Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 12(1); 2021 > Article
-
Original Article
Impact of Mixed Cognitive Intervention Training on Early Onset Dementia - Bo-Ra Jeona, Deok-Ju Kimb
-
Osong Public Health and Research Perspectives 2021;12(1):29-36.
DOI: https://doi.org/10.24171/j.phrp.2021.12.1.05
Published online: February 23, 2021
aDepartment of Occupational Therapy, Graduate School, Cheongju University, Cheongju, Korea
bDepartment of Occupational Therapy, College of Health and Medical Sciences, Cheongju University, Cheongju, Korea
- *Corresponding author: Deok-Ju Kim, Department of Occupational Therapy, College of Health and Medical Sciences, Cheongju University, Daesung-ro 298, Cheongwon-gu, Cheongju, 363-764 Korea, E-mail: dj7407@hanmail.net
©2021 Korea Disease Control and Prevention Agency
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- The aim of this study was to investigate the impact of mixed cognitive intervention training using spaced retrieval training, and errorless learning in participants with early onset dementia. This was based on reality orientation therapy for cognitive function, depression, and occupational performance of patients.
-
Methods
- Two early onset vascular dementia patients (> 65 years) with mild or moderate impairment were enrolled in a pre-test - post-test single-subject research design study. Prior to the study, the caregivers were interviewed about meaningful times, people, places, and areas of interest for the participant. A list of individual training words were selected based upon this information, and the participant was instructed to recall them after a 45-second, 90-second, 6-minute, and 12-minute delay. Baseline (3 sessions), intervention (20 sessions), and a second baseline period (3 sessions) were conducted. Activities of daily living were measured, and cognition was measured using the Consortium to Establish a Registry of Alzheimer’s Disease Korean version, whilst depression was measured using the Korean Form Geriatric Depression Scale, and task performance and satisfaction measured by the Canadian Occupational Performance Measure.
-
Results
- After intervention, both participants showed improvements in activities of daily living (ADL), word list memory/recognition, trail making A, occupational performance, and satisfaction improvement, which was clinically significant in 1 participant who also had a reduced score in the scale of depression classifying him as not depressed.
-
Conclusion
- Spaced retrieval training and errorless learning based on reality orientation therapy is an effective intervention in patients with early onset dementia and mild or moderate impairment.
- As a result of the rapid aging of populations worldwide (attributed to advances in modern medicine, and an improved standard of living), the human lifespan has expanded, and the prevalence of geriatric diseases is increasing. Dementia was reported to account for 9.4% of the prevalence of geriatric diseases in 2013 [1]. Dementia is a term which describes progressive neurological disorders, and it begins with short term memory loss, and is characterized by a deterioration of overall cognitive function, and higher mental functions. As the dementia progresses, patients show an array of behavioural symptoms such as depression, hallucinations, delusions, aggressive behavior, anxiety, and wandering, along with exacerbation of emotional swings, loss of willpower, and depression [2,3].
- Dementia is considered a geriatric disorder that induces temperamental changes in the brain as a result of advanced age and aging. However, the 2010 Korea National Health and Nutrition Examination Survey reported an increasing incidence of dementia among middle aged adults under 65 years, and in 2017, patients under the age of 65 accounted for 9.7% of all dementia patients who had received care [4]. Dementia that occurs in middle aged adults under the age of 65 years is referred to as early onset dementia, and as with geriatric dementia, Alzheimer’s disease accounts for 1/3 of cases of dementia, with other types of dementia including vascular dementia, and frontotemporal dementia, frequently manifesting in early onset dementia [1,5].
- Early onset dementia is often mistaken as other conditions or diseases, such as depression or stress-induced diseases, and this hinders early diagnosis [6,7]. In addition, a variety of behavioural, cognitive, neurological, and psychiatric symptoms develop along with memory(particularly short-term memory) deterioration, depression, and anxiety. In the early stages, memory problems may not be conspicuous, but symptoms such as hallucinations, delusions, problems with word selection, and attention disorder may manifest and be more noticeable. Furthermore, compared with geriatric dementia, early onset dementia is reported to progress more rapidly and with more serious problematic behaviour [8,9]. Patients with early onset dementia undergo challenges in their daily living, and their self-efficacy, and values are critically impaired such as losing their social roles in the family or society [10,11]. In addition, limited social services for early onset dementia may cause patients and families to feel isolated, and because early onset dementia develops at an economically and socially active age, productive activities may be limited and have a wide-ranging impact on their lives and their families compared with geriatric dementia [1,10]. Despite the need for early intervention for these patients, research into early onset dementia in Korea is inadequate compared with geriatric dementia.
