Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 12(5); 2021 > Article
-
Original Article
Delays in the diagnosis and treatment of tuberculosis during the COVID-19 outbreak in the Republic of Korea in 2020 -
Jiyeon Yang1
 , Yunhyung Kwon1
, Yunhyung Kwon1 , Jaetae Kim1
, Jaetae Kim1 , Yoojin Jang1
, Yoojin Jang1 , Jiyeon Han1
, Jiyeon Han1 , Daae Kim1
, Daae Kim1 , Hyeran Jeong1
, Hyeran Jeong1 , Hyekyung Park2
, Hyekyung Park2 , Eunhye Shim1
, Eunhye Shim1
-
Osong Public Health and Research Perspectives 2021;12(5):293-303.
DOI: https://doi.org/10.24171/j.phrp.2021.0063
Published online: September 23, 2021
1Division of Tuberculosis Prevention and Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Korea
2Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Korea
- Corresponding author: Yunhyung Kwon Division of Tuberculosis Prevention and Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Korea E-mail: yhhodori@korea.kr
- Jiyeon Yang and Yunhyung Kwon contributed equally to this study as co-first authors.
© 2021 Korea Disease Control and Prevention Agency
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- We investigated the impact of the coronavirus disease 2019 (COVID-19) pandemic on tuberculosis (TB) "diagnosis and" management in the Republic of Korea (ROK).
-
Methods
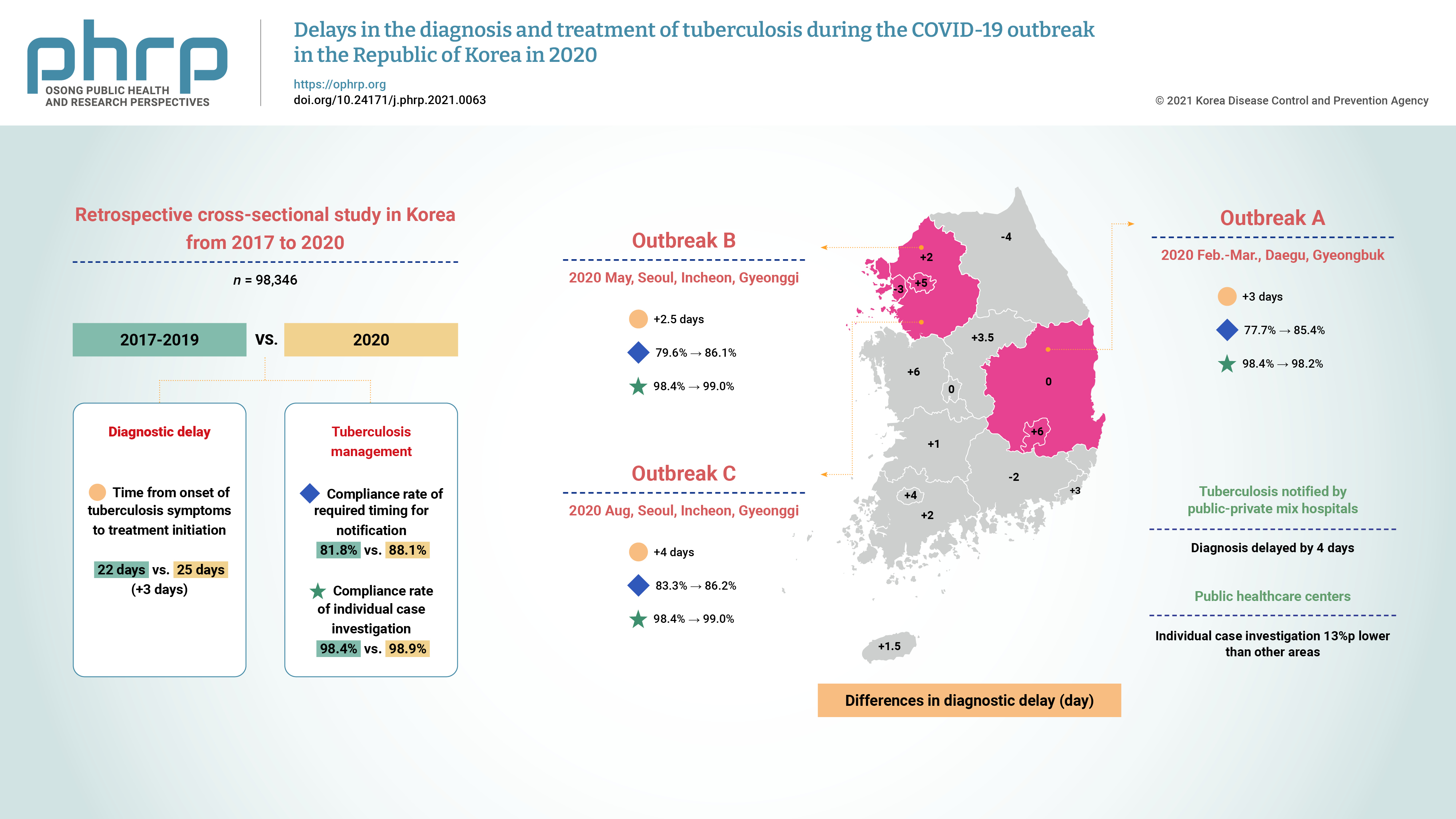
- This retrospective cross-sectional study used nationwide ROK TB notification data (98,346 cases) from 2017 to 2020. The median time from the onset of TB symptoms to treatment initiation and the compliance rates with the required timing for notification and individual case investigations were measured and compared across periods and regions affected by the COVID-19 epidemic.
