Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 11(5); 2020 > Article
-
Original Article
Primary Healthcare Under Transformation in 3 Eastern European Countries: Quality Satisfaction as Rated by Students - Sviatlana Ahiyevetsa, Andrei Shpakoub, Joanna Baj-Korpakc, Ewa Kleszczewskad, Katarzyna Rzatkiewiczd, Krzysztof Mancewicze, Valentina Stetsenkof, Semen Stetsenkog
-
Osong Public Health and Research Perspectives 2020;11(5):286-295.
DOI: https://doi.org/10.24171/j.phrp.2020.11.5.04
Published online: October 22, 2020
aInstitute of Legal Research, National Centre of Legislation and Legal Research of the Republic of Belarus, Minsk, Belarus
bYanka Kupala State University of Grodno, Grodno, Belarus
cPope John Paul II State School of Higher Education Department of Physiotherapy, Biała Podlaska, Poland
dEdward F. Szczepanik State School of Higher Professional Education in Suwałki, Suwałki, Poland
eUniversity of Medical Science in Bialystok, Bialystok, Poland
fNational Pedagogical Drahomanov University, Кiev, Ukraine
gSupreme Court, Kiev, Ukraine
- *Corresponding author: Andrei Shpakou, Yanka Kupala State University of Grodno, Grodno, 230023, 22 Ozheshko str. Belarus, E-mail: shpakofff@tut.by
• Received: February 19, 2020 • Revised: July 1, 2020 • Accepted: July 5, 2020
Copyright ©2020, Korea Centers for Disease Control and Prevention
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- This study aimed to determine the reasons for student dissatisfaction with the quality of primary healthcare (PHC) in countries under healthcare system transformation (Belarus, Poland, and Ukraine) to identify reserves and make improvements.
-
Methods
- A comparative multipopulation survey was translated, verified, and completed during face-to-face interviews during March 2019 to May 2019. There were 700 Humanities students included in this study to determine satisfaction with the quality of PHC provided by the family doctor. Satisfaction was assessed according to the availability of the doctor, the level of organization of the institution, the service process, the quality of the interaction with the doctor, adherence to the rights of patients, and any additional financial expense incurred by the patient.
-
Results
- Politeness and attentiveness of doctors were rated highly. Dissatisfaction was associated with the negative attitude of medical personnel towards the patient. One in 10 respondents replied that medical confidentiality was not observed. More than 65% of students had paid for diagnostic tests/or treatments, and some respondents from Poland and Ukraine were asked by the doctor to pay for services without a receipt.
-
Conclusion
- Dissatisfaction with the quality of PHC in countries under transformation of the health system was largely due to ethical aspects of the doctor-patient relationship. Therefore, ethical standards need to be upheld and patients need to be aware of these standards using medical education materials covering the moral aspects of the relationship between medical personnel and patient.
- Keywords: primary healthcare; students; satisfaction
- One of the most important conditions for reforming and modernizing a healthcare system is the requirement to respect the rights of citizens to receive affordable and qualitative primary healthcare (PHC) [1]. Among the priorities are achieving improved health and reducing inequalities in public health, meeting the expectations of patients which include showing personal (dignity, confidentiality and self-sustainment), and professional (due care and attention, provision of affordable and quality services) respect [2,3]. PHC largely determines the effective functioning of the healthcare system [4,5]. According to the World Health Organization (WHO), PHC is a set of interconnected measures promoting health, sanitation, treatment and prophylactic approaches, implemented at the citizen’s primary contact with the healthcare system. It accounts for prevailing and emerging environmental conditions, and lifestyle, and is aimed at preserving, restoring, and promoting health. This type of care embodies the basic values and principles (affordability of medical and sanitary services, comprehensive examination of patients, coherence in working with other services and departments, continuity in the monitoring of patients in various healthcare organizations, targeting to provide medical, social, and psychological assistance) [6–8].
- Treatment effectiveness has been reported to hold considerable importance in the association between service quality and satisfaction, and a greater effect on satisfaction, compared with facilities and environment [9].
- Patient satisfaction depends on many factors. The promotion of patient’s overall satisfaction with medical service delivery, the improvement of doctor-patient communication, the reduction of medical costs, the improvement of the medical treatment process, the promotion of the medical facility and hospital environment, the reduction of waiting times for medical services, the promotion of patients’ trust in prescriptions, the promotion of patients’ trust in doctors, and the promotion of patients’ trust in recommended medical examination could all help promote patients’ life satisfaction [10]. Patient satisfaction in terms of gender and age variables has been reported to be significant, but it was not significant with regards to education, career, inpatient ward, insurance, and residence variables [11]. Hospital managers can take specific measures to promote patient satisfaction by removing the elements causing dissatisfaction.
- In the context of this current study, PHC is considered as the process of providing healthcare during the patient’s initial request to the healthcare system, which is implemented mainly by family doctors. Access to family medicine is determined by the legislation of each country in this study. However, it is simple and generally provides good opportunities to receive healthcare.
- Despite the fact that in Europe the priority for reforming the healthcare system is to improve services in the PHC system with increased funding, the initial prerequisites, reasons and methods for implementing reforms, differ [12,13]. The countries of Central and Eastern Europe, as well as the countries that were formerly part of the Soviet Union, are trying to fundamentally improve general and PHC functioning and increase the economic efficiency of their healthcare systems [14,15]. PHC as the primary element of medical care, previously in the countries of the post-socialist era, developed under conditions of rigid centralization. Currently, countries are striving to increase the economic efficiency of the system and provide adequate medical care [16,17]. These changes for countries such as Belarus and Ukraine follow an evolutionary path, which implies a delay in the implementation of healthcare reforms [18–24].
- The main purpose of the reform in Ukraine is to objectify the process of providing medical care at the primary level, to “tie” its provision to the subsequent financing of the medical services provided, and to improve control over the spending of funds allocated to protect the health of citizens. For this purpose, a special body was created - the National Health Service of Ukraine. To date, the National Health Service of Ukraine has signed an agreement with more than 1,500 medical institutions that provide PHC. Those hospitals which have not signed the agreement will not receive funding from the government, which will potentially lead to closure. On April 1st 2020, a new stage of reform began involving the signing of agreements with medical institutions which will provide secondary medical care. The transition of PHC to the principles of general practice (family medicine) is the main direction of the reform of the Ukrainian national healthcare system. Current legislation determines that the provision of PHC is provided by healthcare institutions and individuals/entrepreneurs who have received the appropriate license in the manner prescribed by law. PHC is provided by general practitioners/family doctors, doctors of other specialties and other medical staff working under their supervision [25]. According to the reforms, in Ukraine from January 1st, 2020, PHC was to be provided by a family doctor. However, political, socio-economic and ideological factors (non-recognition by the medical community and patients of the proposed changes) lead to an increase in problems in the current healthcare system. As of the beginning of 2019, reforms including elements of decentralization of health management, the formation of the institution of family doctors, changing the basic principles of financing the healthcare system were consolidated [21].
- Now there are positive trends in streamlining the use of medical institutions but nevertheless, the speed and quality of the ongoing reforms have not yet fully justified social expectations [26]. Reforms are not always based on evidence, and progress in these countries often depends on political sway or the interests of specific professional groups, rather than justified assessments [27].
- The strict hierarchical and centralized organization of the healthcare system in Belarus still has features of the former centralized system. The principles of financing and managing the healthcare system remain virtually unchanged. Privatization of services in the healthcare sector or delegation of authority to private entities are fragmented. Unlike other countries in the region, after gaining independence, Belarus does not have revolutionary changes in the healthcare system and PHC. No immediate fundamental reforms have been undertaken and innovations were introduced on a limited scale and restricted to regions and experimental sites, and not on a national scale [28]. Nevertheless, in Belarus, specific decisions were made to reduce the volume of inpatient care and increase the volume of primary care. In Belarus, this is the main type of healthcare accessed for common diseases, during pregnancy and childbirth, during diagnostic testing and medical prevention [24]. Until now, PHC in cities was mainly provided by the district physicians pediatricians, as well as highly-specialized medical specialists working in polyclinics. In rural areas, there were 2 types of PHC facilities: dispensaries and feldsher-midwife posts. In dispensaries, assistance was provided by district general practitioners for adults or pediatricians for children (or occasionally general practitioners who have undergone retraining).
- In recent years, the gradual approach to general medical practice continued with the organization and implementation of the work by the district service run by a family doctor/general practitioner and a team (doctor’s assistant, and general practitioner nurse). The content of the work of the primary care physician is much closer to the content of the work of a family doctor/general practitioner or, who is the main representative of primary care in healthcare systems in most countries of the world. The WHO recommends the use of the terms general practitioner (undertakes appointment of the attached population according to the territorial principle) and family doctor (observes families) as equivalent [29]. It is planned that in 2020 PHC physicians will completely replace general practitioners in Belarus.
- Major changes in the national healthcare system of Poland were carried out in 1999. Then, instead of a system based on financing public health with taxes (Tax-funded National Health Service), a decentralized social health insurance system was introduced. In 2003/2004 there was the return to centralization (the National Health Fund was created). Since 2016, the Ministry of Health has launched a program of healthcare system reform aimed at improving access to healthcare, coordination, efficiency and reducing duplication [30].
