Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 11(2); 2020 > Article
-
Short Communication
Coronavirus Disease-19: The First 7,755 Cases in the Republic of Korea -
Osong Public Health and Research Perspectives 2020;11(2):85-90.
DOI: https://doi.org/10.24171/j.phrp.2020.11.2.05
Published online: April 30, 2020
Korea Centers for Disease Control and Prevention, Cheongju, Korea
- *Corresponding author: COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention, Cheongju, Korea, E-mail: jeongek@korea.kr
Copyright ©2020, Korea Centers for Disease Control and Prevention
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
- We report the first 7,755 patients with confirmed COVID-19 in Korea as of March 12th, 2020. A total of 66 deaths have been recorded, giving a case fatality proportion of 0.9%. Older people, and those with comorbidities were at a higher risk of a fatal outcome. The highest number of cases of COVID-19 were in Daegu, followed by Gyeongbuk. This summary may help to understand the disease dynamics in the early phase of the COVID-19 outbreaks, and may therefore, guide future public health measures.
- Only a few weeks after the first case of coronavirus disease 2019 (COVID-19) was reported in Wuhan, China, the first case of COVID-19 was confirmed in the Republic of Korea on January 20th, 2020 [1]. International travel has facilitated the spread of COVID-19 throughout the world. As of March 13th, 2020, 118 countries, territories, and areas have reported COVID-19 cases, however, differences in patterns and intensity of transmission ranges were observed [2]. In February and early March in Korea, a sharp increase in the number of COVID-19 cases were observed, with most infections in specific clusters and geographical regions.
- Based on the surveillance data, we report the basic epidemiological characteristics of COVID-19 to examine the early course of the pandemic. Furthermore, factors associated with COVID-19 cases and fatality were investigated to provide information on a vulnerable part of the population to guide public health prioritization.
Introduction