-
Results
- TB diagnosis during the COVID-19 pandemic was delayed. The median time to TB treatment initiation (25 days) in 2020 increased by 3 days compared to that of the previous 3 years (22 days) (p<0.0001). In the outbreak in Seoul, Incheon, and Gyeonggi province during August, the time to TB diagnosis was 4 days longer than in the previous 3 years (p=0.0303). In the outbreak in Daegu and Gyeongbuk province from February to March 2020, the compliance rate with the required timing for individual case investigations was 2.2%p lower than in other areas in 2020 (p=0.0148). For public health centers, the rate was 13%p lower than in other areas (80.3% vs. 93.3%, p=0.0003).
-
Conclusion
- TB diagnoses during the COVID-19 pandemic in the ROK were delayed nationwide, especially for patients notified by public-private mix TB control hospitals. TB individual case investigations were delayed in regional COVID-19 outbreak areas (Daegu and Gyeongbuk province), especially in public health centers. Developing strategies to address this issue will be helpful for sustainable TB management during future outbreaks.
- On January 2, 2020, in Wuhan, China, coronavirus disease 2019 (COVID-19) was first identified, and in March 2020, the World Health Organization (WHO) declared COVID-19 as a global pandemic [1,2]. In the Republic of Korea (ROK), a nationwide COVID-19 epidemic began after the first case was confirmed on January 20, 2020 [3]. In particular, a few large-scale regional outbreaks occurred in 2020. In Daegu and Gyeongbuk province, a COVID-19 outbreak related to religious facilities occurred from February to March 2020. In Seoul, Incheon, and Gyeonggi province, a COVID-19 outbreak related to nightclubs in Itaewon, Seoul took place in May [4]. Another outbreak related to religious facilities occurred in Seoul, Incheon, and Gyeonggi province in August 2020. Dozens of medical institutions, including the Masan National Tuberculosis Hospital, were designated as infectious disease control institutions under the Infectious Disease Control and Prevention Act (Article 37) to accommodate COVID-19 cases. Tuberculosis (TB) patients who were being treated at the Masan National Tuberculosis Hospital were sent to another national TB hospital, and no TB patients could be admitted to the designated Masan National TB Hospital during the corresponding period. COVID-19 patients were also prioritized for negative-pressure units in hospitals.
- TB is a major cause of death worldwide and should not be neglected even during the current pandemic [5–7]. However, data collated by the WHO from high TB burden countries showed sharp drops in TB notifications in 2020 [7]. In the ROK, the total number of TB cases in 2020 was 25,350 (49.4 cases per 100,000 population), corresponding to a decrease by 16.3% from 2019 [8]. TB has many similarities to COVID-19 regarding its main site of occurrence (the lungs), treatment resources (medical teams in the pulmonary or infectious disease divisions), and prevention methods (masks, ventilation, etc.). A prior study reported a high mortality rate among COVID-19 patients with TB [9]. In the ROK, a cross-sectional survey was conducted to evaluate the impact of COVID-19 on TB management in public-private mix (PPM) TB control hospitals in Korea based on the WHO’s survey tool in August and September, 2020 [10]. Of the 201 survey respondents, 63.2% responded that they experienced a decline in routine TB services during the COVID-19 pandemic and 47.3% responded that the number of newly diagnosed TB patients had decreased. In addition, COVID-19 led to failure to hospitalize some TB patients who needed hospitalization (26.9%) and to the discharge of hospitalized TB patients (16.9%). Kwak et al. [11] found that there was a 24% decrease in TB notifications after the COVID-19 pandemic began. Early diagnosis of TB, as a main indicator of TB management, increases the likelihood of successful treatment and could reduce the risk of community transmission by shortening the duration of exposure to others [12]. Therefore, it is important to understand the impact of the COVID-19 pandemic on TB diagnosis and management.
- Diagnostic delay is defined as the time from the first onset of symptoms related to pulmonary TB to the start of TB treatment, and can be subdivided into patient delay and health system delay [13]. Patient delay refers to the duration from the onset of the first symptoms to the date when the patient first visits any type of health care institution for those symptoms. Health system delay refers to the period from the date of the patient’s first contact with the health care institution to the date of diagnosis.
- The effect of the COVID-19 pandemic on TB is not confined to TB diagnosis. TB management can also be delayed, and it is necessary to assess whether there have been delays in TB management during the COVID-19 pandemic. When physicians diagnose and treat TB or suspected TB patients, they are required to notify the health authorities within 24 hours. As of 2020, an individual case investigation must be performed within 3 days for all notified patients, while until 2019, investigations had to be performed within 3 days for sputum smear-positive patients and within 7 days for sputum smear-negative patients. Delays in initial TB management, such as TB notifications or individual case investigations, based on legal requirements and the guidelines for TB management may be affected by changes in the numbers or roles and responsibilities of the staff who are in charge of those tasks as a result of the COVID-19 pandemic. Therefore, in order to determine whether the COVID-19 pandemic affected TB management, it is necessary to evaluate changes in the compliance rate with the required timing for notification and investigations.
- This is the first study to evaluate the potential impact of the COVID-19 pandemic on TB cases and delays in TB diagnosis or individual case investigations during the COVID-19 pandemic in the ROK. We expect that our study findings will serve as baseline data for establishing a TB management policy, which will be necessary to prepare for outbreaks of other respiratory infections such as COVID-19 in the future.