- The material of this multicenter study involved a structured review of the strengths and weaknesses of the PHC organization model, based on the views of university students. This category of the population was chosen because of the relatively rare access to PHC. Focus was on the choice of students as a separate category of the population representing youth, mobility, and social activity enabling leadership of countries to predict ways to improve the protection of public health to improve the quality and accessibility of medical care.
- This study aimed to determine reasons for the perceived dissatisfaction with the quality of PHC in countries undergoing transformation of their health systems, identifying reserves, and determining ways to improve it based on the comparative survey of students in Belarus, Poland, and Ukraine. In these countries, health legislation and the health system are being reformed at different speeds.
Introduction
- 1. Study design and setting
- During the period from March 2019 to May 2019, a sociological study was conducted in Humanities students from 3 countries (Belarus, Poland, and Ukraine). The main perceived factors (according to respondents) which affected their satisfaction with PHC were identified, and the quality, and the availability of the doctors in the PHC in their country of residence was examined. This study was approved by the local ethics committee of Yanka Kupala State University of Grodno (no.: N12-1, 2019).
- 2. Participants
- There were 700 students from the university of Grodno and Minsk (Belarus), Bialystok, Suwalki and Biala Podlaska (Poland), and Kiev (Ukraine), who anonymous questionnaire on satisfaction with the quality of medical care provided by a family doctor (general practitioner, primary care physician) which had previously been tested in a pilot study indicating sufficient test-retest reliability of the data could be obtained.
- Students were approximately the same age and studying humanities. They answered identical questions from the same questionnaire. Thus, the sample structure met the requirements for this research, and the sample itself was representative.
- 3. Variables
- The satisfaction of respondents was assessed according to the availability of doctors in the PHC and the level of organization of the institution, the degree of satisfaction with the service process, the quality of personal contact with the doctor, the rights of patients observed by medical personnel, as well as the presence (absence) of additional financial expenses incurred by the patient.
- 4. Descriptive data
- The present study was a comparative multipopulation survey. A multilingual and multinational study with descriptive analysis of data collected in 2019 from humanities students in Poland, Ukraine and Belarus.
- 5. Data collection instruments
- The questionnaire was translated into the languages of the respective countries, and the translation was double-checked. Initially, the document was translated into the state language, and expert comments were received on the wording of questions about PHC. Then the text was reverse translated and verified. The study used non-repeated random sampling whereby a respondent answered the questionnaire only once. The poll was conducted in full-time and part-time students forums. In face-to-face polls, the questionnaire was filled out by interviewers, whilst in absentia the respondents independently answered the questions on paper or in an electronic form.
- 6. Statistical analysis
- Quantitative parameters were represented by average scores, and qualitative ones as a percentage. In a comparative analysis of quantitative indicators the Student t test for the symmetric (normal) distribution of variables was used, and the Mann-Whitney U-test and Kruskal-Wallis H-test was used for asymmetric (skewed distribution). The distribution of qualitative variables was presented as a percentage, with 95% confidence at intervals, and statistical comparisons were performed using independent Chi-square analyzes. The critical significance level (p) when testing statistical hypotheses was assumed to be 0.05. The statistical analysis included data from 90% of the proposed questionnaires. The criteria for the exclusion of a respondent from the study was the answer “Never during the year” to the question “When did you last go to the local doctor (general practitioner, family doctor)?” and blanks on the forms. A total of 631 cases were entered into the database and processed.
Materials and Methods
- 1. Participants
- In total, 631 profiles were entered into the database and processed (Grodno n = 109, Minsk n = 82, Bialystok n = 100, Suwalki n = 108, Biala Podlaska n = 138, Кiev n = 94). By country: Belarus n = 191, Poland n = 346, Ukraine n = 94. The distribution by age and gender in each group of respondents is presented in Table 1.
- The average age of the respondents was 21.6 ± 2.41 years (range 18–28 years) without statistical differences between the groups (p > 0.05). Among the respondents there were more women (70.7%) than men (29.3%), and are typical for the Humanity Departments of universities of the 3 countries.
- 2. Main results of the survey
- The students’ perception of the availability of the doctors in the PHC was studied. The time of the last visit to the doctor, and the method of making an appointment. The infrequent visit of students to PHC was confirmed as 84.3% of the respondents who last visited a doctor 1 month ago or more. Recently (during the last month), 15.7% of respondents (more often students from Belarus, less often students from Poland and Ukraine) were seen by a primary physician/general practitioner (Table 2).
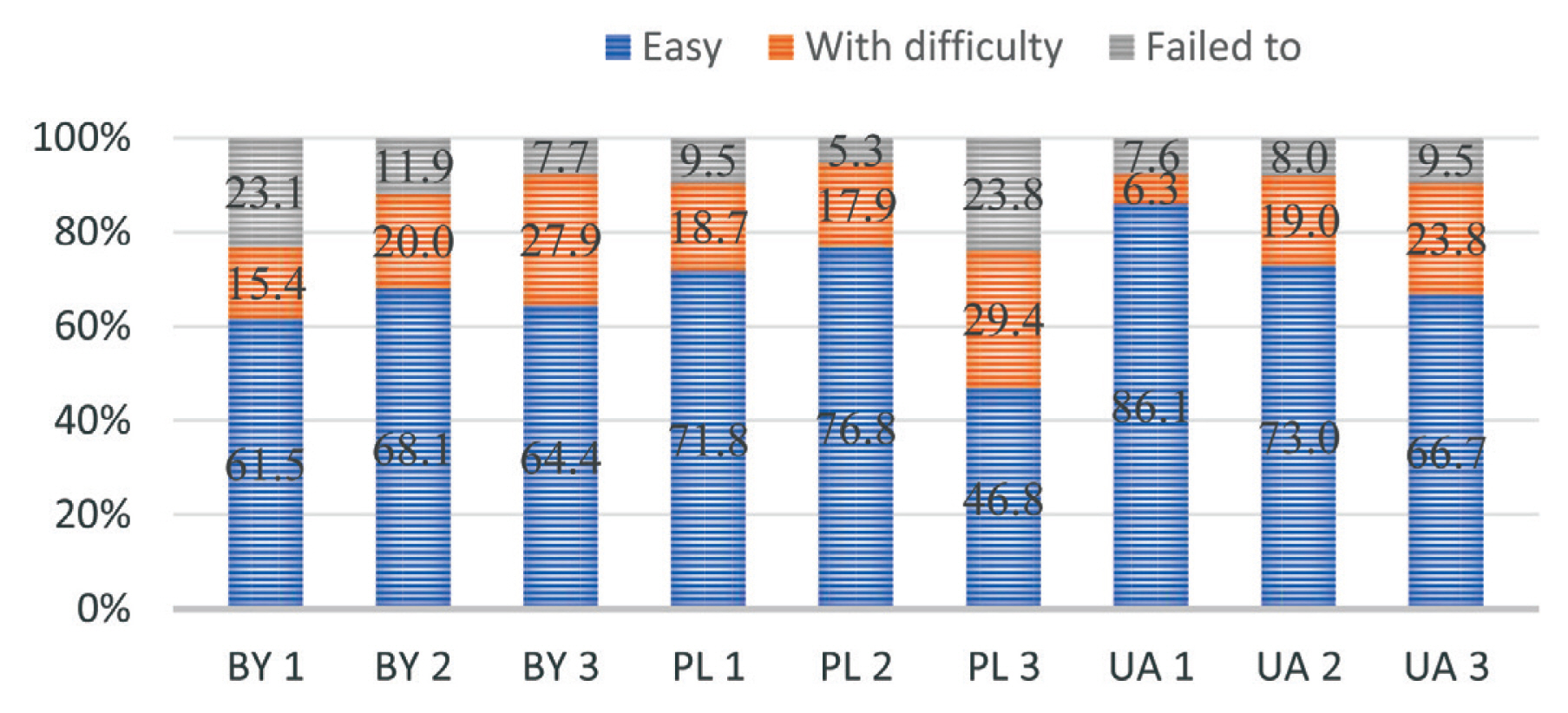
- Respondents used several methods to make a doctor’s appointment. Most often, they registered for an appointment with a doctor by phone (89.4%). Moreover, they were successful in more than half of the cases. On the first attempt, it was not possible to make an appointment for 13.9% of respondents, and 16.0% of the respondents said that making an appointment to see a doctor by phone was associated with great difficulties. The differences between the groups of respondents from each country were significant (Chi-square 28.3, p < 0.001) mainly due to the significantly larger number of respondents from Belarus who were not able to make an appointment to see a doctor by phone. While in general 82.6% of the respondents managed to make an appointment with the doctor during the first call, in a quarter of cases of Belarusian students they were unable to make an appointment with the doctor on the first attempt. In the other 2 groups, this indicator did not exceed 14%. It is also indirectly confirmed that students from Poland and Ukraine are more satisfied with the availability of a doctor’s appointment for personal visits or telephone consultations, compared with respondents from Belarus. Via personal request to the registry, 79.1% of respondents made an appointment with a doctor, and answered that this was easy to do in more than 70% of cases. On the first attempt it did not work out in 7.8% of cases, while 18.3% of students considered that this was difficult. The groups did not differ significantly. Website registering was not common for most respondents (39.8%). More than half explained the preference for this method because of the ease of registration. In 15.9% of cases, respondents were not able to immediately register via the internet, and 28.3% of students found this method more difficult. The differences between the groups of respondents were significant (Chi-square 13.7, p < 0.01) mainly due to the larger number of respondents from Poland, which either failed to register, or when registering via the internet, encountered significant difficulties. The preferences and possibilities of making an appointment with a doctor in the 3 countries are presented in Figure 1.