- This is a summary of the first 7,755 patients with confirmed COVID-19 in Korea as of March 12th, 2020. To obtain demographic, epidemiological, and early clinical information, COVID-19 reporting and surveillance data were retrieved from Korea Centers for Disease Control and Prevention (KCDC)-operated National Notifiable Disease Surveillance System (NNDSS) [3]. The patient age was provided on the date of diagnosis, and key indicators such as estimated duration of exposure, date of onset of symptoms, and route of transmission were identified by field epidemiological investigators [1]. It must be noted that the data presented in this summary may change depending on the results of further epidemiological investigations.
Materials and Methods
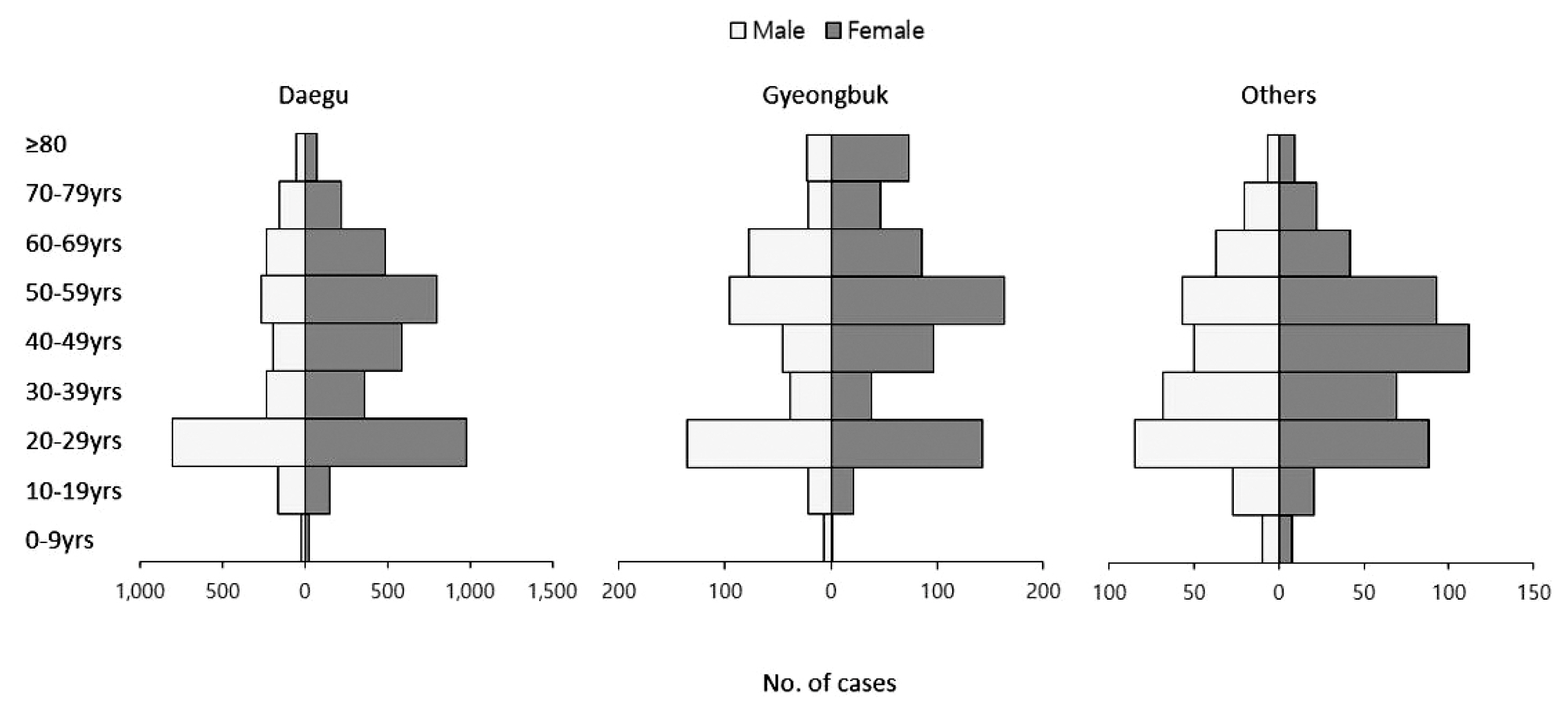
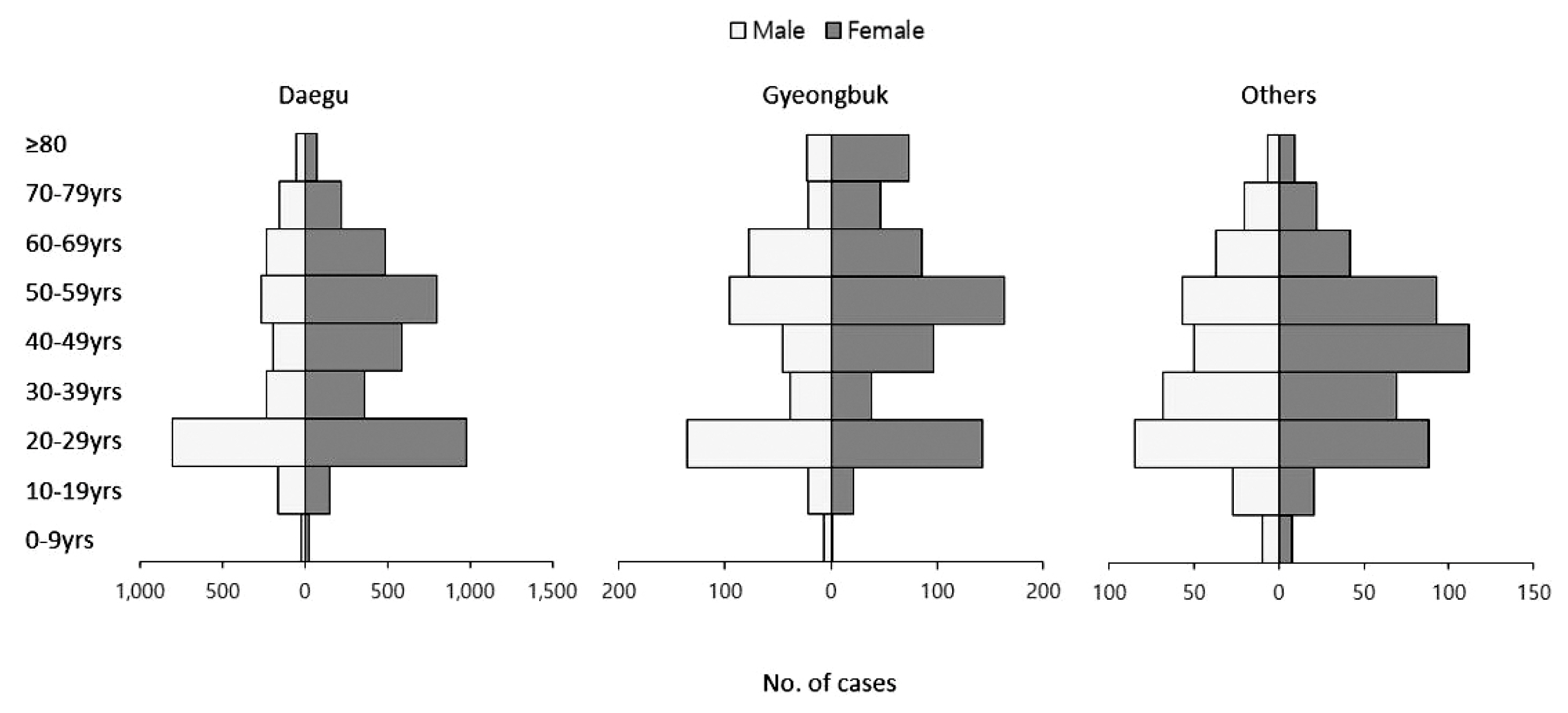
- As of March 12th, 2020, a total of 7,755 laboratory-confirmed cases of COVID-19 and 66 deaths were recorded in Korea, giving a case fatality proportion of 0.9% (Table 1). The female-to-male ratio of confirmed COVID-19 cases was 62:38. The age group 20–29 years