Introduction
- Study Design and Population
- This was a retrospective cross-sectional study analyzing mandatorily collected Korean TB report data from January 2017 to December 2020 according to the Tuberculosis Prevention Act. Of the data on 125,494 cases that were extracted from the Korean National TB Surveillance System, data on 98,346 cases were included in this study after excluding 27,148 cases that were not new TB cases or duplicates. From 2017 to 2019, there were 78,445 cases, of which 53,231 were symptomatic. The data from 2017 to 2019 were used as a baseline for comparisons with 2020. In 2020, there were 19,933 cases, of which 13,354 were symptomatic. We compared delays in diagnosis and TB management between before and during the pandemic, which occurred in 2020. There were 3 outbreaks in 2020. Outbreak A was the first outbreak, which occurred in Daegu and Gyeongbuk province from February to March 2020. Outbreak B occurred in Seoul, Incheon, and Gyeonggi province in May, and was related to nightclubs in Itaewon, Seoul. Outbreak C occurred in August 2020 in Seoul, Incheon, and Gyeonggi province and was related to religious facilities. Each outbreak corresponded to specific months. We compared the values of variables in the months corresponding to each outbreak between 2017–2019 and 2020 in the outbreak areas and in other areas.
- Individual Case Investigations
- Based on the Tuberculosis Prevention Act and the national guideline [14], each TB case notified by physicians is mandatorily investigated following the Tuberculosis Case Investigation report form within 3 days after notification. Until 2019, investigations had to be performed within 3 days for sputum smear-positive patients and within 7 days for sputum smear-negative patients. The purpose of individual case investigations is to investigate whether the cases have family members and other contacts in settings where people congregate (e.g., schools or workplaces) or in regular gatherings. TB epidemiologic investigators who belong to the Korea Disease Control and Prevention Agency (KDCA) and TB management staff in local public healthcare centers conduct contact investigations based on the facts identified through the individual case investigations. The transmission of TB to others can be prevented if these investigations are performed rapidly and thoroughly. Another purpose of individual case investigations is to follow up on the results of tests or treatment related to TB. Individual case investigations are performed by dedicated TB nurses in PPM TB control project hospitals or by TB management staff in public health centers. The TB management staff in public health centers are also responsible for individual case investigations for cases notified by non-PPM institutions.
- Variables and Statistical Analysis
- To determine the TB diagnostic delay and TB management delay, we defined the following variables. The time to TB treatment initiation was defined as the period from the onset of symptoms to the time when TB treatment was started. It was not possible to divide the diagnostic delay into patient versus health system delays since the data of TB notifications and individual case investigations did not contain information on the dates of visits to medical institutions or health care centers. This variable was calculated only for TB patients who had TB symptoms. Among symptomatic cases, 769 cases were excluded because they had no information on the date of TB treatment initiation. In this study, we divided the regions into those where the 3 specific COVID-19 outbreaks (outbreaks A–C) occurred and others and compared variables between those 2 groups for each outbreak using the non-parametric Mann-Whitney test because the data did not follow a normal distribution. The data are presented as median values. The median numbers of days from the onset of symptoms to TB treatment initiation in 2020 were compared with those in the previous 3 years before the COVID-19 pandemic (2017–2019). The median numbers in the outbreak areas during the outbreak period were also compared with the same variables in other areas during the same period. To evaluate the delay in the initial management of TB patients, we defined 2 variables. The time to TB notification was defined as the period from when TB patients’ treatment was started to the notification date. The time to individual case investigation was defined as the time from the date of TB notification to the date of submission of individual case investigation reports. For these 2 variables, 1,860 cases and 2,609 cases were excluded, respectively, due to a lack of the relevant information. The national guideline indicates that investigations should not be conducted in certain cases (e.g., prisoners or the dead). We compared the compliance rate with the required timing in 2017–2019 and 2020, between outbreak areas and other areas using the chi-square test. In this study, we applied the previous timing requirement to compare the compliance rates for individual case investigations between before and after the pandemic. For each of the 3 variables, we excluded outliers (data in the upper or lower 1%). A p-value <0.05 was considered to indicate statistical significance. The statistical analysis was performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
- Ethical Approval and Consent to Participate
- TB is a nationally notifiable disease according to the Korean Infectious Disease Control and Prevention Act and the Tuberculosis Prevention Act. Thus, the requirement for written informed consent from patients was waived. This was a retrospective study using existing data, and all data for the study were de-identified before analysis. The study was approved by the KDCA Institutional Review Board (IRB No: 2021-06-14-PE-A).