- The waiting time for the provision of services satisfied the majority of respondents. Geographic accessibility was high. 70% of the respondents indicated that they spend less than 20 minutes to see a general practitioner or primary care physician. In Belarusian students this indicator exceeded 77%, and among Polish respondents it was 73%. Students in Ukraine took longer. The waiting time for an appointment at the doctor’s did not exceed 20 minutes for 65.1% of students, 16.3% did not have any expectations, and 34.9% expected more than 20 minutes-. There were 66.5% of respondents from Poland who waited for an appointment with a doctor for 20 minutes or more. This indicator among respondents from 2 other countries did not exceed 50% (Table 3).
- The waiting time from appointment to receiving diagnostic tests, and from passing tests to obtaining results in the groups was different. About half of the students (43.5%) spent more than 4 days waiting. Respondents from Belarus differed from their colleagues from Poland and Ukraine by having a more significant waiting period.
- The comfort of the conditions for the provision of services and the availability of a receipt of payment did not satisfy all respondents. Lack of repair in the premises, old furniture, and poor sanitary-technical conditions of premises in 11.2% of cases were cited as the cause of discomfort, and not due to the medical care in general. One out of 10 respondents had difficulty getting a prescription. This concerned students from Ukraine least of all students (3.2%), however it affected significantly more students from Poland (13.0%; p < 0.05).
- The average scores in a comparative analysis of the general assessment of satisfaction with a doctor’s appointment as one of the quality characteristics of PHC were more than 3.5 points in all groups. The courtesy and attentiveness of the doctor was not statistically different between the groups. For a number of factors, there were statistically significant differences in the opinions of respondents. Thus, the average scores characterizing the level and availability of explanations by the doctor and treatment prescribed, as well as the doctor’s identification of changes in health status (taking into account the patient’s complaints and the results of the treatment), were minimal in the responses of the Belarusian student groups. Satisfaction with the medical care provided by the doctor as a whole did not differ in groups and amounted to a median of 4.0 ± 0.83 points (Table 4).
- In general, the level of satisfaction with the quality of medical care was quite high and was within the “good” ratings. The main reasons for dissatisfaction with the result of the medical care provided were mainly related to the carelessness of the doctor towards the patient, rudeness in communication, indifference and irritability (22.5%), as well as difficulties for the patient to receive counseling by a specialist (30.8%), or have extensive laboratory diagnostic and functional research performed (24.9%).
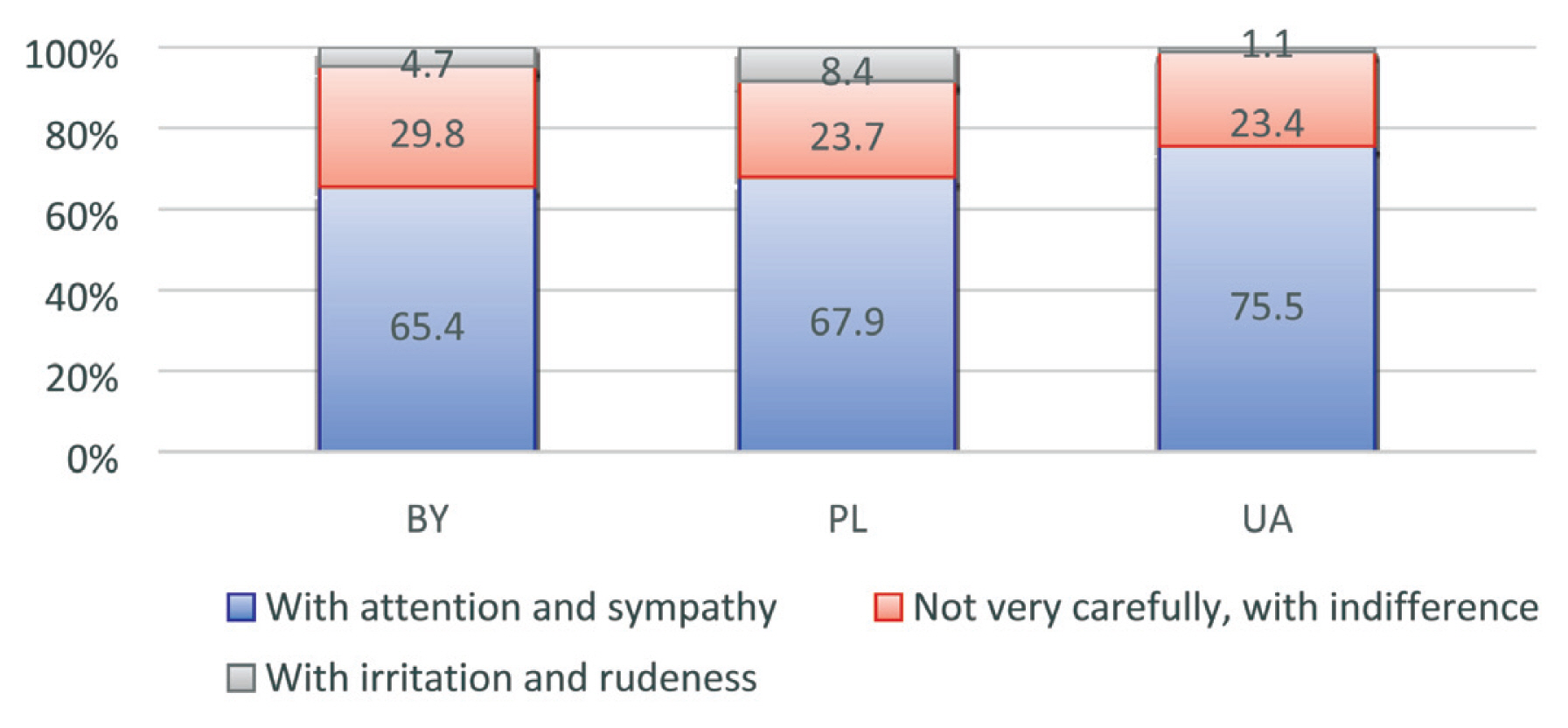
- The degree of satisfaction with PHC experienced by students was determined by factors related to the quality of personal contact with a doctor. The next group of questions was devoted to assessing the perception of the doctors’ function in the PHC system based on communication with the doctors, trust in the doctors, and how the respondents perceived the doctors’ competencies. Experience of communication with doctors was evaluated positively. Most of the respondents answered that doctors devoted enough time to talk, listen attentively, and gave clear explanations about the condition/disease and medications. Representatives of all 3 groups did not differ in assessing the doctors’ attitude towards them. More than 65% of respondents indicated attention and sympathy in communication. In a third of cases, there were negative aspects associated with some inattention, indifference, irritation and even rudeness (Figure 2).
- Indirectly, malevolence in the relationship was confirmed by a more frequent indication of conflicts between the doctor and the patient as reported by the respondents (38.7% among the respondents in Belarus, 20.8% in Poland and 11.7% in Ukraine).
- The prevalence of a hostile attitude on the part of doctors was a problem and needs further study. The ill-will from doctors and the inaccessibility of their explanations increased the relative chances of respondents being dissatisfied with their medical care. Therefore, there is a certain reserve, the elimination of which must be sought by identifying and eliminating the reasons that negatively affect the perception of the quality of medical care by respondents.
- The final part of the questionnaire was concerned with the rights of patients and compliance by medical personnel, as well as the students’ attitudes towards paid medical services. The majority of respondents (more than 63% in all groups) indicated the availability of patient information in medical offices and waiting rooms. To the question: “What do you think, who often allows violations of patient’s rights when providing medical care?” The answers were varied (Table 5), but 1 in 10 people surveyed pointed to examples of a violation of a patient’s rights by a doctor.
- The negative experience of communication with nursing staff and paramedical staff, although statistically significantly associated with satisfaction with medical care, turned out to be insignificant in terms of its influence.
- One in 10 respondents also indicated a lack of medical privacy in their case where professional medical ethics and the legal obligation of the doctor in relation to the patient was not observed. In a group of students from Belarus, 14 (10.5%) students confirmed a lack of medical confidentiality by the primary physician and in Poland and Ukraine it was 7.2% and 14.8% respectively (p > 0.05). All respondents knew that they had the right to receive information on their health status in an accessible form. However, 1 in 10 students were denied such information. The percentage of respondents who did not receive permission to access medical records in the group of students from Belarus was 14.1%, and among students in Poland and Ukraine this did not exceed 8.5%.
- Satisfaction with medical care may be distorted by the need to bear the additional costs associated with treatment. It should be noted that even though students usually turn to their local primary care physician (general practitioner) for assistance, medical assistance can be received in the ambulance, at medical hospitals and through private doctors. There is a growing tendency towards trust in private practitioners (especially among Belarusian respondents). Presumably, this may be because more than 20% of this group answered affirmative to the question “Over the past 12 months, have you experienced difficulties in receiving medical care?”