- Dementia is treated with pharmacological and non-pharmacological therapies, and an appropriate combination of both modalities produces the best outcomes [12]. As a nonpharmacological therapy for dementia, cognitive stimulation is gaining traction, and there are several validated types of cognitive stimulation training, including reality orientation therapy (ROT), spaced retrieval therapy (SRT), and errorless learning. ROT is the most widely used cognitive stimulation for dementia patients. It was first introduced in the US for older adults in hospital with dementia, and it involved repeatedly answering questions about orienting information such as times, places, and person, such that dementia patients could remember and understand their day to day environments, and recent events [13,14]. SRT is a technique in which patients are encouraged to recall information repetitively over progressively longer intervals of time, and the technique does not require many cognitive factors but uses implicit memory instead [13]. Errorless learning was designed for optimized learning in individuals with intellectual disability and memory impairment to prevent learning by trial and error (Baddeley and Wilson [15]). It is used as memory training for dementia patients, and is a technique involving early prompting to ensure an error does not occur in the early stages of learning, by minimizing implicit interferences in the initial learning process. Furthermore, it is often used in combination with SRT as opposed to being implemented alone [16].
- Grandmaison and Simard [17] reported that combining SRT and errorless learning is the most effective compared with each individual technique, and Jean et al [18] reported statistically significant positive changes in cognitive function in patients with mild cognitive impairment by administering face-name association training that integrated SRT and errorless learning. SRT is an effective individualized intervention that improves cognitive function and behavioural symptoms in dementia patients, helping them remember recent events and environments that are meaningful to them including current affairs, scheduling a daily routine, time, and place [19]. In Korea research into the integration of SRT and errorless learning is limited. Repetitive cognitive training at home is essential, but many studies have developed programs to be run under the guidance of an instructor. There are a lack of studies that have designed programs enabling training at home for repeated use [13,20].
- Therefore, this study aimed to investigate the impact of a mixed intervention program involving SRT, and errorless learning based on ROT (meaningful times, people, and places to an individual) to determine cognitive function, depression, and occupational performance of patients with early onset dementia to report foundation data useful in the development of easy home-based programs in the future.
Introduction
- 1. Participants
- This study was conducted on 2 patients under the age of 65 who had been diagnosed with vascular dementia and mild or moderate impairment [using the clinical dementia rating (CDR) 5 point scale and the Mini-Mental State Examination-Korean (MMSE-K) scores] at a dementia centre in the North Chungcheong Province (August to October 2019). The study was reviewed for ethical considerations by the institutional review board at the Cheongju University, and written informed consent was obtained from the participants prior to beginning the study. The inclusion criteria were as follows:
1) Diagnosis of dementia by a psychiatrist or neurologist.
2) Early onset dementia (under the age of 65 years).
3) CDR score ≤ 2 (CDR 0, none; 0.5, questionable; 1, mild; 2, moderate; 3, severe impairment).
4) No hearing or visual impairments, and capable of communication.
5) Capable of recall for more than 45 seconds.
6) Patient’s and caregiver’s written informed consent given to participate in the study.