Materials and Methods
- Time to TB Treatment Initiation
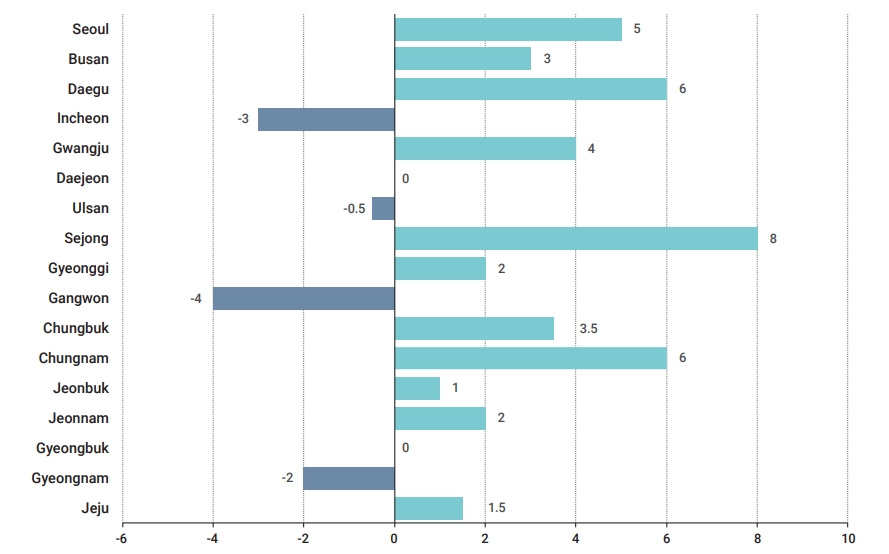
- We compared the time from the onset of symptoms to TB treatment initiation between the COVID-19 pandemic of 2020 and the previous 3 years (2017–2019) (Tables 1, 2). We also evaluated the time to TB treatment initiation in 3 outbreak areas compared to other areas in the same period when outbreaks occurred (Table 3).
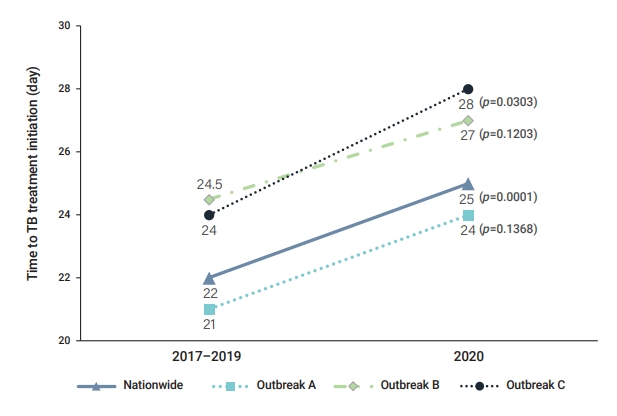
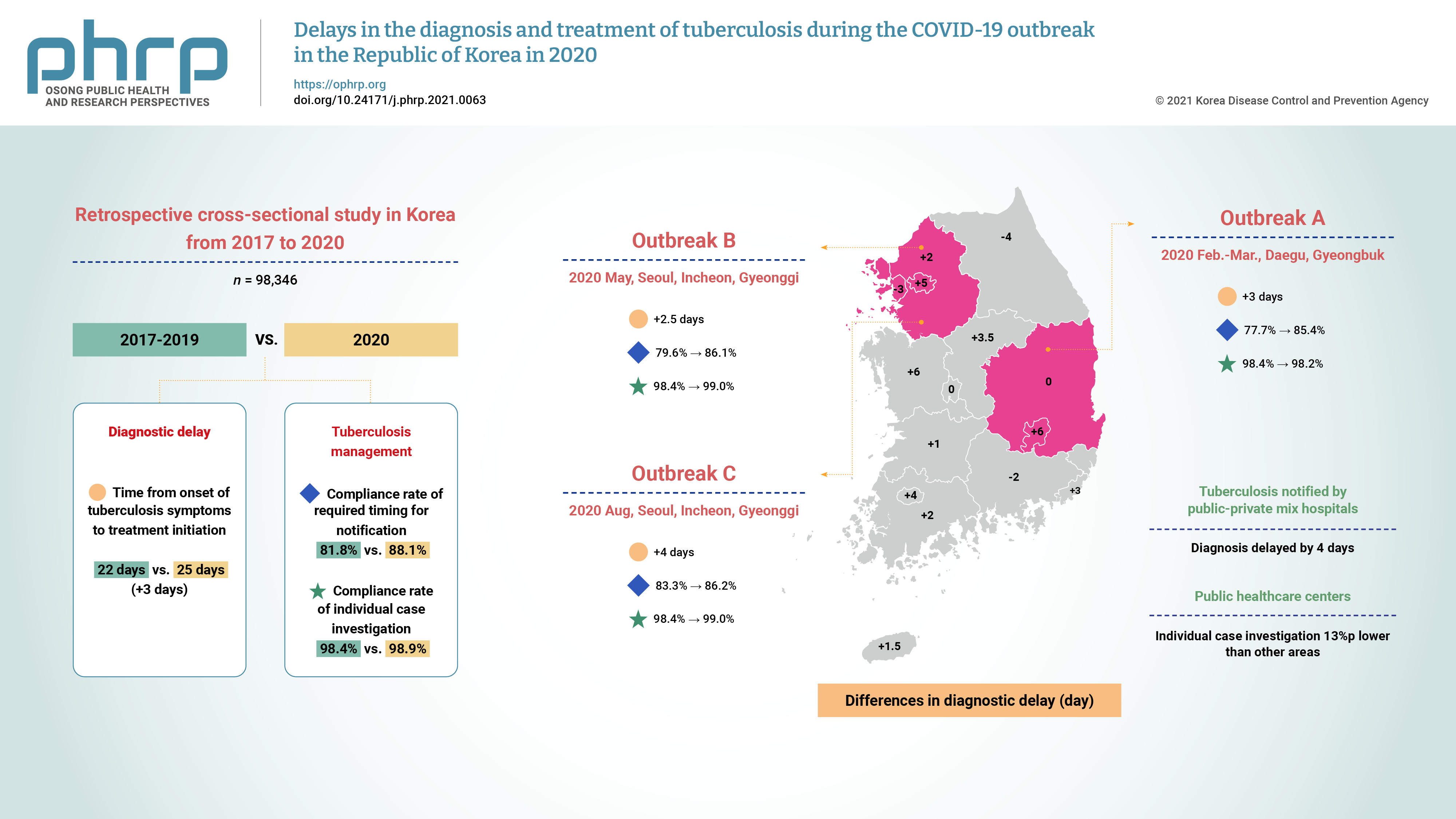
- The overall findings are shown in Table 1. The median number of days from the onset of symptoms to TB treatment initiation was 22 in 2017–2019 and 25 in 2020. This difference of 3 days was statistically significant (p<0.0001). The time to TB treatment initiation was 2 days longer in 2020 during the COVID-19 pandemic in both men and women (p<0.0001). The time to TB treatment initiation was 2 to 5 days longer in each age group, except for the 0- to 9-year-old group and the over-80 age group. The time was 11.5 days shorter in 2020 in the 0 to 9-year-old group (p=0.2798). In the over-80 group, the time in 2020 was the same as in 2017–2019 (p=0.3433). For PPM hospitals, the time to TB treatment initiation was 4 days longer in 2020, which was a statistically significant difference (p<0.0001). For non-PPM or public health centers, the time in 2020 was similar to that in 2017–2019. In a comparison according to the results of the sputum smear test, the time was 2 days longer for sputum smear-positive cases and 3 days longer for negative cases in 2020. In an analysis by region, longer times to TB treatment initiation in 2020 were found in Seoul (5 days longer), Busan (3 days longer), Daegu (6 days longer), Sejong (8 days longer), Gyeonggi province (2 days longer), Chungnam province (6 days longer), and Jeonnam province (2 days longer) (p<0.05). Gangwon province had the opposite result, with a time that was 4 days shorter in 2020 (p=0.0214) (Figure 1).
- We compared the time to TB treatment initiation in the areas where COVID-19 outbreaks occurred between the period during which the outbreak occurred in 2020 and the same months in the previous 3 years (Table 2, Figure 2). For outbreak A (in February to March, 2020), the time was 3 days longer than that of the same months in the previous 3 years in Daegu and Gyeongbuk province. For outbreaks B and C, the time was 2.5 days longer during May and 4 days longer during August 2020 than in the corresponding months in the previous 3 years in Seoul, Incheon, and Gyeonggi province. This difference was only statistically significant for outbreak C (p=0.0303).
- The time to TB treatment in the outbreak A areas (24 days) was 1 day shorter than in other areas (25 days), which was not a statistically significant difference (p=0.6884). The time to TB treatment initiation in the outbreak B areas (27 days) was 5 days longer than in other areas (22 days). The time to TB treatment initiation in the outbreak C areas (28 days) was 6 days longer than in other areas (22 days). The differences between the outbreak areas (outbreak B and outbreak C) and other areas in the same month were not statistically significant (p=0.1335, p=0.0595) (Table 3).