accounted for the highest level of all confirmed cases at 28.9%, followed by 50–59 years, and 40–49 years. The case fatality proportion was 0.1% among 30–39 years and 40–49 years age groups, then increased to 0.4% in the 50–59 years, 1.5% in the 60–69 years, 5.0% in the 70–79 years, and 8.5% in the ≥80 years age groups (Table 1).
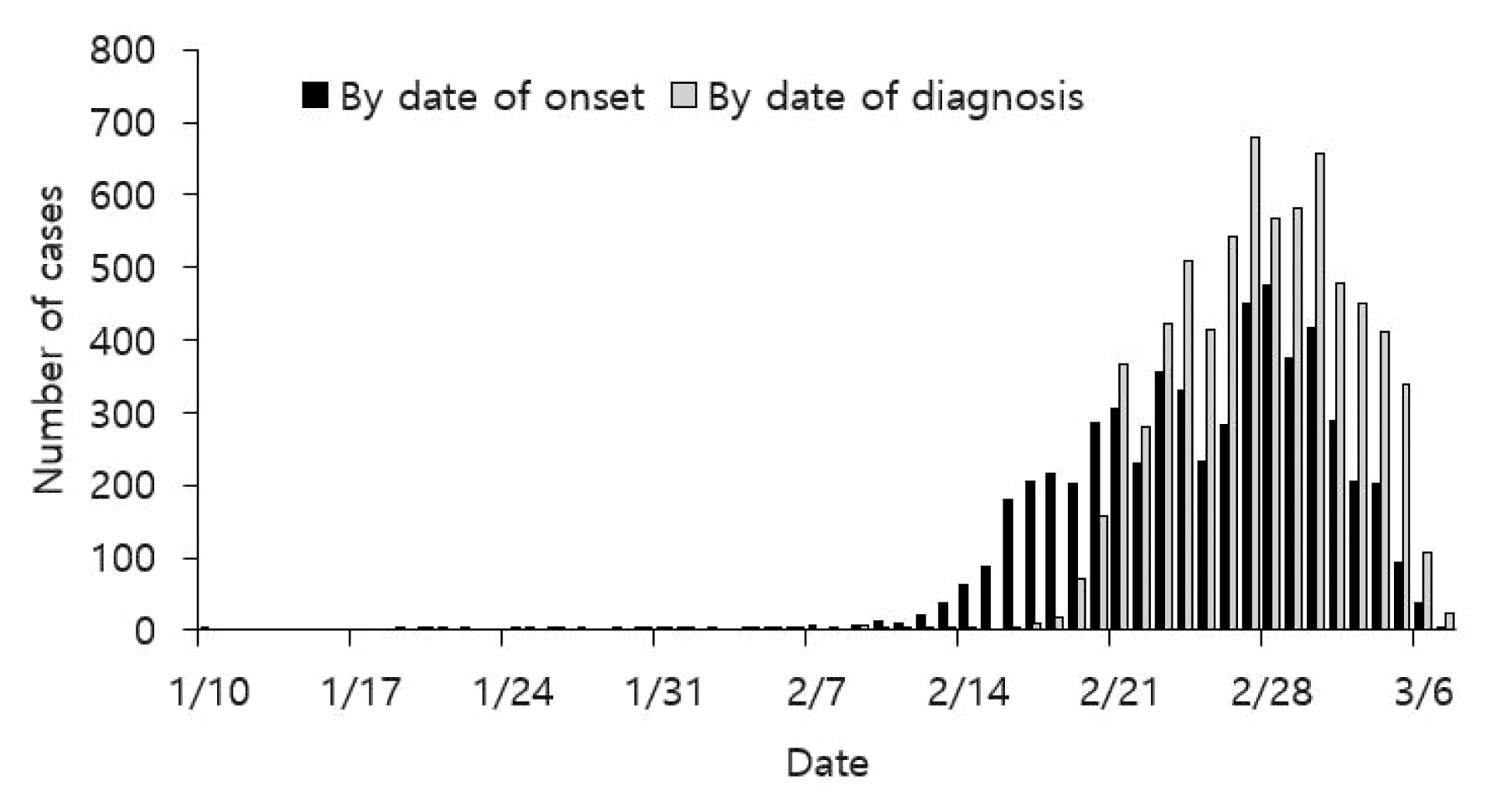
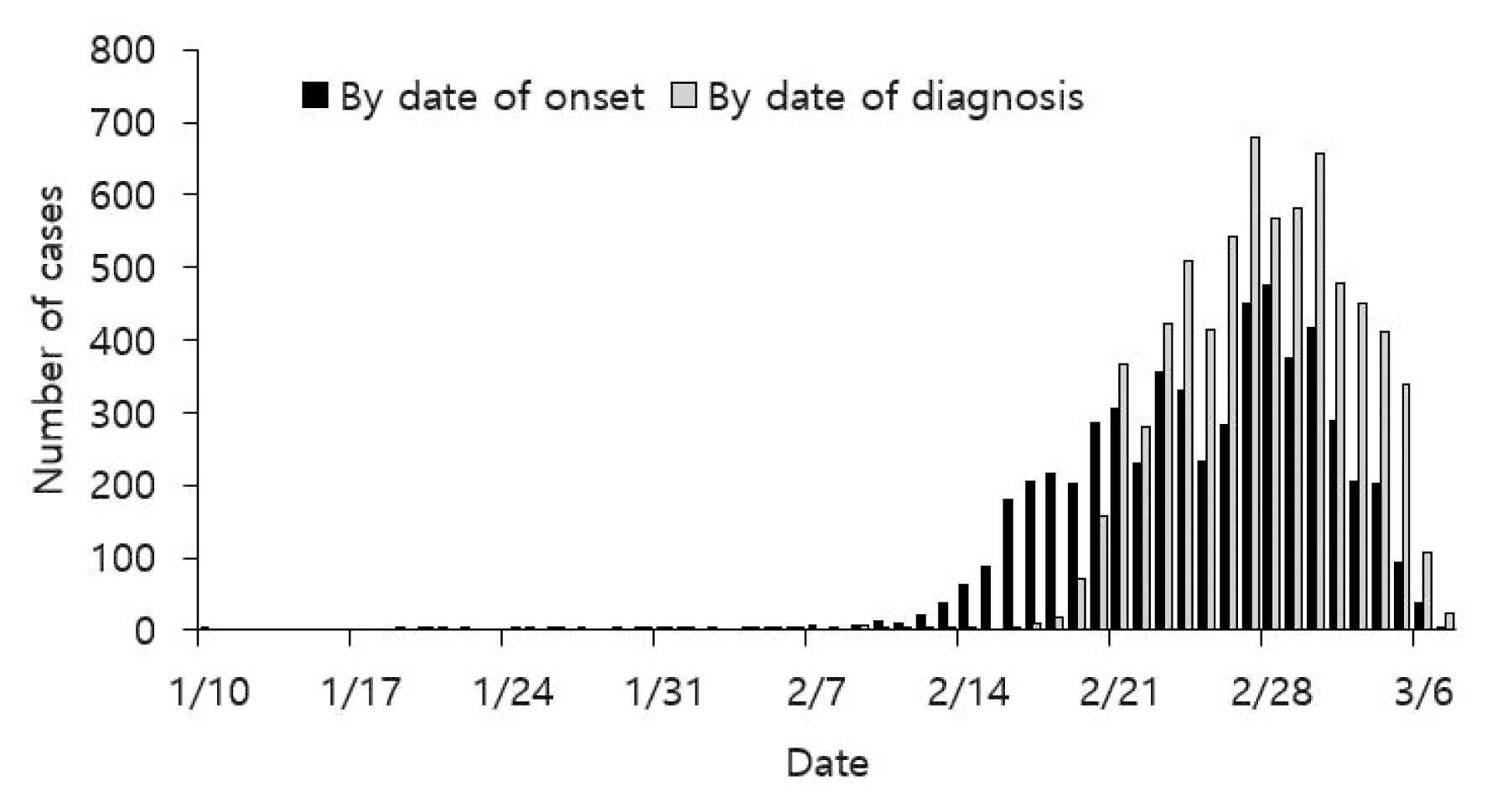
- The epidemic curves presented in Figures 1 and 2 were generated using National Notifiable Disease Surveillance System (NNDSS) data. Epidemic curves by date of onset preceded epidemic curves by date of diagnosis, by a few days or a week (Figure 1). It must be noted that the date of symptom onset may change depending on further epidemiological investigation, and delayed reporting of cases. Figure 2 depicts an epidemic curve by different regions of Korea: the nationwide, Daegu, Gyeongbuk, and others (outside Daegu and Gyeongbuk). From mid-February, an increased number of cases were reported with a peak in late February and early March. Figure 3 