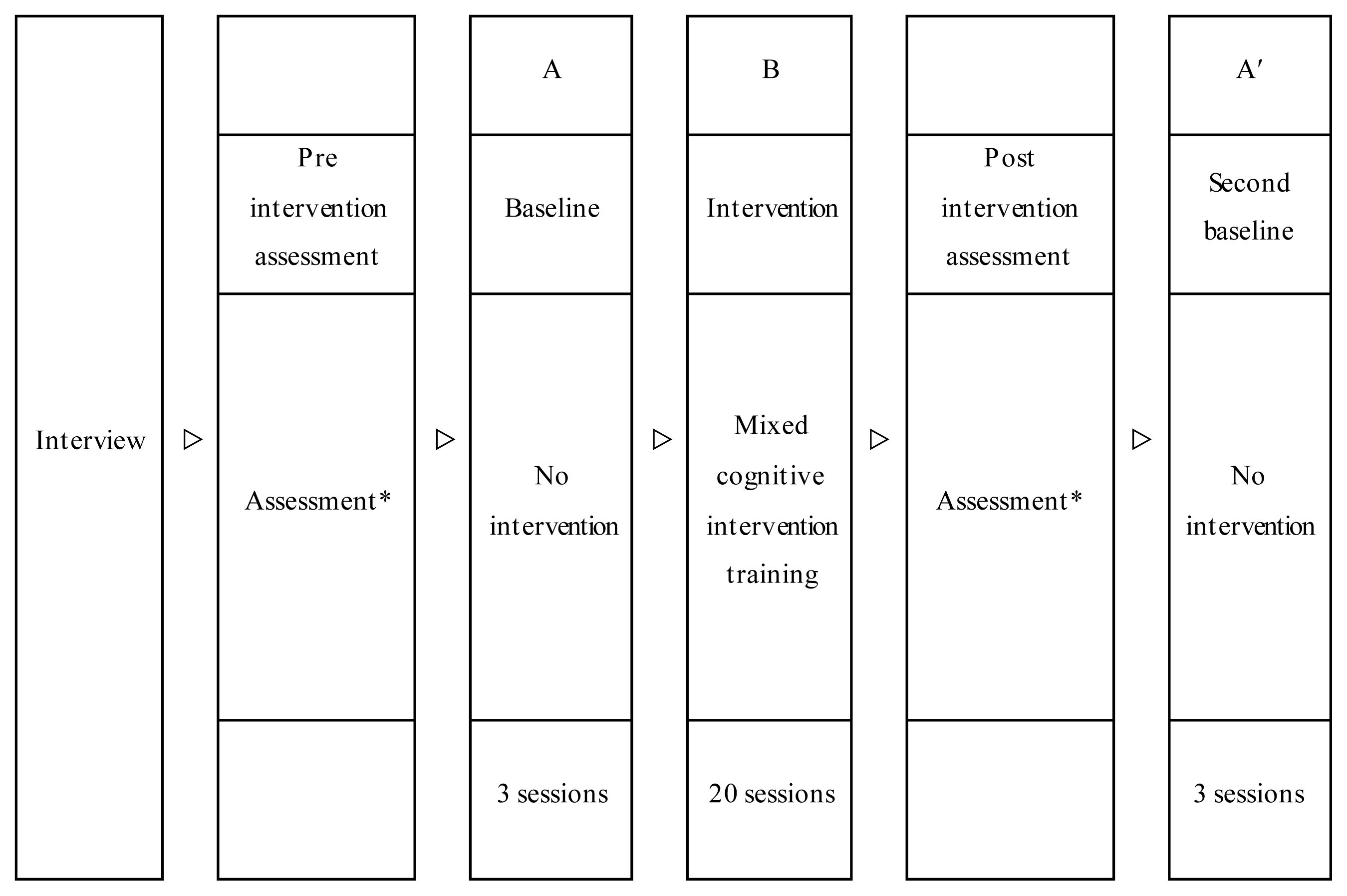
- 2. Study design
- This study used the pre-test - post-test single-subject research design (ABA’), and a total of 26 sessions consisting of 3 sessions at baseline (A), 20 sessions of intervention (B), and 3 sessions of a second baseline period (A’) were conducted (Figure 1).
- The program was modified as determined by the participant and therapist considering Korean culture, and the topic of the session was chosen from person, place, time, and area of interest every week. To structure the training program, participants’ information were obtained via caregiver interviews prior to the study, and the study was conducted over a 4-week period. The program was designed to include topics on personal orientation (my family) in Week 1, time orientation (season) for Week 2, place orientation (my neighborhood) in Week 3, and my areas of interests or social issues for Week 4 (Tables 1 and 2).
- The participants were shown words about the topic and were instructed to recall the words over an interval of 45 seconds, 90 seconds, 6 minutes, and 12 minutes. The duration of recall was recorded. Furthermore, to examine the performance of activities of daily living (ADL) at baseline, intervention, and second baseline periods, the participants were given 6 picture cards for the tasks in 2 areas in the Canadian Occupational Performance Measure (COPM) and were instructed to list them in order. The number of correctly listed cards were recorded and converted to a percentage.