- Time to TB Notification
- We compared the compliance rate with the required timing for notifying TB cases between the COVID-19 pandemic of 2020 and the previous 3 years (2017–2019) and between each outbreak area and other areas in the same period in 2020. The compliance rate was 81.8% throughout the nation in 2017–2019 and 88.1% in 2020 (p<0.0001) (Table 4). For the outbreak A areas, the compliance rate was 85.4% in the outbreak period in 2020 and 77.7% in the same months during 2017–2019 (p=0.0014). For the outbreak B and outbreak C areas, the compliance rates were 86.1% and 86.2% in the outbreak periods in 2020 and 79.6% and 83.3% in the same months in 2017–2019, respectively. The rates were 6.5%p higher in 2020 for outbreak B (p<0.0001) and 2.9%p higher in 2020 for outbreak C (p=0.0458).
- The compliance rates were 85.4%, 86.1%, and 86.2% in outbreak A, outbreak B, and outbreak C, respectively. The rates of the other areas in the same period as each outbreak were 87.7%, 88.0%, and 88.9%, respectively. The compliance rates in other areas were higher than in the outbreak areas, but none of the differences were statistically significant (Table 5).
- Time to Individual Case Investigation
- We compared the compliance rate with the required timing for performing individual case investigations between the COVID-19 pandemic in 2020 and the previous 3 years (2017–2019) and between each outbreak area and other areas in the same period in 2020 (Table 6). The compliance rate was 98.4% throughout the nation in 2017–2019 and 98.9% in 2020. The rate in 2020 was 0.5%p higher than that in 2017–2019 (p<0.0001). Public health centers are responsible for conducting individual case investigations of cases notified by non-PPM medical institutions. We compared the compliance rate by the type of medical institution (PPM hospitals or public health centers) with the previous time requirement. For PPM hospitals, the compliance rate improved by 0.4%p, which was statistically significant (p=0.0004). For public health centers, it was 0.6%p higher in 2020, which was not statistically significant. For the outbreak A areas, the compliance rate was 98.4% in the corresponding months in 2017–2019, and the rate in 2020 was similar to before (0.2%p lower, p=0.8302). For the outbreak B and outbreak C areas, the compliance rates were the same (98.4%) in the corresponding periods in 2017–2019 and the same (99.0%) in 2020. For PPM hospitals, the compliance rates improved by 0.2%p to 0.5%p in each outbreak area in 2020, which was not statistically significant. For public health centers, there was a fluctuation of some percentage points in 2020 relative to previous values, but these differences were not statistically significant.