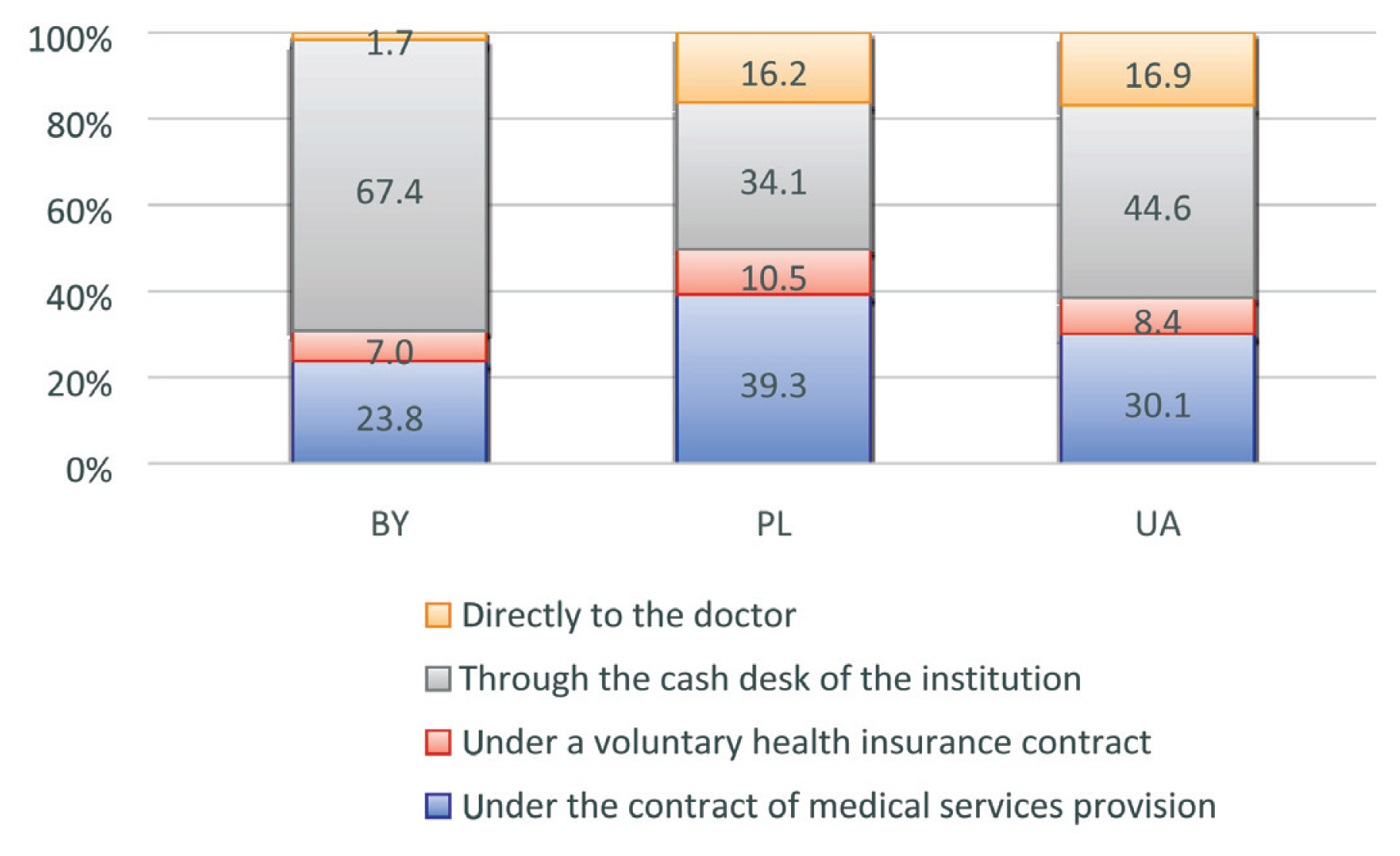
- Two-thirds of respondents indicated that they had to pay for some types of diagnostic tests or treatment methods [88.5% in Belarus, 87.3% in Ukraine and 65.0% in Poland (p < 0.05)]. Among those, 27.8% of Belarusian students paid for physiotherapy treatment. This type of treatment was paid in half the cases in Poland and Ukraine. More than half of the respondents indicated that they paid laboratory tests, and in the group of students from Poland this indicator exceeded 70%. Functional and instrumental research methods were paid in a quarter of observations. More often these types of diagnostics were paid by respondents from Belarus and Ukraine. Among the reasons for the need to pay for the service, in a quarter of cases personal initiative was indicated and in a third of cases it was due to the lack of an offer from a doctor to do it for free. In 40.9% of cases, the doctor offered to do everything for free, but it took longer. The first 2 reasons are most typical for respondents from Ukraine (35.0% and 48.8, respectively), and the third reason is typical for respondents from Belarus (more than half of the observations). The prevalence of the main payment methods is shown in Figure 3.
- More than 16% of respondents from Poland and Ukraine reported that the doctor asked the patient to pay for the service, bypassing the cash register and without documentary evidence of payment.
Results
- The highest satisfaction with the quality of PHC was noted among students from Poland. To a certain extent, this is due to a higher standard of living in Poland, and a greater degree of trust in the organizational models of providing medical care at the primary level, as well as a longer period of reform change. The degree of satisfaction with PHC in students’ assessments of the 3 countries was determined by factors related to the quality of personal contact with a doctor. Therefore, the development of doctors’ communication skills to show respect whilst being effective communicators, and the ability to convey information about the revealed pathology and treatment prospects of the patient (in an accessible form), enables active cooperation with the doctor, and affects the quality of care. It seems appropriate to use medical education materials more widely in the system which are devoted to the moral and ethical aspects of the relationship between medical staff and patients. Interestingly only 63% of students interviewed from Ukraine went to a family doctor (general physician). This may be due to the following reasons: a) the common practice of self-medication; b) a visit to highly-specialized medical specialists directly, bypassing the therapist; c) the presence of shortcomings in the ongoing PHC reform (lack of family doctors in many regions of Ukraine and, as a result of this, the inability for some of the population to conclude a contract and be served by a family doctor). Among students, who have had experience with family doctors, there are clearly positive attitudes and high levels of satisfaction with the medical services provided. This makes it possible to predict the positive outcomes of the ongoing reform, subject to political stability, economic growth, and an established system of financing for the institution of family doctors introduced.
- Satisfaction with PHC quality did not differ in groups (about 4 points). The politeness and attentiveness of the doctors were rated highly. The main reasons for dissatisfaction were associated with the negative attitude of medical personnel towards the patient and the time-consuming process of waiting for the results of laboratory diagnostic tests. Respondents from Belarus more often indicated difficulties in making appointments by phone. One in 10 respondents reported that medical confidentiality was not observed in his case. More than 65% of students answered that they paid for diagnostic tests or treatment methods, and some respondents from Poland and Ukraine replied that the doctor asked them to pay for the service and did not give a receipt.
- The results of this study highlighted that researchers have no consensus on the content of the term “satisfaction with the quality of medical care,” and its characteristics and structural components. This makes it extremely difficult to define quantitative and qualitative criteria. It seems appropriate to widely use medical education materials devoted to the moral and ethical aspects of the relationship between medical staff and patients.
- In the medical care of the population, PHC takes priority, however, it is entrenched in healthcare legislation [30]. According to the Ljubljana Charter on Improving Health Care (adopted in 1996 at a meeting of the WHO Regional Office for Europe, by European Ministers of Health), “any healthcare reform should aim to continuously improve the quality of medical care, as well as increase its effectiveness, and include a clearly developed strategy to achieve this goal” [31]. In the period of fundamental changes of a healthcare system, the importance of measuring satisfaction is increasing.
- Perceived patient satisfaction and quality of care are associated, but it is not necessarily a direct relationship. Satisfaction in general should be observed in a broader context. It reflects the variability of personal resources of the patients, the dynamics of the behavior between personnel they are in contact with, and the nature of the conditions for the provision of medical services. In addition, there are variables that determine the nature of interpersonal relationships in the dialogue between “medical workers and patients.”
- Currently, the attention of research is mainly focused on the characteristics of the relationship between the doctor and the patient. It has been reported that patient dissatisfaction was associated mainly with low emotional support offered by medical personnel, and the patient’s family in the diagnostic process, and a lack of understanding of the reported medical information [32]. At the same time, there is unsatisfactory organization of the case where there is no consistency between the inpatient and outpatient stages of medical care, the timeliness of PHC, and the availability of high-tech types of medical care. This has been reported to lead to dissatisfaction with the waiting time for a doctor’s appointment (75.8%), and the perception of limited knowledge of the patient’s problems by the doctor (74.2%) [32]. The results of this current study of respondents’ satisfaction with PHC quality indicated that researchers need to reach a consensus on the content of the term “satisfaction with the quality of medical care,” a list of its characteristics, and structural components to define and systematize, quantitate and qualify criteria. The most significant factor in patient satisfaction was determined to be the respectful and attentive attitude of medical personnel [33].
- Medical ethics set out to regulate the relationship between a doctor and a patient and it has been suggested that medical ethics should become a potential source of the law [34]. We propose consideration of such innovations and propose that this could be among other factors influencing the satisfaction of patients with the quality of PHC.
