract of which is purgative manna) among 100 newborns, and observed that the herbal remedy and phototherapy, was effective in the treatment of neonatal hyperbilirubinemia [43]; a finding similar to this current study. In addition, Ghotbi et al similarly reported that cotoneaster was effective in the treatment of neonatal hyperbilirubinemia resulting in a rapid decline in serum bilirubin concentration and cotoneaster treatment resulted in a reduced hospital stay duration [44].
Discussion
- In this study, treatment of jaundiced neonates with purgative manna (Bilineaster) resulted in a greater reduction of bilirubin concentration in the blood and had additive effects when combined with phototherapy treatment. Moreover, in the Bilineaster and phototherapy group the number of neonates leaving hospital at 2 days was higher than phototherapy treatment alone, although the mean length of stay was not significantly different between groups. Further studies with a larger sample size, mothers who receive Bilineaster, and assessment of prophylactic and therapeutic effects is required.
Conclusion
-
Acknowledgements
- The authors are indebted to Dr. Fardmal for his assistance in statistical analysis, and Mrs. Fattahi for her practical help, and the Research Center of Hamadan University of Medical Sciences for their support.
Acknowledgments
-
Conflicts of Interest
The authors declared that they have no competing interests.
Article information
- 1. Kliegman RM, Behrman RE, Jenson HB, et al. Nelson textbook of pediatrics e-book. Elsevier Health Sciences; 2007.
- 2. Porter ML, Dennis BL. Hyperbilirubinemia in the term newborn. Am Fam Physician 2002;65(4). 599−606. PMID: 11871676.PubMed
- 3. Masoudi Alavi N, Madani M, Sadat Z, et al. Fatigue and vitamin D status in Iranian female nurses. Glob J Health Sci 2015;8(6). 196−202. PMID: 10.5539/gjhs.v8n6p196.Article
- 4. Eghbalian F, Monsef F, Alam-Ghomi N, et al. Effect of low versus moderate dose of clofibrate on serum bilirubin in healthy term neonates with indirect hyperbilirubinemia. Iran J Med Sci 2013;38(4). 349−50. PMID: 24293792. PMID: 3838990.PubMedPMC
- 5. Lazar L, Litwin A, Merlob P. Phototherapy for neonatal nonhemolytic hyperbilirubinemia: analysis of rebound and indications for discontinuing therapy. Clin Pediatr (Phila) 1993;32(5). 264−7. PMID: 10.1177/000992289303200502.ArticlePubMed
- 6. Eghbalian F, Rafienezhad H, Farmal J. The lowering of bilirubin levels in patients with neonatal jaundice using massage therapy: A randomized, double-blind clinical trial. Infant Behav Dev 2017;49:31−6. PMID: 10.1016/j.infbeh.2017.05.002. PMID: 28688960.ArticlePubMed
- 7. Morris BH, Oh W, Tyson JE, et al. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N Engl J Med 2008;359(18). 1885−96. PMID: 10.1056/NEJMoa0803024. PMID: 18971491. PMID: 2821221.ArticlePubMedPMC
- 8. Kaplan M, Kaplan E, Hammerman C, et al. Post-phototherapy neonatal bilirubin rebound: a potential cause of significant hyperbilirubinaemia. Arch Dis Child 2006;91(1). 31−4. PMID: 10.1136/adc.2005.081224.ArticlePubMed
- 9. Drew JH, Marriage K, Bayle VV, et al. Phototherapy. Short and long-term complications. Arch Dis Child 1976;51(6). 454−8. PMID: 10.1136/adc.51.6.454. PMID: 942239. PMID: 1546009.ArticlePubMedPMC
- 10. Azadbakht M, Pishva N, Mohammadi Samani S, et al. The effect of purgative manna on the infant jaundice. Iran J Pharm Res 2005;1(2). 95−100.
- 11. Mansouri M, Ghotbi N, Bahadorbeigi L. Evaluation of the preventive effects of purgative manna on neonatal icterus in Sanandaj. Scientific J Kurdistan Univ Med Sci 2012;17(2). 30−5.