- 3. Measurements
- Cognitive function was measured using the Consortium to Establish a Registry of Alzheimer’s Disease-Korean version (CERAD-K). The CERAD was originally developed in 1989 in the United States for the diagnosis of Alzheimer’s disease and was adapted and modified into Korean in 1994. While it was originally developed to diagnose and assess Alzheimer’s disease, its application subsequently extended to the diagnosis of other types of dementia, including vascular dementia, dementia with Lewy bodies, Parkinson’s disease dementia, and frontotemporal dementia. The tool assesses individual cognitive function, such as memory, language, and spatio-temporal ability. The test-retest reliability ranged from 0.63 to 0.87 [21].
- Depression was measured using the Korean Form Geriatric Depression Scale (K-GDS). The GDS, developed by Yesavage et al [22], is a 30-item yes-or-no instrument, and 2 psychiatrists and 2 clinical psychologists modified and adapted it into Korean using vocabulary and routine expressions appropriate for and easily understood by older adults in Korea. Each of the 30 items is scored with a 0 or 1. A score of 16–22 indicates borderline and mild depression, a score of 23–25 moderate depression, and score of ≥ 26 severe depression. The internal consistency was 0.88 and split-half reliability was 0.79 [23].
- Changes in occupational performance and satisfaction were examined using the COPM. The COPM assesses changes in self-perception after treatment, and it promotes treatment participation by involving the participants in occupational therapy early in intervention. The assessment is performed by choosing meaningful work via an interview prior to the intervention, and level of importance and satisfaction are rated on a scale from 1–10. After the intervention, level of importance and satisfaction are rated using the same method. A change of score of 2 or higher after the intervention is regarded clinically significant [24]. The test-retest reliability was 0.84 [25].
- 4. Statistical analysis
- The mean performance of ADL was analyzed with descriptive statistics. Changes in the performance of ADL were visually presented using a graph, and changes in the CERAD-K, the K-GDS, and the COPM scores after the intervention were presented using bar graphs.
Materials and Methods
3.1. Cognitive function
3.2. Depression
3.3. Occupational performance and satisfaction)
- 1. Participant characteristics
- The participants’ general characteristics are presented in Table 3. Participant 1 was a 58-year-old male diagnosed with vascular dementia. His CDR score was 1, indicating mild dementia, and his MMSE-K score was 18, which indicated definite dementia. Participant 2 was a 51-year-old male also diagnosed with vascular dementia. His CDR score was 2, indicating moderate dementia, and his MMSE-K score was 16, which indicated definite dementia.
- 2. Changes of cognition after the intervention
- Changes of the CERAD-K after the intervention are presented in Table 4. Participant 1 scored higher in the word list memory, word list recognition, constructional recall, trail making A, stroop test, color, and color-word tests after the intervention. Participant 2 scored higher in the word list memory, constructional praxis, word list recognition, and trail making A tests after the intervention, and he showed a marked improvement in the constructional praxis test compared with other tests.
- 3. Changes of depression after the intervention
- The K-GDS results before and after the intervention are presented in Table 5. Participant 1 had a total score of 6 (below 16, indicates a normal level without borderline or mild depression). After the intervention, the total score dropped by 4. Participant 2 had a total score of 18 before the intervention, which indicated mild depression. After program participation, the score dropped by 4, indicating a normal level.
- 4. Changes of occupational performance after the intervention
- The COPM results before and after the intervention are presented in Table 6. For Participant 1, washing hair and going to the toilet were chosen as the assessment items based on the caregiver interview, as the caregiver stated that the participant has difficulties completing these activities because he skips some parts of the activities. After the intervention, both performance and satisfaction increased by 1 point. For Participant 2, brushing teeth and finding the bathroom at home were selected as the assessment items based on the caregiver interview, as the caregiver stated that the participant would forget to put toothpaste on the brush or other parts of the activity while brushing his teeth, and also had problems associated with going to the toilet because he could not find the bathroom at home. After the intervention, the performance score increased by 4 points and satisfaction by 3 points, showing a clinically significant change.