- The quality, accessibility, and effectiveness of various models of primary care organizations needs further study, and scientific substantiation for optimizing management decisions. It is important not to mechanically borrow the best examples of various organizational and legal technologies from Belarus, Poland, or Ukraine. It is necessary to comprehensively research the factors that affect the state of healthcare, the degree of its financing, the attitude of citizens to primary healthcare, the level of the general culture and legal culture of medical workers and patients, and the involvement of the patient and the doctor in the process of diagnosis and treatment.
Discussion
-
Acknowledgements
- This work was funded by the authors’ own resources.
Acknowledgments
- 1. Khodakova OB, Shilnikova NF. Characterization of legal awareness as a factor affecting the social satisfaction of the population when receiving medical care. Problems of social hygiene. Healthc Hist Med 2012;5:22−5. [in Russian].ArticlePubMed
- 2. Murray C, Frenk J. World Health Report 2000: A step towards evidence-based health policy. Lancet 2001;357(9269). 1698−700. PMID: 10.1016/S0140-6736(00)04826-1. PMID: 11425395.ArticlePubMed
- 3. Lima AOL, Mochón LG, Tamayo CB. Identification of health outcome indicators in Primary Care. A review of systematic reviews. Rev Calid Asist 2017;32(5). 278−88.ArticlePubMedPMC
- 4. Rawaf S. A proactive general practice: Integrating public health into primary care. London J Prim Care (Abingdon) 2018;10(2). 17−8. PMID: 10.1080/17571472.2018.1445946.
- 5. Boyce T, Peckham S, Hann A, et al. A pro-active approach: Health promotion and ill-health prevention. London (UK): Kings Fund; 2010. p 41.
- 6. The World Health Report 2000: Health systems: Improving performance [Internet] Geneva (Switzerland): World Health Organization; 2000 [cited 2019 Aug 13]. Available from: https://www.who.int/whr/2000/en/whr00_en.pdf?ua=1.
- 7. Chebanova M, Chernoknyzhna K, Sinichenko V. Health care system in Belarus: path of least resistance. Mod Econ Stud 2018;1(1). 18−27.
- 8. Meads G. Primary care in the twenty-first century - An international perspective. Oxford (UK): CRC Press; 2006. p 172. ArticlePDF
- 9. Kim CE, Shin JS, Lee J, et al. Quality of medical service, patient satisfaction and loyalty with a focus on interpersonal-based medical service encounters and treatment effectiveness: a cross-sectional multicenter study of complementary and alternative medicine (CAM) hospitals. BMC Complement Altern Med 2017;17(1). e174PMID: 10.1186/s12906-017-1691-6.ArticlePubMedPMC
- 10. Tang L. The influences of patient’s satisfaction with medical service delivery, assessment of medical service, and trust in health delivery system on patient’s life satisfaction in China. Health Qual Life Outcomes 2012;10:111PMID: 10.1186/1477-7525-10-111.
- 11. Ziapour A, Khatony A, Jafari F, et al. Patient satisfaction with medical services provided by a hospital in Kermanshah Iran. Acta Medica Mediterranea 2016;32:959−65.Article
- 12. Groenewegen PP, Dourgnon P, Greß S, et al. Strengthening weak primary care systems: Steps towards stronger primary care in selected Western and Eastern European countries. Health Pol 2013;113(1–2). 170−9. PMID: 10.1016/j.healthpol.2013.05.024.
- 13. Busse R. Health care systems in EU pre-accession countries and European integration. Arbeit und Sozialpolitik 2002;56(5–6). 41−9.
- 14. Karailanov MG, Rusev IT, Borisov DN, et al. Reform of primary health care in Russia. News Russian Mil Med Acad 2017;36(1). 32−6. [in Russian].
- 15. Voronenko YuV, Lysenko GI, Sheker OG. Family medicine at the head of healthcare reform in Ukraine. Bulletin of the KSMA named after I.K. Akhunbaeva 2013;2:20−6. [in Russian].
- 16. WHO Regional Committee for Europe [Internet]. Resolution - Strengthening health systems as a continuation of the WHO Regional Office for Europe’s Country Strategy “Matching services to new needs” [Internet] Copenhagen (Denmark): WHO Regional Office for Europe; 2005 [cited 2019 Aug 12]. Available from: https://www.euro.who.int/__data/assets/pdf_file/0010/88093/RC55_eres08.pdf.
- 17. Demchenko I. Reforma krajowego systemu opieki zdrowotnej Ukrainy. Pierwsze Wyniki I Dalsze Perspektywy Medyczna Wokanda 2018;10(10). 169−84. [in Polish].
- 18. Richardson E, Malakhova I, Novik I, et al. Belarus: health system review. Health Syst Transit 2013;15(5). 1−118. PMID: 24334702.
- 19. Lekhan V, Rudiy V, Shevchenko M, et al. Ukraine: Health system review. Health Syst Transit 2015;17(2). 1−154. PMID: 26106880.
- 20. Sowada C, Sagan A, Kowalska-Bobko I, et al. Poland: Health System Review. Health Syst Transit 2019;21(1). 1−234. PMID: 31333192.
- 21. Stetsenko S. The right to health as a constitutional value Public Law 2018; Special issue:1705[in Ukrainian].
- 22. Shatkovskiy Y. Access to medical care: Administrative and legal framework for security. Visegrad J Hum Rights 2019;6:253−6.Article
- 23. Sidelkovsky O. Subjects of formation and implementation of public policy in the field of health care. Public Law 2020;1:116−23. PMID: 10.37374/2020-37-10.Article
- 24. Ahiyevets S. Legal framework of accessible medical care in the conditions of sustainable development goals achieving. Medical Law 2020;1:9−16.
- 25. Yakovenko IV. Healthcare reform in Ukraine: initial results pending. Kyiv (Ukraina) 2018;25[in Ukrainian].
- 26. Gadsby E, Peckham S, Kvit A, et al. Public health programmes and policies in Ukraine: development, design and implementation. Kent (UK): Centre for Health Services Studies; 2017. p 23. ArticlePubMed
- 27. Rechel B, McKee M. Health reform in Central and Eastern Europe and the former Soviet Union. Lancet 2009;374:1186−95. PMID: 10.1016/S0140-6736(09)61334-9. PMID: 19801097.
- 28. Boerma WGW, Pellny M, Wiegers TA, et al. Evaluation of the Organizational Model of Primary Care in Belarus A Survey-Based Project in the Regions of Minsk and Vitebsk. Copenhagen (Denmark): World Health Organization; 2009.
- 30. OECD and World Health Organization [Internet]. State of Health in the EU. Poland. Country Health Profile 2017 [cited 2019 Aug 13]. Available from: https://ec.europa.eu/health/sites/health/files/state/docs/chp_poland_english.pdf.
- 31. The Ljubljana Charter on Reforming Health Care, 1996 [Internet] [cited 2019 Aug 13]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0010/113302/E55363.pdf?ua=1.
- 32. Joffe S, Manocchia M, Weeks J, et al. What do patients value hospital care? An empirical perspective on autonomy center bioethics. J Med Ethics 2003;29(2). 103−8. PMID: 10.1136/jme.29.2.103. PMID: 12672891. PMID: 1733711.ArticlePubMedPMC
- 33. Rusinova NL, Panova LV, Burmykina ON. Predictors of customer satisfaction with primary healthcare services. Sociol Med 2006;2(9). 24−31.
- 34. Golovchenko V. Medical ethics as a potential source of law. Legal Bull Ukraine 2014;15(980). 12.
References
Figure 1
Preference of the methods and the ability to make an appointment with the doctor.
* Registering by phone, † personal request to the registry, ‡ via the internet.
BY = Belarus; PL = Poland; UA = Ukraine.