- 12. Ebrahimimd S, Ashkani-Esfahani S, Poormahmudibs A. Investigating the efficacy of Zizyphus jujuba on neonatal jaundice. Iran J Pediatr 2011;21(3). 320−4.PubMedPMC
- 13. Clinical Research Collaborative Group of Yinzhihuang Oral Solution. Multicenter randomized controlled study on the efficacy and safety of Yinzhihuang oral solution for the treatment of neonatal indirect hyperbilirubinemia in term newborn infants. Zhonghua Er Ke Za Zhi 2011;49(9). 663−8. PMID: 22176900.PubMed
- 14. Nag N, Halder S, Chaudhuri R, et al. Role of bilirubin as antioxidant in neonatal jaundice and effect of ethanolic extract of sweet lime peel on experimentally induced jaundice in rat. Indian J Biochem Biophys 2009;46(1). 73−8. PMID: 19374257.PubMed
- 15. Lazar MA. East meets West: an herbal tea finds a receptor. J Clin Invest 2004;113(1). 23−5. PMID: 10.1172/JCI200420661. PMID: 14702104. PMID: 300773.ArticlePubMedPMC
- 16. Fok TF. Neonatal jaundice—traditional Chinese medicine approach. J Perinatol 2001;21(Suppl 1). S98−100. discussion S104–7.PMID: 10.1038/sj.jp.7210643.ArticlePubMedPDF
- 17. Dennery PA. Pharmacological interventions for the treatment of neonatal jaundice. Semin Neonatol 2002;7(2). 111−9. PMID: 10.1053/siny.2002.0098. PMID: 12208095.ArticlePubMed
- 18. Mohammad SM, Kashani HH, Azarbad Z. Capparis spinosa L. Propagation and medicinal uses. Life Sci J 2012;9(4). 684−6.
- 19. Haddad-Kashani H, Seyed-Hosseini E, Nikzad H, et al. Pharmacological properties of medicinal herbs by focus on secondary metabolites. Life Sci J 2012;9(1). 509−20.
- 20. Hosseyni ES, Kashani HH, Asadi MH. Mode of action of medicinal plants on diabetic disorders. Life Sci J 2012;9(4). 2776−83.
- 21. Kamani M, Hosseini ES, Kashani HH, et al. Protective Effect of Lepidium sativum Seed Extract on Histopathology and Morphology of Epididymis in Diabetic Rat Model. Int J Morphol 2017;35(2). 603−10. PMID: 10.4067/S0717-95022017000200036.Article
- 22. Najaran H, Rashtbari H, Mohammadi A, et al. The protective effect of coenzyme Q10 and berberine on sperm parameters, with and without varicocelectomy in rats with surgically induced varicoceles. Comp Clin Path 2019;28(2). 479−85. PMID: 10.1007/s00580-018-2850-y.ArticlePDF
- 23. Hamedi A, Zarshenas MM, Sohrabpour M, et al. Herbal medicinal oils in traditional Persian medicine. Pharm Biol 2013;51(9). 1208−18. PMID: 10.3109/13880209.2013.777462. PMID: 23746335.ArticlePubMed
- 24. Hewitt C, Hahn S, Torgerson DJ, et al. Adequacy and reporting of allocation concealment: review of recent trials published in four general medical journals. BMJ 2005;330(7499). 1057−8. PMID: 10.1136/bmj.38413.576713.AE. PMID: 15760970. PMID: 557225.ArticlePubMedPMC
- 25. Tamadon MR, Soleimani A, Keneshlou F, et al. Clinical trial on the effects of vitamin D supplementation on metabolic profiles in diabetic hemodialysis. Horm Metab Res 2018;50(1). 50−5. PMID: 10.1055/s-0043-119221.ArticlePubMedPDF
- 26. Sharif MR, Kashani HH, Ardakani AT, et al. The effect of a yeast probiotic on acute diarrhea in children. Probiotics Antimicrob Proteins 2016;8(4). 211−4. PMID: 10.1007/s12602-016-9221-2. PMID: 27530282.ArticlePubMedPDF
- 27. Haddad-Kashani H, Nikzad H, Mobaseri S, et al. Synergism effect of nisin peptide in reducing chemical preservatives in food industry. Life Sci J 2012;9(1). 496−501.
- 28. Lotfi A, Shiasi K, Amini R, et al. Comparing the effects of two feeding methods on metabolic bone disease in newborns with very low birth weights. Glob J Health Sci 2016;8(1). 249−54. PMID: 10.5539/gjhs.v8n1p249. PMID: 4804066.Article
- 29. Haddad Kashani H, Moshkdanian Gh, Atlasi MA, et al. Expression of galectin-3 as a testis inflammatory marker in vasectomised mice. Cell J 2013;15(1). 11−8. PMID: 23700556. PMID: 3660020.PubMedPMC
- 30. Hosseini ES, Moniri R, Goli YD, et al. Purification of antibacterial CHAPK protein using a self-cleaving fusion tag and its activity against methicillin-resistant Staphylococcus aureus. Probiotics Antimicrob Proteins 2016;8(4). 202−10. PMID: 10.1007/s12602-016-9236-8. PMID: 27797005.ArticlePubMedPDF
- 31. Nikzad H, Haddad Kashani H, Kabir-Salmani M, et al. Expression of galectin-8 on human endometrium: Molecular and cellular aspects. Iran J Reprod Med 2013;11(1). 65−70. PMID: 24639695. PMID: 3941385.PubMedPMC