- In 2020, when the new timing requirements were applied, the compliance rates were 95.6%, 97.5%, and 96.1% in the areas of outbreak A, outbreak B, and outbreak C, respectively (Table 7). The rates of other areas in the same period as each outbreak were 97.8%, 96.0% and 95.1%, respectively. The only statistically significant difference was found for outbreak A, where the compliance rate in the outbreak area was 2.2%p lower than in other areas (p=0.0148). For PPM hospitals, there was no substantial difference in compliance rates between the outbreak areas and the other areas. For public health centers, the rate was 13%p lower in outbreak A than in other areas (p=0.0003), while the rates in the areas of outbreak B and outbreak C were similar to those in other areas.
Results
- Our study showed that the diagnosis of TB was delayed during the COVID-19 pandemic in 2020. A delay of 3 days was found during the COVID-19 pandemic in the time from the onset of TB symptoms to TB treatment initiation. This TB diagnostic delay can be explained by the delay in patients’ first visits to the medical institutions, as well as health system delays (i.e., those related to the medical system) [12,15]. It is possible that patients’ first visits to medical institutions to see a doctor were delayed despite the symptoms of TB patients due to concerns regarding exposure to COVID-19 patients. The pandemic has adversely affected public sentiment by creating fear and anxiety [16,17]. According to a recent survey among medical staff (doctors or dedicated TB nurses) in PPM hospitals in the ROK, a substantial proportion of respondents (17.4%) stated that TB patients were afraid to visit medical institutions due to fear of becoming infected with COVID-19 [18], while some TB patients who needed hospitalization refused hospitalization [10]. Nonetheless, patients having respiratory symptoms could find it difficult to see doctors since they would be redirected to COVID-19 screening clinics [19], patients had to undergo procedures such as checking for fever and filling out questionnaires before seeing a doctor for TB diagnosis and treatment. In other words, the diagnosis of TB might have been delayed because COVID-19 was prioritized as a potential diagnosis in patients with respiratory symptoms rather than TB [19]. Furthermore, according to news articles in the ROK, a few medical institutions did not even accept patients from Daegu, where the first large outbreak of COVID-19 occurred [20]. When COVID-19 patients were diagnosed at medical institutions and public health centers, these facilities were immediately closed and their medical services were discontinued since they had many high-risk patients. Therefore, the delay in TB diagnosis may have been due to decreased access to medical care, as well as patient-related factors [5,6,10,11].
- In almost all age groups, the time to TB treatment initiation was longer during the COVID-19 pandemic in 2020. However, it was much shorter (11.5 days) than before the pandemic in the 0- to 9-year-old age group, unlike other age groups. Due to the young age of these patients, the COVID-19 outbreak may have spurred their parents or guardians to visit medical institutions more urgently. Since the symptoms of COVID-19 are almost identical to those of TB, their parents and guardians might have suspected COVID-19, prompting them to visit medical institutions early, which in turn led to an earlier TB diagnosis. At the first clinical presentation a wide range of differential diagnoses must be considered, providing an opportunity to diagnose other diseases early [21]. We evaluated the time taken for TB diagnosis by the type of medical institution. PPM hospitals accounted for around 80% of all TB patients in the ROK. Among the 67 designated infectious disease control institutions in 2020, 22 (32.8%) were PPM hospitals, including Masan National Tuberculosis Hospital [22]. For TB cases notified by PPM hospitals, the diagnosis of TB was delayed by 4 days compared to the previous 3 years, whereas it was not delayed for non-PPM hospitals and public health centers, which had fewer TB patients than before. Fortunately, the coverage of acid-fast bacilli smear and culture tests and drug susceptibility testing was above 90% at PPM hospitals, which implies that TB management was carried out at PPM hospitals under the national PPM TB control project in the ROK regardless of the pandemic [23].
- In the areas affected by each outbreak, we found that there was a delay in TB diagnosis (Figure 2). This was only significant for the outbreak in Seoul, Incheon, and Gyeonggi province in August (outbreak C), which had a delay of 4 days in TB diagnosis compared to before the pandemic. Meanwhile, a few province-level areas, including the city of Daegu where the first larger outbreak occurred and some areas without large-scale outbreaks had delays in TB diagnosis throughout 2020, but some areas had shorter times to TB treatment initiation (Figure 1). Given these circumstances, COVID-19 outbreaks in the context of the pandemic were considered to have had impacts on TB nationally in 2020, with geographic variation due to differences in how local health authorities carried out prevention strategies and resource distribution depending on local conditions and based on the central health authority’s policy.
- We confirmed that there was no delay in TB notification during the COVID-19 pandemic, including the outbreak areas, compared to the previous 3 years. Individual case investigations were not delayed overall in 2020 compared to before the pandemic. However, the compliance rate with the required timing for individual case investigations in Daegu and Gyeongbuk province from February to March, 2020 was lower than in other areas in the same period. Furthermore, it was clearly shown that individual case investigations carried out at public health centers were delayed during the outbreaks in Daegu and Gyeongbuk province, with a 13%p lower compliance. The dedicated TB staff could not deal with the corresponding tasks in time, while PPM hospitals were not affected by the COVID-19 pandemic in terms of compliance with the required timing for TB individual case investigations. Public health centers in the ROK prioritized responding to COVID-19 in terms of staff and resources, which may have affected TB management, particularly at the beginning of the pandemic. However, our analysis showed that there were no delays in TB notifications and individual case investigations in PPM hospitals during the COVID-19 pandemic. A major reason for this may be the maintenance of dedicated TB nurses in PPM hospitals, even when medical resources were concentrated on the COVID-19 response [14]. In the analysis of TB management indicators at PPM medical institutions, it was reported that the initial TB test rate and the initial compliance rate with treatment guidelines during the COVID-19 pandemic were well maintained, without any substantial differences compared to the rates before COVID-19 [23]. In addition, it is necessary to consider the decrease in the number of people diagnosed with TB during the COVID-19 pandemic compared to the same period in 2017–2019 [11]. Therefore, continuing support should be provided for medical resources dedicated to TB management to flexibly respond to any possible changes, including a potential temporary increase in TB notifications after the COVID-19 pandemic [11,19]. Through our study, we learned that adequate preparation to address other diseases during the prolonged pandemic is required [5-7,24].