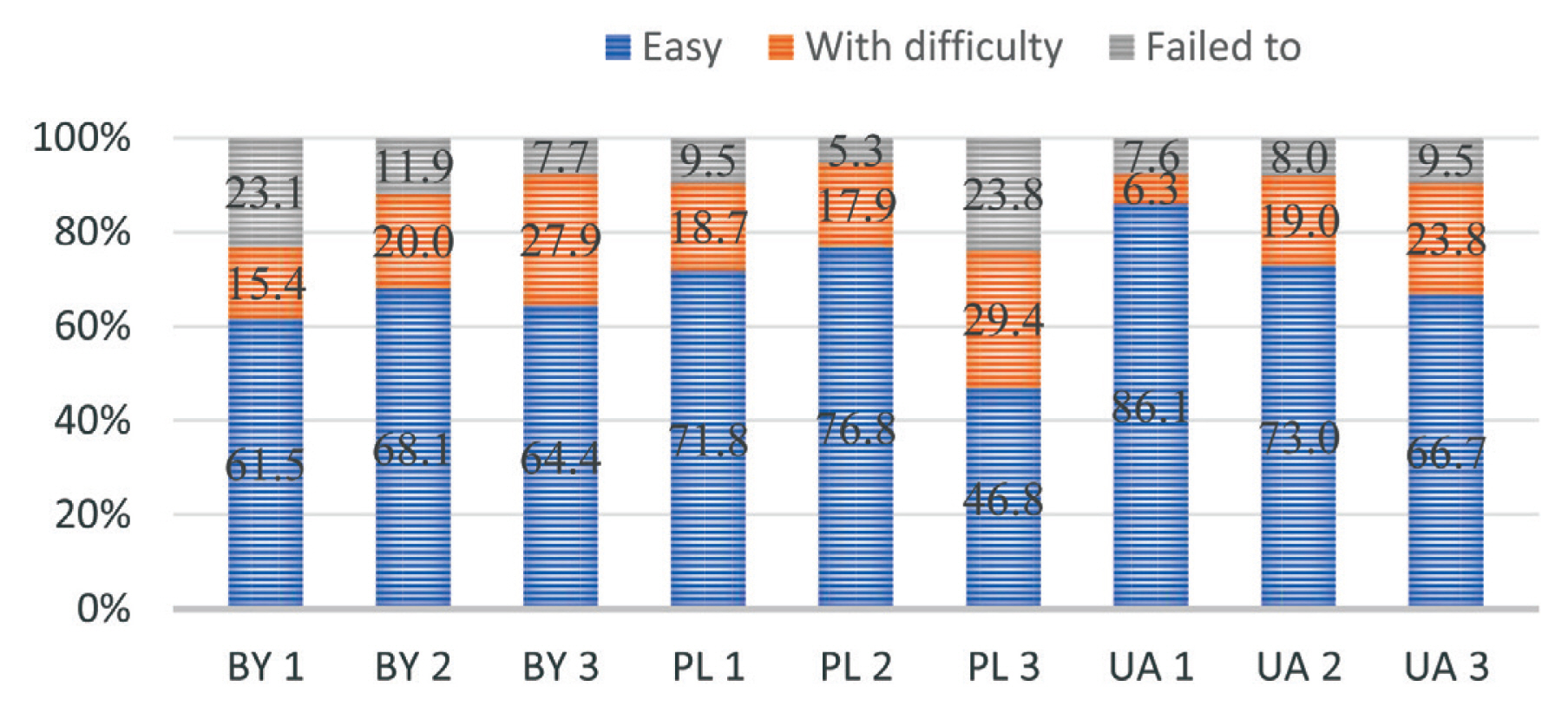
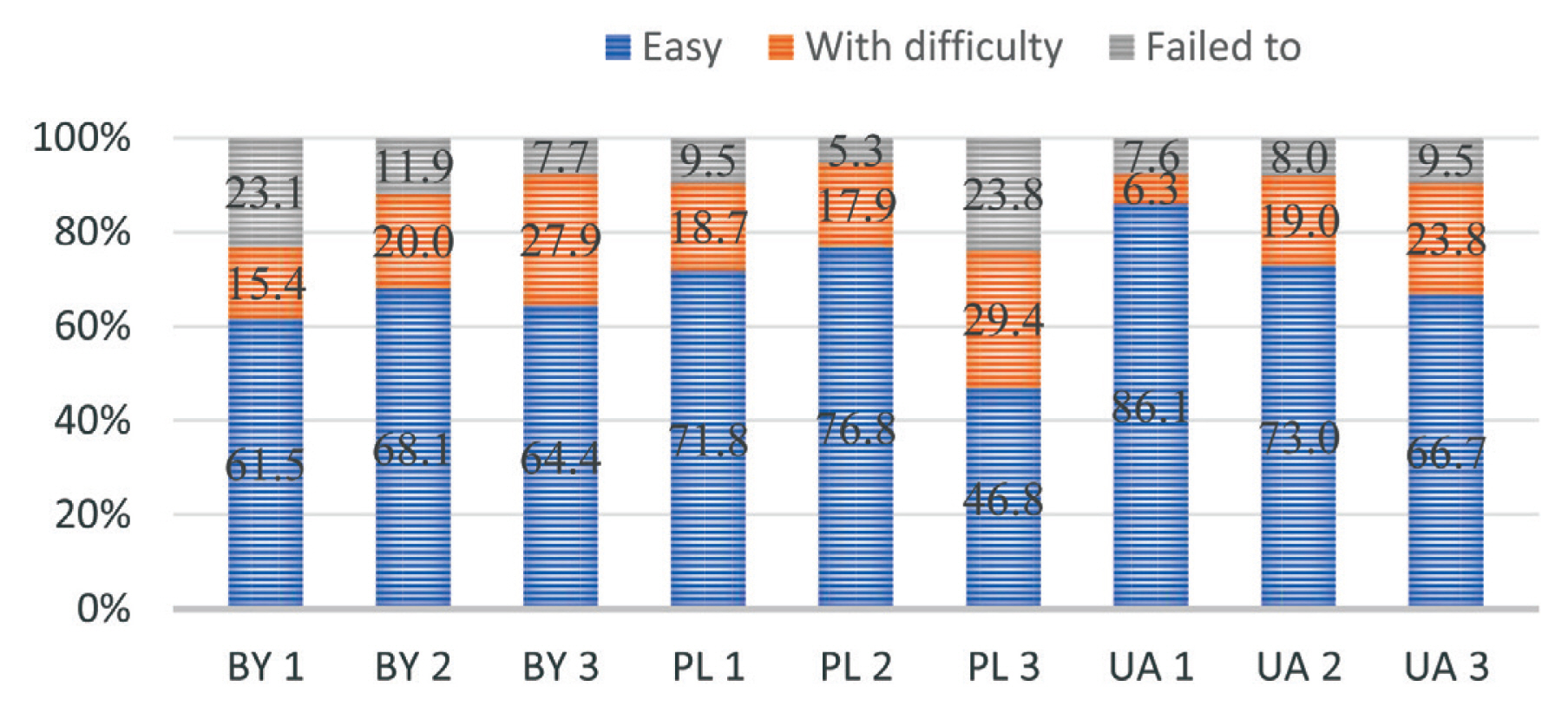
Figure 2
The communication experience of respondents with a doctor.
BY = Belarus; PL = Poland; UA = Ukraine.
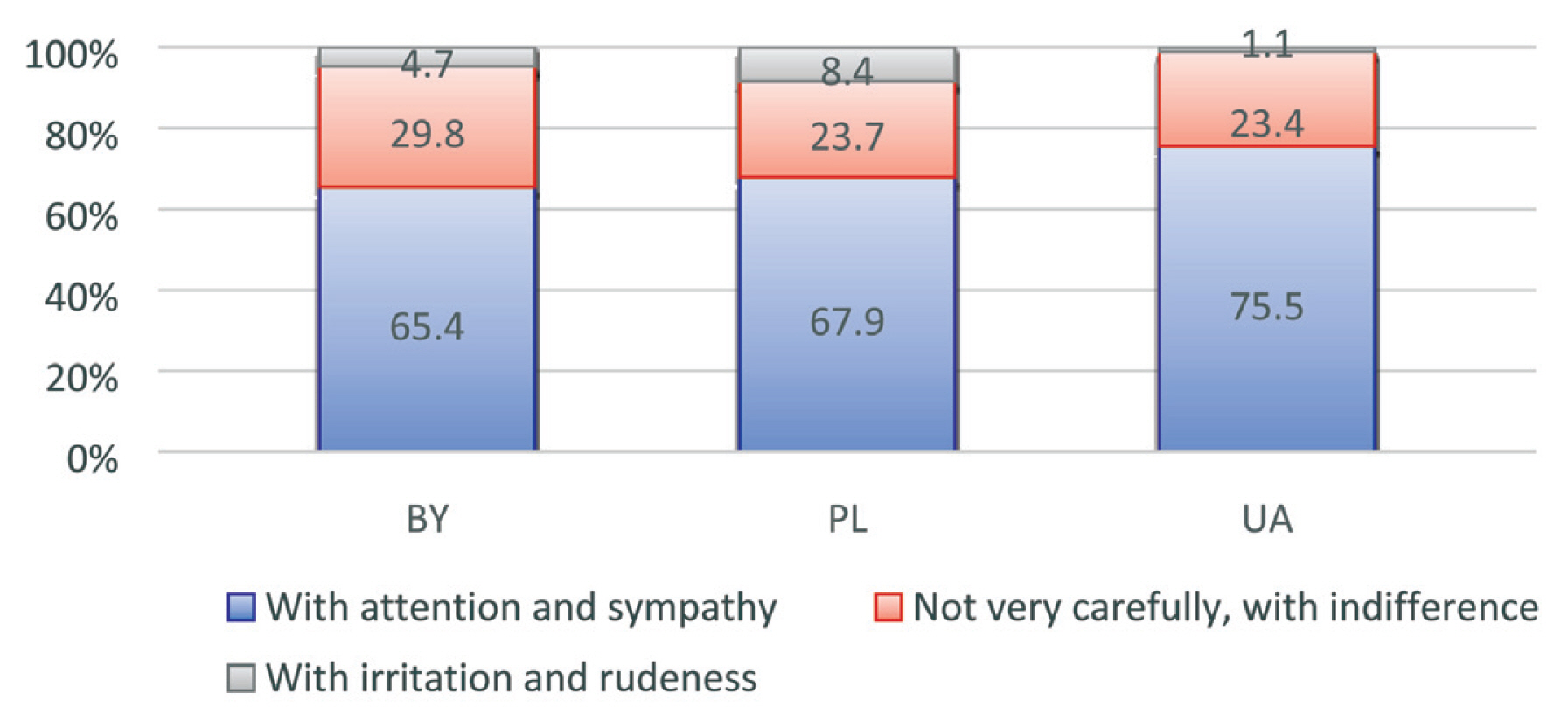
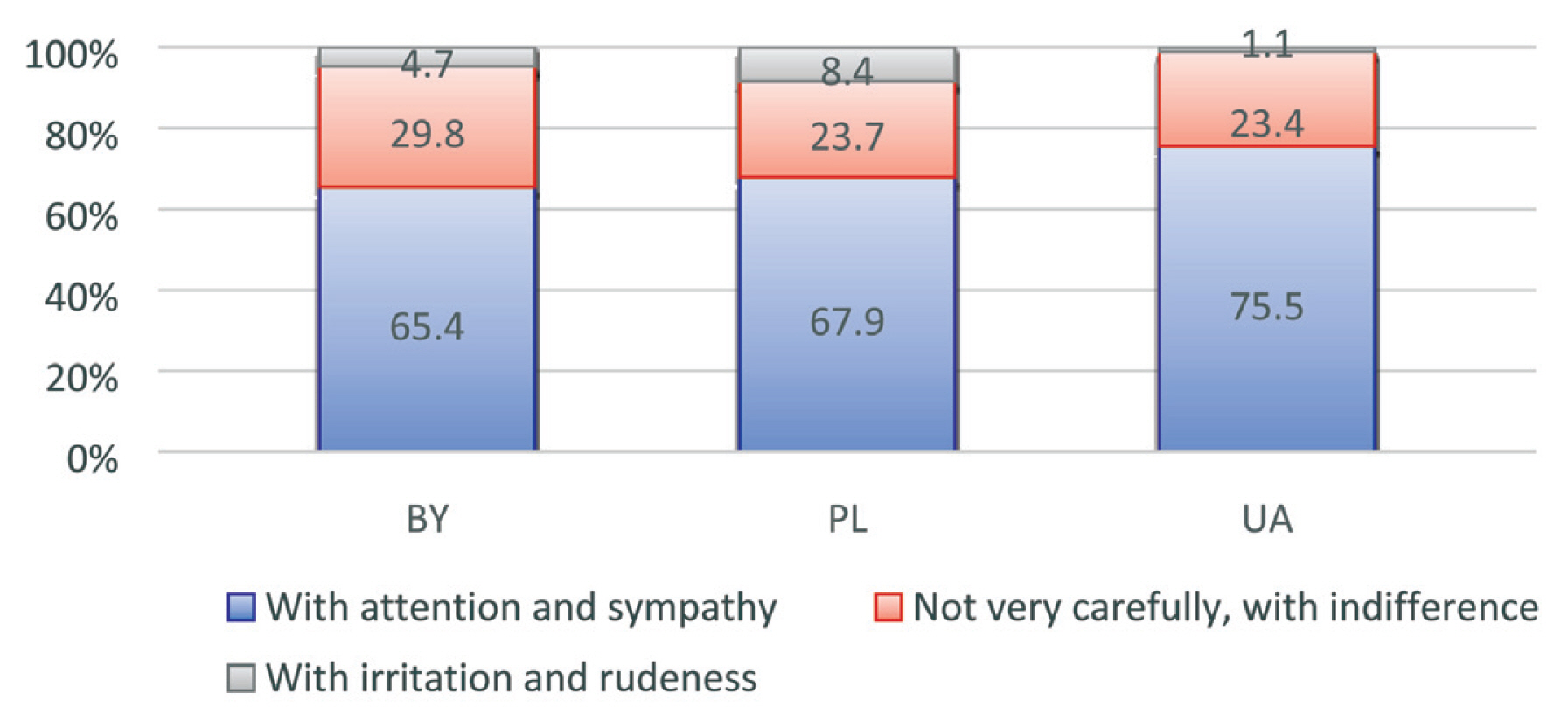
Figure 3
Types of official and illegal payment for diagnostic