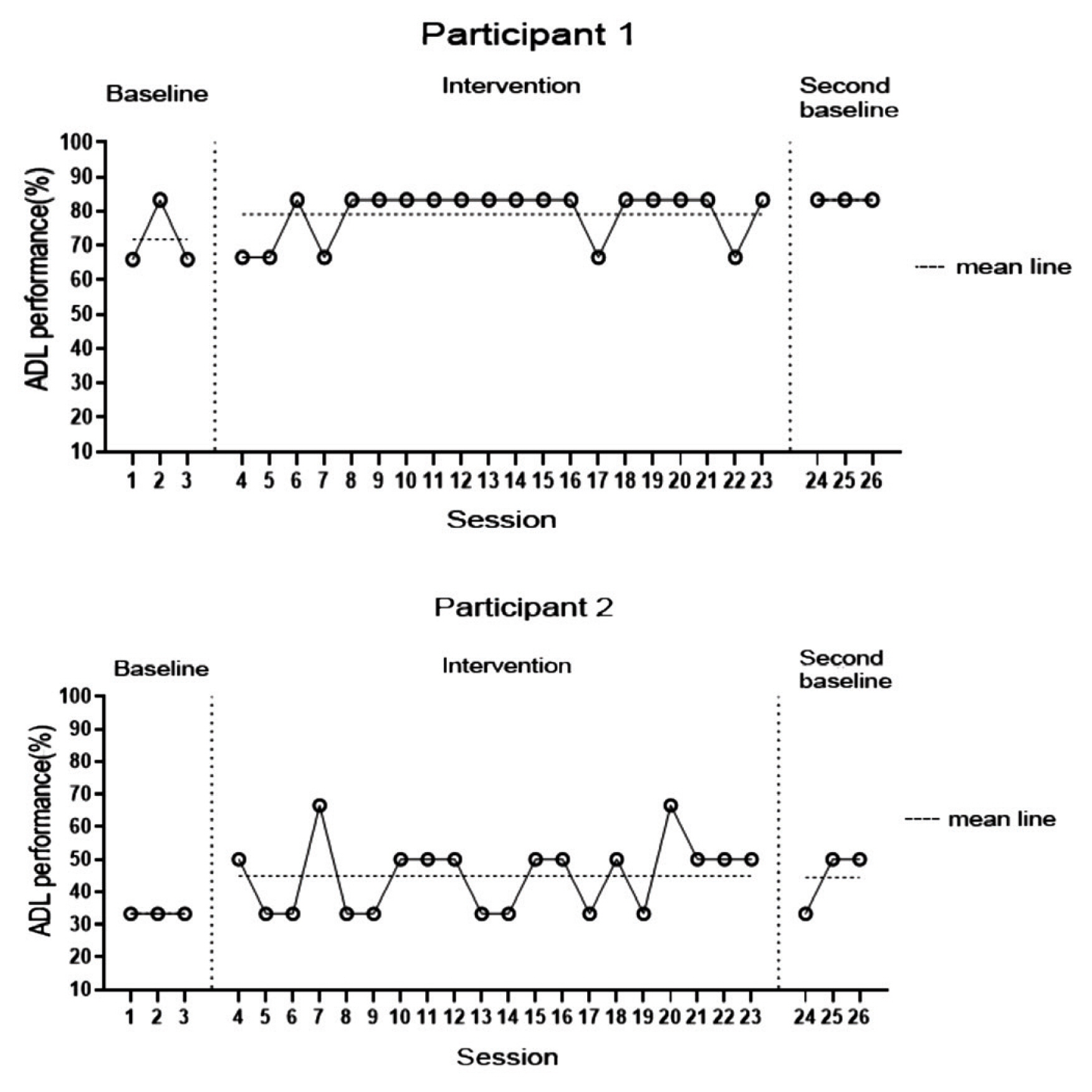
- 5. Changes in performance of ADL
- Changes in the rate of successful ADL performance during the baseline, intervention, and second baseline periods were measured. Participant 1 had a success rate of 71.7% at the baseline, 79.13% during the intervention period, and 83.3% during the second baseline, showing a consistently improving trend. Participant 2 had a success rate of 33.3% at the baseline, but it increased by 11.6% to 44.9% at the second baseline after the intervention. The success rate during the second baseline period was high compared with the mean successful ADL performance rate (Figure 2).