- This study has several limitations. First, it was a retrospective study and only notified cases were included in the analysis. It is likely that some patients with TB died before diagnosis and that some TB cases were not notified, and those cases were impossible to include. Another limitation is that we could not evaluate the respective impact of patient delay and health system delay because we did not have information on the date of patients’ first visits to medical institutions, which would have been necessary to distinguish these delays. The information was also insufficient to determine specific factors related to delays in diagnosis, such as underlying diseases or knowledge, patients’ attitudes towards TB, and the local environment related to health care. We should scrutinize where exactly delays in diagnosis occur and investigate various factors causing delays in the diagnosis of TB, such as health strategies, infrastructure related to health care, personnel in each local region, and so on. To achieve this goal, we should gather the corresponding information for future analysis. Despite these limitations, this study is meaningful in that the data analyzed were nationally representative, and the findings will be helpful for developing an evidence-based policy for TB management and prevention of delayed diagnoses.
Discussion
- The diagnosis of TB during the COVID-19 pandemic in the ROK was delayed nationwide, especially for patients notified by PPM hospitals, which cover about 80% of all TB patients. Delays in TB notification did not occur. Some delays in TB individual case investigations in Daegu and Gyeongbuk province, where an outbreak occurred, were confirmed. Especially in public health centers, there was a relatively large delay in individual case investigations in the outbreak areas. To establish a policy and strategies for minimizing delays in TB diagnosis, follow-up studies are needed to identify patient-related and health care system factors that cause delays. Understanding factors in detail through future studies and developing strategies accordingly will be helpful for sustainable TB management during outbreaks of other infectious diseases in the future.
Conclusion
-
Ethics Approval
The study was approved by the KDCA Institutional Review Board (IRB No: 2021-06-14-PE-A). The requirement for written informed consent from patients was waived.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
All data analyzed in this study are included in this article. For other data, these may be available through the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: YK, JY, HP, ES; Data curation: JK; Formal analysis: JK; Investigation: YJ, JH, DK, HJ; Methodology: YK; Writing-original draft: JY, YK; Writing-review & editing: YK.
-
Additional Contributions
We would like to express our deep appreciation to the health care providers at the public-private mix hospitals and public health centers for making efforts to ensure that tuberculosis patients were well-treated despite the COVID-19 situation in the Republic of Korea.
Article information
Outbreak A occurred in Daegu and Gyeongbuk province from February to March 2020. Outbreaks B and C occurred in Seoul, Incheon, and Gyeonggi province in May and August 2020, respectively. Compliance rate with the time to individual case investigation based on the requirement to perform the investigation within 3 days for sputum smear-positive patients and within 7 days for sputum smear-negative patients.
PPM, public-private mix (tuberculosis control project hospitals); PHC, public health centers.
Outbreak A occurred in Daegu and Gyeongbuk province from February to March 2020. Outbreaks B and C occurred in Seoul, Incheon, and Gyeonggi province in May and August 2020, respectively. Compliance rate with the time to individual case investigation based on the requirement to perform the investigation within 3 days after the notification.
PPM, public-private mix (tuberculosis control project hospitals); PHC, public health centers.
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497−506.ArticlePubMedPMC
- 2. World Health Organization (WHO). Timeline: WHO's COVID-19 response [Internet]. Geneva: WHO; 2020 [cited 2020 Jan 25]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline.
- 3. Kim JY, Choe PG, Oh Y, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci 2020;35:e61.ArticlePubMedPMC
- 4. Kang CR, Lee JY, Park Y, et al. Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg Infect Dis 2020;26:2499−501.ArticlePubMedPMC
- 5. McQuaid CF, McCreesh N, Read JM, et al. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur Respir J 2020;56:2001718. ArticlePubMedPMC
- 6. Alene KA, Wangdi K, Clements A. Impact of the COVID-19 pandemic on tuberculosis control: an overview. Trop Med Infect Dis 2020;5:123. ArticlePubMedPMC
- 7. World Health Organization (WHO). Global tuberculosis report 2020. Geneva: WHO; 2020.
- 8. Korea Disease Control and Prevention Agency (KDCA). Annual report on the notified tuberculosis in Korea, 2020. Cheongju: KDCA; 2020. Korean.