and treatment services when visiting a doctor among respondents who indicated cases of payment.
BY = Belarus; PL = Poland; UA = Ukraine.
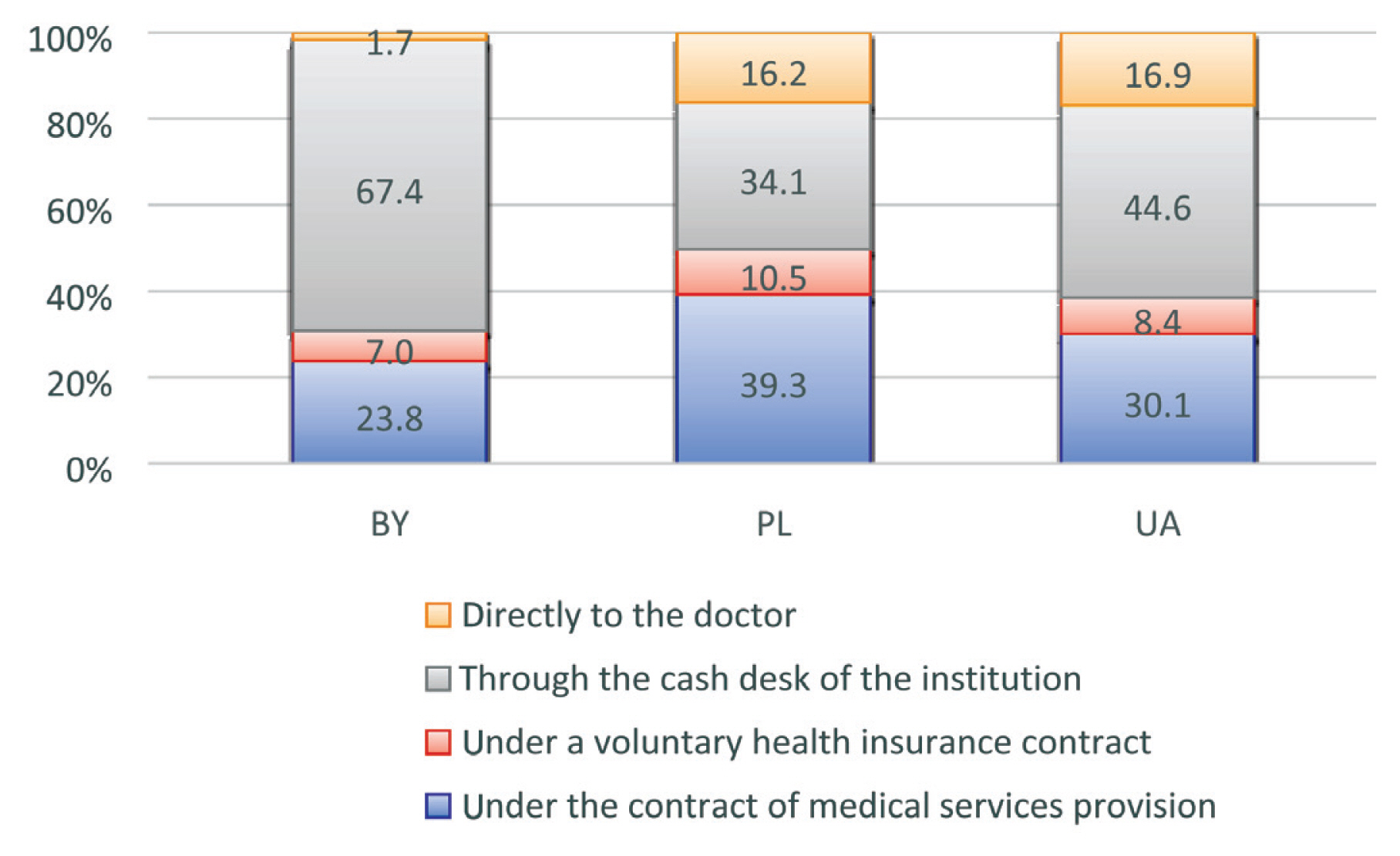
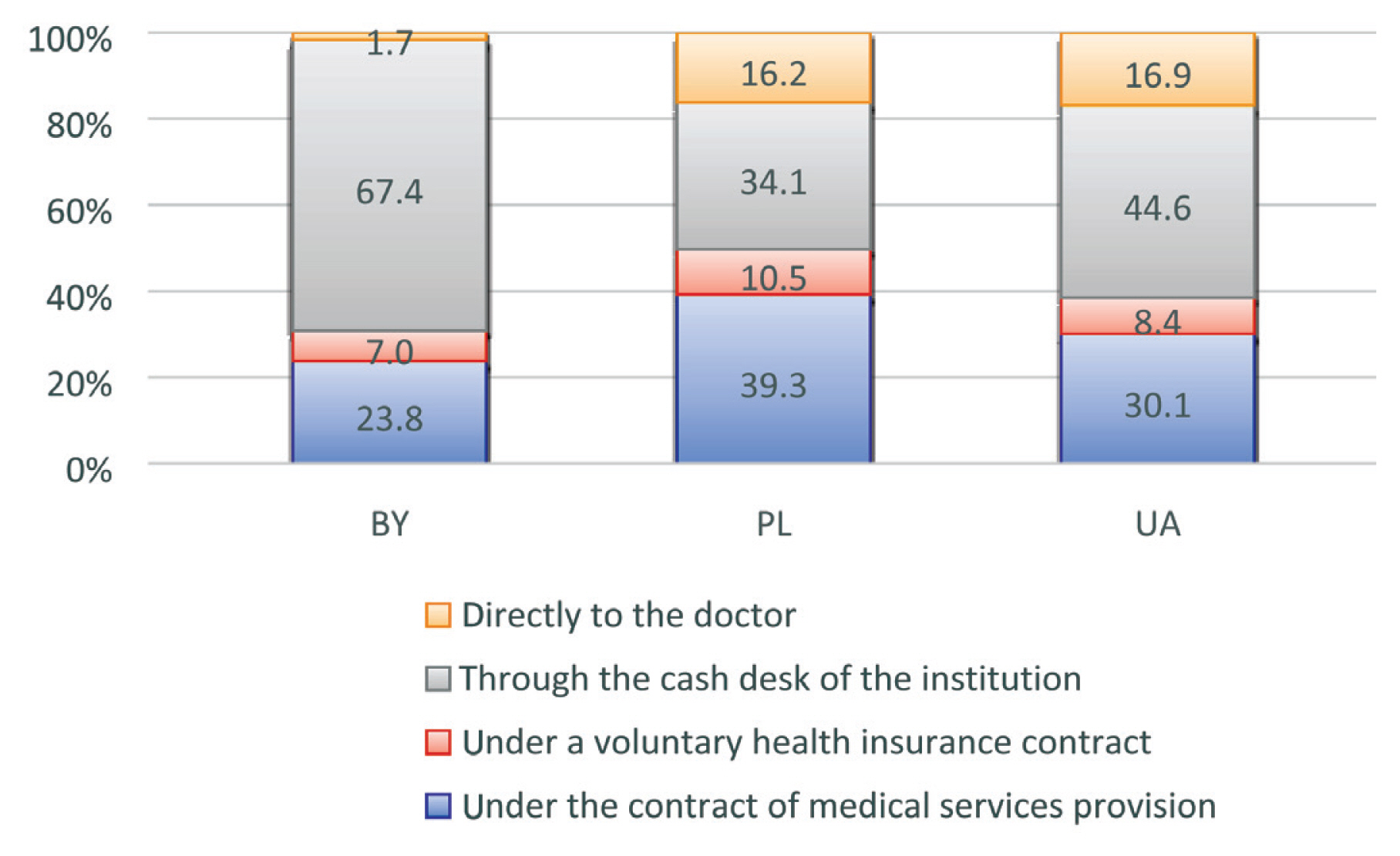
Table 1General descriptive characteristics of groups of respondents (interviewed students) depending on the country.