Results
- Dementia that occurs in middle-aged adults under the age of 65 years is referred to as early onset dementia. While memory problems may not be as conspicuous in the early stages, symptoms such as hallucinations, delusions, problems with word selection, and attention disorder may occur. Early onset dementia is reported to be associated with a shorter survival period compared with geriatric dementia and the speed of progression [5,26]. Some studies on early onset dementia report that 56% of these patients have depression, and 71% have anxiety, and because patients in this age group are physically healthy and active, progression to moderate-severe dementia leads to more serious restlessness/aggression, hypersensitivity/instability, abnormal repetitive behaviours, and problematic behaviours compared with geriatric dementia [7,8]. Despite the fact that various interventions could help patients with early onset dementia, provision is needed. Research into early onset dementia in Korea is inadequate compared with geriatric dementia, and programs designed to provide repeated training at home are lacking [10,13].
- In the present study, the impact of a mixed intervention program consisting of SRT and errorless training was investigated. This was based on meaningful reality orientation information for individual patients with early onset dementia to determine their cognitive function, depression, and occupational performance. In terms of the effects of a mixed intervention program consisting of SRT and errorless learning based on reality orientation information, Participant 1 scored higher in the word list memory, word list recognition, constructional recall, trail making A, and stroop test, after the intervention, while Participant 2 scored higher in the constructional praxis, word list recognition, and trail making A tests after the intervention. Participant 1 showed a greater improvement in the scores. In particular, both participants showed a markedly improved score in the constructional praxis test after interventions. In a study examining the changes in level of cognition according to diagnosis of dementia after training consisting of SRT and errorless learning, Jang et al [27] compared the changes of cognition between vascular dementia and Alzheimer’s disease, and observed that the former group had more significant changes in constructional recall, word list recognition, word list recall, and word list memory, which was in line with our findings. In contrast, participants in this current study showed changes in trail making A, which assesses spatiotemporal ability and execution. This may be attributable to the fact that the training program in this current study involved spatiotemporal memory training, such as remembering the locations of shops in the neighbourhood and remembering the layout at home.
- In this current study, the changes in the level of depression in participants after the intervention, was examined. Participant 1 did not have depression at baseline, but he still showed an improved score after the intervention as observed with Participant 2. In terms of the changes in task performance and satisfaction, Participant 1 scored at least 2 points higher after the intervention, which is considered a clinically significant change. The participants also showed increased performance of ADL at the second baseline compared with that at the first baseline. Kauhanen et al [28] reported that stroke patients with depression had statistically significantly poorer cognitive function than stroke patients without depression. Furthermore, in a study on the association between depression, cognitive function, and lesions in patients with vascular dementia, Oh et al [29] observed that physical functioning was not correlated with depression, but it is significantly correlated with language memory, concentration, psychomotor speed, and execution. Yoon and Cho [30] also reported that there were significant changes in depression and performance of ADL after a cognitive rehabilitation program. Thus, the findings in this current study, which are similar to previous findings, suggest that changes in the level of cognition is closely associated with a reduced level of depression [31].
- While this study observed that a program consisting of SRT and errorless learning based on reality orientation information had positive effects on cognitive function, occupational performance, and depression in patients with early onset dementia, this study has a few limitations. Firstly, the findings cannot be generalized due to the small sample size. Secondly, an adequate follow-up study was not performed, so the duration of the therapeutic effects could not be examined. Thirdly, only 2 patients with a mild dementia or moderate dementia were enrolled into the study, so the effects of the program could not be examined by level of cognition. Subsequent studies should recruit a larger sample size and use a controlled experimental design to examine changes in each group, with the addition of adequate follow-up to examine the retention of the positive effects of SRT and errorless learning based on reality orientation information.
- However, the greatest strength of this study was that it provided data on early onset dementia in Korean patients using a mixed intervention program which positively contributed to changes in cognitive function, occupational performance, and depression. We hope that these findings would serve as a foundation for therapists who attempt to develop home-based programs in the future.