- 32. Eghbalian F, Monsef A, Mousavi-Bahar SH. Urinary tract and other associated anomalies in newborns with esophageal atresia. Urol J 2009;6(2). 123−6. PMID: 19472132.PubMed
- 33. Sharif MR, Kheirkhah D, Madani M, et al. The relationship between iron deficiency and febrile convulsion: a case-control study. Glob J Health Sci 2016;8(2). 185−9. PMID: 4804054.Article
- 34. Piroozmand A, Haddad Kashani H, Zamani B. Correlation between Epstein-Barr virus infection and disease activity of systemic lupus erythematosus: a cross-sectional study. Asian Pac J Cancer Prev 2017;18(2). 523−7. PMID: 28345840. PMID: 5454753.PubMedPMC
- 35. Etehadi Moghadam S, Azami Tameh A, Vahidinia Z, et al. Neuroprotective Effects of Oxytocin Hormone after an Experimental Stroke Model and the Possible Role of Calpain-1. J Stroke Cerebrovasc Dis 2018;27(3). 724−32. PMID: 10.1016/j.jstrokecerebrovasdis.2017.10.020.ArticlePubMed
- 36. Sharif A, Kashani HH, Nasri E, et al. The role of probiotics in the treatment of dysentery: a randomized double-blind clinical trial. Probiotics Antimicrob Proteins 2017;9(4). 380−5. PMID: 10.1007/s12602-017-9271-0. PMID: 28321826.ArticlePubMedPDF
- 37. Jalali HK, Salamatzadeh A, Jalali AK, et al. Antagonistic activity of Nocardia brasiliensis PTCC 1422 against isolated Enterobacteriaceae from urinary tract infections. Probiotics Antimicrob Proteins 2016;8(1). 41−5. PMID: 10.1007/s12602-016-9207-0. PMID: 26920557.ArticlePubMedPDF
- 38. Ferdosian M, Khatami MR, Malekshahi ZV, et al. Identification of immunotopes against Mycobacterium leprae as immune targets using PhDTm-12mer phage display peptide library. Trop J Pharm Res 2015;14(7). 1153−9. PMID: 10.4314/tjpr.v14i7.5.Article
- 39. Dehghani R, Sharif A, Madani M, et al. Factors influencing animal bites in Iran: a descriptive study. Osong Public Health Res Perspect 2016;7(4). 273−7. PMID: 10.1016/j.phrp.2016.06.004. PMID: 27635378. PMID: 5014749.ArticlePubMedPMC
- 40. Naeini ZK, Bafrani HH, Nikzad H. Evaluation of ebselen supplementation on cryopreservation medium in human semen. Iran J Reprod Med 2014;12(4). 249−56.PubMedPMC
- 41. Haddad Kashani H, Fahimi H, Dasteh Goli Y, et al. A novel chimeric endolysin with antibacterial activity against methicillin-resistant Staphylococcus aureus. Front Cell Infect Microbiol 2017;7:290PMID: 10.3389/fcimb.2017.00290. PMID: 5491540.ArticlePubMedPMC
- 42. Raeisi R, Heidari-Soureshjani S, Asadi-Samani M, et al. A systematic review of phytotherapies for newborn jaundice in Iran. Int J Pharm Sci Res 2017;8(5). 1953−8.
- 43. Rafieian-Kopaei M, Khoshdel A, Kheiri S, et al. Cotoneaster: A safe and easy way to reduce neonatal jaundice. J Clin Diagn Res 2016;10(4). SC01−3. PMID: 27190910. PMID: 4866208.Article
- 44. Ghotbi F, Nahidi S, Zangi M. Surveying the effect of cotoneaster spp. (shir khesht) on neonatal jaundice. Res Med 2006;30(4). 353−61.
References
Figure 2Total bilirubin concentration (mg/dL) expressed as a mean value, over time. The serum concentration of bilirubin expressed as a mean value for the groups was statistically significantly reduced at 72 hours in the Bilinaster and Phototherapy group compared with the Phototherapy treatment group p = 0.001.


Table 1Baseline characteristics.
Table 2Reduction of bilirubin serum concentration following treatment.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Recent Advances in Adjuvant Pharmacotherapy for Neonatal Indirect Hyperbilirubinemia: A Narrative Review
Seyyedeh Azade Hoseini Nouri, Marjaneh Zarkesh
Journal of Comprehensive Pediatrics.2023;[Epub] CrossRef - The effect of oral use of concentrated pomegranate juice by mothers on hyperbilirubinemia in neonates under phototherapy: A randomized clinical trial
Masomeh Rezapour, Yadollah Zahedpasha, Mohammad Kamalinejad, Zahra Memariani, Morteza Alijanpour, Mousa Ahmadpour-Kacho, SeyyedAli Mozaffarpur, Hoda Shirafkan
Journal of Research in Medical Sciences.2023; 28(1): 46. CrossRef - The effects of clofibrate on neonatal jaundice: A systematic review
Fathemeh Eghbalian, Ali Hasanpour- Dehkordi, Roya Raeisi
International Journal of Preventive Medicine.2022; 13(1): 3. CrossRef


 PubReader
PubReader ePub Link
ePub Link Cite
Cite