| Belarus (n = 191) | Poland (n = 346) | Ukraine (n = 94) | Total (n = 631) | p | |
|---|---|---|---|---|---|
| Age (y ± SD) | 21.6 ± 2.50 | 21.7 ± 2.82 | 21.7 ± 2.61 | 21.6 ± 2.41 | > 0.05* |
| Men (%, 95% CI) | 34.0 (27.3–40.8) | 30.1 (25.2–34.9) | 17.0 (9.4–24.6) | 29.3 (25.8–32.9) | < 0.05† |
| Women (%, 95% CI) | 66.0 (59.3–72.7) | 69.9 (65.1–74.8) | 83.0 (75.4–90.6) | 70.7 (67.1–74.2) | < 0.05† |
Table 2Dates of the last call to the family doctor/general practitioner (%, 95% CI).
| Belarus | Poland | Ukraine | Total | p* | |
|---|---|---|---|---|---|
|
|
|||||
| When was the last time you went to a family doctor (general practitioner)? | |||||
| < a month | 22.0 (16.1–27.9) | 12.4 (9.0–15.9) | 14.9 (7.7–22.1) | 15.7 (12.9–18.5) | < 0.05 |
| > a month | 78.0 (72.1–83.9) | 85.6 (84.1–91.1) | 85.1 (77.9–92.3) | 84.3 (81.5–87.2) | |
|
|
|||||
| Made an appointment at the first request | 74.4 (68.2–80.5) | 86.1 (82.5–89.8) | 86.2 (79.2–93.2) | 82.6 (79.6–85.5) | < 0.01 |
|
|
|||||
| By phone | 88.5 (84.0–93.0) | 91.3 (88.4–94.3) | 84.0 (76.6–91.4) | 89.4 (87.0–91.8) | < 0.01 |
|
|
|||||
| Via personal request to the registry | 83.8 (75.8–89.0) | 80.9 (76.8–85.1) | 67.0 (57.5–67.5) | 79.7 (76.6–82.9) | > 0.01 |
|
|
|||||
| Via the internet | 54.5 (47.4–61.5) | 36.4 (31.4–41.5) | 22.3 (13.9–30.8) | 39.8 (36.0–43.6) | < 0.01 |
Table 3Duration of waiting for primary healthcare depending on the country of observation.
| Indicator | Belarus | Poland | Ukraine | Total | p |
|---|---|---|---|---|---|
| Travel time from home to the doctor (geographical availability) X ± SD, Me | 18.7 ± 9.9, 15.0 | 20.6 ± 11.8, 15.0 | 25.5 ± 11.6, 30.0 | 20.7 ± 11.4, 15.0 | < 0.05* |
| How many days have passed from appeal date to a family doctor (general practitioner) to receive medical care until the appointment? (%, 95% CI) | |||||
| 1–2 d | 34.0 (27.3–40.8) | 58.4 (53.2–63.6) | 54.3 (44.2–64.3) | 50.4 (46.5–54.3) | < 0.001† |
| 3–4 d | 22.5 (16.6–28.4) | 20.2 (16.0–24.5) | 16.0 (8.6–23.4) | 20.3 (17.2–23.4) | |
| > 4 d | 43.5 (36.4–50.5) | 21.4 (17.1–25.7) | 29.8 (20.5–39.0) | 29.3 (25.8–32.9) | |
| How long did you expect to wait to see a doctor? (%, 95% CI) | |||||
| Virtually no expectation | 14.7 (9.6–19.7) | 17.6 (13.6–21.7) | 14.9 (7.7–22.1) | 16.3 (13.4–19.2) | < 0.001† |
| 10 min | 36.6 (29.8–43.5) | 15.9 (12.1–19.8) | 27.7 (18.6–36.7) | 23.9 (20.6–27.3) | |
| 20 min | 11.0 (6.6–15.4) | 31.5 (26.6–36.4) | 28.7 (19.6–37.9) | 24.9 (21.5–28.3) | |
| > 20 min | 37.7 (30.8–44.6) | 35.0 (30.0–40.0) | 28.7 (19.6–37.9) | 34.9 (31.2–38.6) | |
Table 4Satisfaction with the quality of the doctor’s appointment (in points).
| Belarus | Poland | Ukraine | Total | p* | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| X ± SD | Me (Q25–Q75) | X ± SD | Me (Q25–Q75) | X ± SD | Me (Q25–Q75) | X ± SD | Me (Q25–Q75) | ||
| Courtesy and attentiveness of the doctor | 4.0 ± 1.0 | 4.0 (3–5) | 3.9 ± 1.13 | 4.0 (3–5) | 3.9 ± 1.10 | 4.0 (3–5) | 3.9 ± 1.10 | 4.0 (3–5) | > 0.05 |
|
|
|||||||||
| Doctor’s explanation of the purpose of medical examination and their results, treatment features | 3.6 ± 0.81 | 3.0 (3–4) | 3.7 ± 1.18 | 4.0 (3–5) | 3.6 ± 1.31 | 4.0 (3–5) | 3.6 ± 1.10 | 4.0 (3–5) | < 0.05 |
|
|
|||||||||
| Identification by a doctor of a change in health status taking into account the patient’s complaints | 3.5 ± 0.92 | 3.0 (3–4) | 3.7 ± 1.20 | 4.0 (3–5) | 3.6 ± 1.81 | 4.0 (3–5) | 3.6 ± 1.24 | 4.0 (3–5) | < 0.05 |
|
|
|||||||||
| Assessment of treatment results | 3.3 ± 0.9 | 3.0 (3–4) | 3.5 ± 0.88 | 4.0 (3–4) | 3.5 ± 1.08 | 4.0 (3–4) | 3.5 ± 0.93 | 3.0 (3–4) | < 0.05 |
|
|
|||||||||
| Difficulty getting a prescription for drugs | 17 (8.9) | 45 (13.0) | 3 (3.2) | 65 (10.3) | < 0.05 | ||||
|
|
|||||||||
| Satisfaction with overall medical care provided by a doctor | 3.9 ± 0.9 | 4.0 (3–5) | 4.1 ± 0.85 | 4.0 (4–5) | 3.9 ± 0.79 | 4.0 (3–5) | 4.0 ± 0.83 | 4.0 (3–5) | > 0.05 |
Table 5Distribution of answers about who often violates the rights of the patient (%, 95% CI).
Figure & Data
References
Citations
Citations to this article as recorded by 

- The perception of outpatient care quality by healthcare users in Ukraine
Valentyna Anufriyeva, Milena Pavlova, Tetiana Stepurko, Wim Groot
International Journal of Healthcare Management.2024; 17(1): 25. CrossRef - Satisfaction with primary health care in Ukraine in 2016–2020: A difference-in-differences analysis on repeated cross-sectional data
Valentyna Anufriyeva, Milena Pavlova, Tetiana Chernysh (Stepurko), Wim Groot
Health Policy.2023; 137: 104916. CrossRef


 PubReader
PubReader ePub Link
ePub Link Cite
Cite