Discussion
-
This paper was written by revising and supplementing the first author’s master’s thesis.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
Article information
| Participant 1 | Participant 2 | |
|---|---|---|
| Age (y) | 58 | 51 |
| Sex | Male | Male |
| Education | High school graduate | High school graduate |
| Diagnosis | Vascular dementia | Vascular dementia |
| CDR | 1 | 2 |
| MMSE-K | 18/30 | 16/30 |
| Score | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Participant 1 | Participant 2 | |||||
|
|
|
|||||
| Pre | Post | Change | Pre | Post | Change | |
| KGDS | 6 | 2 | 4 | 18 | 14 | 4 |
| Task | Participant | Score | ||
|---|---|---|---|---|
|
|
||||
| Pre | Post | Change | ||
| COPM-P | 1 | 4.5 | 5.5 | 1.0 |
| 2 | 3.0 | 7.0 | 4.0 | |
|
|
||||
| COPM-S | 1 | 3.0 | 4.0 | 1.0 |
| 2 | 2.5 | 5.5 | 3.0 | |
- 1. National Institute of Dementia. Global trends of dementia policy. National Institute of Dementia; 2018.
- 2. Oh BH. Diagnosis and treatment for behavioral and psychological symptoms of dementia. J Korean Med Assoc 2009;52(11). 1048−54. PMID: 10.5124/jkma.2009.52.11.1048.Article
- 3. Kim SY. Behavioral and psychological symptoms of dementia. Dement Neurocogn Disord 2004;13(1). 14−7.
- 4. Statistics Korea. Discover 2011 polisumer 6 from national statistics. Statistics Korea; 2010.
- 5. Baek SY. [Thesis]. The case study on caregiving experience of family primary caregivers for patients with early onset dementia Seoul (Korea), Hanyang University. 2008.
- 6. Podell K, Torres K. Affective symptoms in early-onset dementia. Neurol Clin 2001;29(1). 99−114. PMID: 10.1016/j.ncl.2010.10.009.Article
- 7. Kaiser S, Panegyres PK. The psychosocial impact of young onset dementia on spouses. Am Alzheimers Dis Other Demen 2007;21(6). 398−402. PMID: 10.1177/1533317506293259.Article
- 8. Sampson EL, Warren JD, Rossor MN. Young onset dementia. J Postgrad Med 2004;80:125−39. PMID: 10.1136/pgmj.2003.011171.Article
- 9. Haase T. Early onset dementia: Clinical and social aspects. Int Psychogeriatr 2009;24(4). 631−6.
- 10. Yoon YJ, Kim EJ, Hong CH. Comparison of behavioral and psychological symptoms between early and late Onset Alzheimer’s disease according to the progression of dementia. Dement Neurocogn Disord 2014;13:89−93. PMID: 10.12779/dnd.2014.13.4.89.Article
- 11. Arai A, Matsumoto T, Ikeda M, Arai Y. Do family caregivers perceive more difficulty when they look after patients with early onset dementia compared to those with late onset dementia? J Geriatr Psychiatry 2007;22:1255−61. PMID: 10.1002/gps.1935.Article
- 12. Omerovic M, Hampel H, Teipel SJ, et al. Pharmacological treatment of alzheimer’s dementia: state of the art and current dilemmas. World J Biol Psychiatry 2008;9:69−75. PMID: 10.1080/15622970701568412.ArticlePubMed
- 13. Hwang JH, Lee KS. Reality orientation therapy and spaced retrieval therapy of the applied of CERAD-K type cognitive rehabilitation programs effects: for mild Alzheimer’s dementia. J Korea Acad Indust Cooperation Soc 2015;16(9). 6201−13. PMID: 10.5762/KAIS.2015.16.9.6201.Article
- 14. Spector A, Woods B, Orrell M. Cognitive stimulation for the treatment of Alzheimer’s disease. Expert Rev Neurother 2008;8(5). 751−7. PMID: 10.1586/14737175.8.5.751. PMID: 18457532.ArticlePubMed
- 15. Baddeley AD, Wilson BA. When implicit learning fails: Amnesia and the problem of error elimination. Neuropsychologia 1994;32(1). 53−68. PMID: 10.1016/0028-3932(94)90068-X. PMID: 8818154.ArticlePubMed
- 16. Kim HS, Kim YW. Non-pharmacotherapy including rehabilitation for dementia. Geriatr Rehabil 2014;4:29−35.