- 9. Gupta N, Ish P, Gupta A, et al. A profile of a retrospective cohort of 22 patients with COVID-19 and active/treated tuberculosis. Eur Respir J 2020;56:2003408. ArticlePubMedPMC
- 10. Min J, Kang JY, Kim J, et al. Impact of COVID-19 on TB services in Korea. Int J Tuberc Lung Dis 2021;25:400−2.ArticlePubMed
- 11. Kwak N, Hwang SS, Yim JJ. Effect of COVID-19 on tuberculosis notification, South Korea. Emerg Infect Dis 2020;26:2506−8.ArticlePubMedPMC
- 12. Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health 2008;8:15. ArticlePubMedPMC
- 13. Kuznetsov VN, Grjibovski AM, Mariandyshev AO, et al. Two vicious circles contributing to a diagnostic delay for tuberculosis patients in Arkhangelsk. Emerg Health Threats J 2014;7:24909. ArticlePubMed
- 14. Korea Disease Control and Prevention Agency (KDCA). 2020 National Guideline of TB management. Cheongju: KDCA; 2020. Korean.
- 15. Sreeramareddy CT, Panduru KV, Menten J, et al. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis 2009;9:91. ArticlePubMedPMC
- 16. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020;277:55−64.ArticlePubMedPMC
- 17. Talevi D, Socci V, Carai M, et al. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr 2020;55:137−44.PubMed
- 18. Korea Disease Control and Prevention Agency (KDCA). Internal report documentof result of survey on the impact of COVID-19 pandemic on TB patients management. Cheongju: KDCA; 2020. Korean.
- 19. McQuaid CF, Vassall A, Cohen T, et al. The impact of COVID-19 on TB: a review of the data. Int J Tuberc Lung Dis 2021;25:436−46.ArticlePubMedPMC
- 20. Kwak SS. News article [Internet]. Seoul: Cheongnyeon-uisa; 2020 Mar 9 [cited 2020 Mar 9]. Available from: https://www.docdocdoc.co.kr/news/articleView.html?idxno=1078309. Korean.
- 21. Zumla A, Marais BJ, McHugh TD, et al. COVID-19 and tuberculosis-threats and opportunities. Int J Tuberc Lung Dis 2020;24:757−60.ArticlePubMed
- 22. Ministry of Health and Welfare. Press release [Internet]. Sejong, KR: Ministry of Health and Welfare; 2020 Mar 13 [cited 2021 Sep 6]. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=80&CONT_SEQ=353539. Korean.
- 23. Min J, Kim HW, Koo HK, et al. Impact of COVID-19 pandemic on the National PPM tuberculosis control project in Korea: the Korean PPM monitoring database between July 2019 and June 2020. J Korean Med Sci 2020;35:e388.ArticlePubMedPMC
- 24. Richards M, Anderson M, Carter P, et al. The impact of the COVID-19 pandemic on cancer care. Nat Cancer 2020 May 20 [Epub];https://doi.org/10.1038/s43018-020-0074-y.Article
References
Figure & Data
References
Citations

- A Review of the Impact of Patent Medicine Vendors in Driving Community Tuberculosis Case Finding in the COVID-19 Pandemic in Nigeria
Arinze Emmanuel Ajogwu, Onwubiko Iheanyichukwu Samuel, Nnanyelugo Longinus Ochike, Uzoma Chidinma Ajegbo, Chinedu Paschal Maduka
Matrix Science Medica.2024; 8(2): 33. CrossRef - Tuberculosis: Republic of Korea, 2021
Jinsoo Min, Hyung Woo Kim, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2023; 86(1): 67. CrossRef - Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study
Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Jeong Mi Seo, Hongjo Choi, Young Ae Kang
BMJ Open.2023; 13(3): e069642. CrossRef - Increased Healthcare Delays in Tuberculosis Patients During the First Wave of COVID-19 Pandemic in Korea: A Nationwide Cross-Sectional Study
Jinsoo Min, Yousang Ko, Hyung Woo Kim, Hyeon-Kyoung Koo, Jee Youn Oh, Yun-Jeong Jeong, Hyeon Hui Kang, Kwang Joo Park, Yong Il Hwang, Jin Woo Kim, Joong Hyun Ahn, Yangjin Jegal, Ji Young Kang, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Time trend prediction and spatial–temporal analysis of multidrug-resistant tuberculosis in Guizhou Province, China, during 2014–2020
Wang Yun, Chen Huijuan, Liao Long, Lu Xiaolong, Zhang Aihua
BMC Infectious Diseases.2022;[Epub] CrossRef - Real-world association of adherence with outcomes and economic burden in patients with tuberculosis from South Korea claims data
Sun-Hong Kwon, Jin Hyun Nam, Hye-Lin Kim, Hae-Young Park, Jin-Won Kwon
Frontiers in Pharmacology.2022;[Epub] CrossRef - The Impact of the COVID-19 Pandemic on Tuberculosis Case Notification and Treatment Outcomes in Eswatini
Hloniphile Victory Masina, I-Feng Lin, Li-Yin Chien
International Journal of Public Health.2022;[Epub] CrossRef - Trends in incidences of newly notified tuberculosis in Jeju Province, Korea, 2017-2021
Jinhee Kim, Nam-Hun Kang, Jong-Myon Bae
Journal of Medicine and Life Science.2022; 19(3): 103. CrossRef
- Figure
- Related articles
-
- Epidemiological characteristics of carbapenemase-producing Enterobacteriaceae outbreaks in the Republic of Korea between 2017 and 2022
- Vaccine effectiveness and the epidemiological characteristics of a COVID-19 outbreak in a tertiary hospital in Republic of Korea
- Preparedness for the next wave of COVID-19 in the Republic of Korea
- Epidemiological characteristics of varicella outbreaks in the Republic of Korea, 2016–2020


 PubReader
PubReader ePub Link
ePub Link Cite
Cite