- 17. Grandmaison E, Simard M. A critical review of memory stimulation programs in Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 2003;15(2). 130−44. PMID: 10.1176/jnp.15.2.130. PMID: 12724453.ArticlePubMed
- 18. Jean L, Simard M, Wiederkehr S, et al. Efficacy of a cognitive training programme for mild cognitive impairment: Results of a randomised controlled study. Neuropsychol Rehabil 2010;20(3). 377−405. PMID: 10.1080/09602010903343012.ArticlePubMed
- 19. Spector A, Thorgrimsen L, Woods B, et al. Efficacy of an evidence-based cognitive stimulation therapy program for people with dementia. Br J Psychiatry 2003;183:248−54. PMID: 10.1192/bjp.183.3.248. PMID: 12948999.ArticlePubMed
- 20. Chiu HY, Chen PY, Chen YT, et al. Reality orientation therapy benefits cognition in older people with dementia: A meta-analysis. Int J Nurs Stud 2018;86:20−8. PMID: 10.1016/j.ijnurstu.2018.06.008. PMID: 29960104.ArticlePubMed
- 21. Lee JH, Lee KU, Lee DY, et al. Development of the Korean version of the consortium to establish a registry for Alzheimer’s disease assessment packet (CERADK) clinical and neuropsychological assessment batteries. Psychol Sci Soc Sci 2002;57(1). 47−53.Article
- 22. Yesavag JA, Brink TL, Rosre TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatry Res 1983;17:37−49. PMID: 10.1016/0022-3956(82)90033-4.Article
- 23. Jung IK, Kwak EI, Joe SH, et al. A study of standardization of Korean form of geriatric depression scale. J Korean Geriatr Psychiatry 1998;1(1). 61−72.
- 24. Carpenter L, Baker GA, Tyldesley B. The use of the Canadian occupational performance measure as an outcome of pain management program. Can J Occup 2001;68(1). 16−22. PMID: 10.1177/000841740106800102.Article
- 25. Pan AW, Chung L, Hsin-Hwei G. Reliability and validity of the Canadian occupational performance measure for clients with psychiatric disorders in Taiwan. Occup Ther Int 2003;10(4). 269−77. PMID: 10.1002/oti.190. PMID: 14647540.ArticlePubMed
- 26. Rogaeva E. The solved and unsolved mysteries of the genetics of early onset Alzheimer’s disease. Neuromolecular Med 2002;2(1). 1−10. PMID: 10.1385/NMM:2:1:01. PMID: 12230301.ArticlePubMed
- 27. Jang JS, Lee JS, Kim SK, et al. The change in spaced retrieval training (SRT) combined with errorless learning on cognitive function and depression in dementia sufferers. J Korean Soc Occup Ther 2012;20(4). 43−55.
- 28. Kauhanen ML, Korpelainen JT, Hiltunen P, et al. Poststroke depression correlates with cognitive impairment and neurological deficits. J Am Heart Assoc 1999;30(9). 1875−80.Article
- 29. Oh EA, Kang YW, Kim JH, et al. Relationships among depression, cognitive functions, and lesion sites in vascular dementia. Korean J Clin Psychol 2005;1:448−9.
- 30. Yoon JA, Cho YN. Effect of cognitive occupational therapy programs for community-dwelling elderly with dementia. J Occup Ther Aged Dement 2009;3(2). 33−43.
- 31. Son EG, Lee JS. Canadian occupational performance measure. 3rd ed Revised. Seoul (Korea): Jungdam; 2001. pp 67−72.
References
Figure & Data
References
Citations

- Non‐pharmacological interventions for people living with young‐onset dementia and their carers: A scoping review focussing on the support of participants' needs
Iktae Kim, Yoosun Yang, Hongjin Cheon, Jiyeon Kim, Jun‐Ah Song
Journal of Psychiatric and Mental Health Nursing.2024; 31(1): 14. CrossRef - Interventions for Persons with Young-Onset Dementia and Their Families: A Scoping Review
Xiaoyan Cui, Junqiao Wang, Bei Wu, Qianhua Zhao, Xueting Tang, Jing Wang
Journal of Alzheimer's Disease.2024; 97(4): 1519. CrossRef





 PubReader
PubReader ePub Link
ePub Link Cite
Cite