shows the age distribution and sex ratio among Daegu, Gyeongbuk, and others regions. Note the increased proportion of cases in 20–29 years and in females among cases in Daegu and Gyeongbuk.
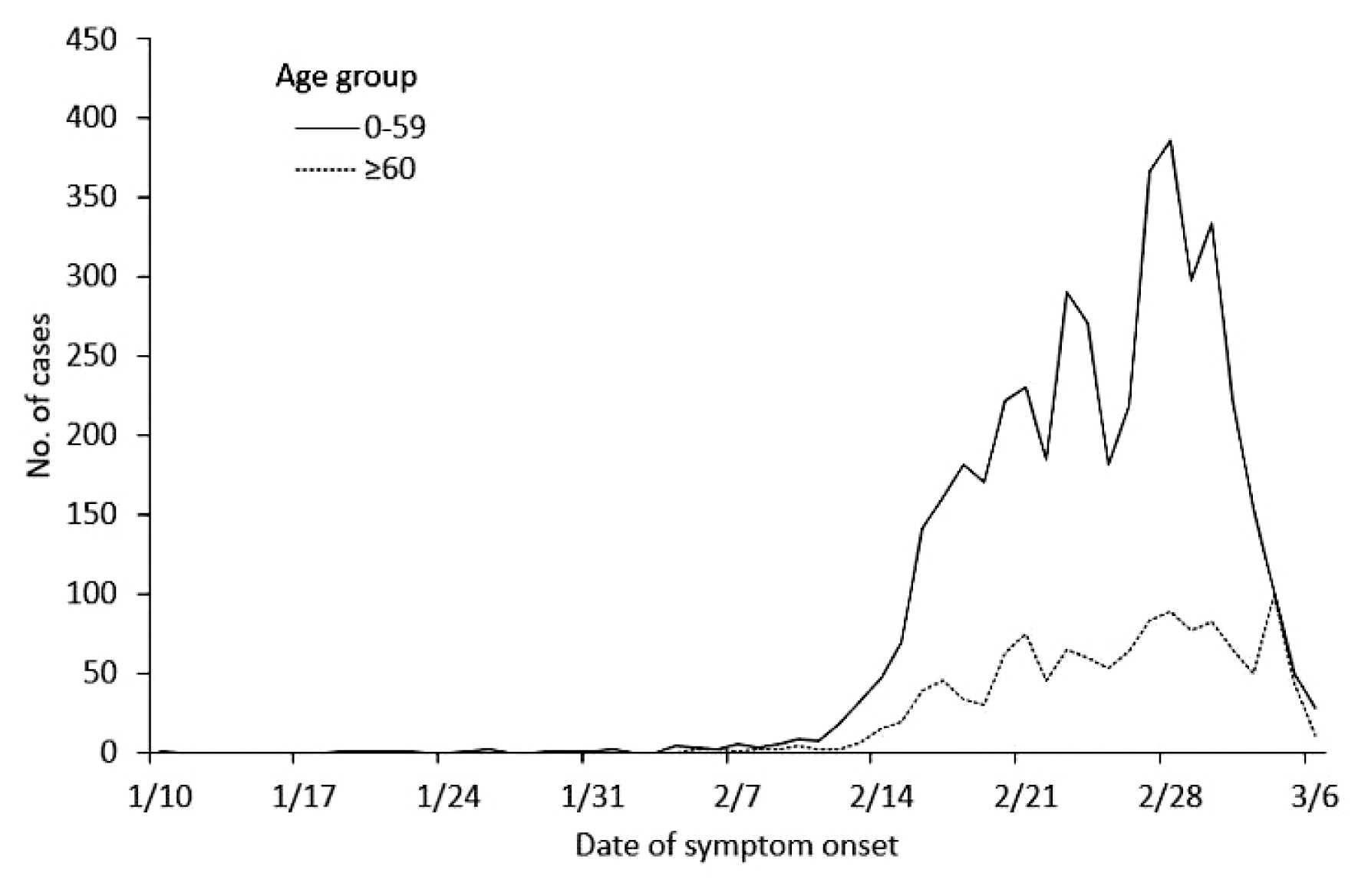
- Fatal cases of COVID-19 in Korea, as of March 12th, 2020 are shown in Tables 2 and 3. Case fatality proportion was the highest among people aged ≥ 80 years in Daegu, followed by those aged 70–79 years in Daegu, and elderly persons ≥ 80 years old in Gyeongbuk. Overall case fatality proportion in Daegu and Gyeongbuk were 0.8% and 1.4%, which were higher than that in other regions with 0.4%. Figure 4 depicts age-specific epidemic curve stratified as 0–59 years and ≥ 60 years. The outbreak generally began with the younger age group, followed by the elderly population.
- There were 66 laboratory-confirmed fatal cases of COVID-19, as of March 12th, 2020 (Table 3). The median age was 77 years (range, 35–93 years), and female-to-male ratio of 44:56. Of 63 cases, 96.8% were reported to have comorbidities: 47.6% hypertension, 36.5% diabetes, 16% neurodegenerative disorders, and 17.5% pulmonary diseases. There were 71.2% of fatal cases in Daegu and 24.2% were from Gyeongbuk. There were 5 patients who succumbed to death at home, and COVID-19 was identified as the cause of death in 11 individuals after their death. The median interval between onset of symptoms and death was 10 days (range 1–24 days), while the median interval between date of hospitalization and date of death was 5 days (range 0–16 days).
Results
- The analysis of the first 7,755 cases of COVID-19 in Korea showed an initial increase in cases in specific geographical regions, comparable to the epidemiological situation in China and Italy [4,5]. In Korea, despite a sharp decline in the number of confirmed cases reported, there were still a relevant number of confirmed cases per week in late February and early March. With descriptive analysis of interim surveillance data, the data suggest that the patient outcome differed markedly between the geographic regions, highlighting the magnitude of surge of cases and access to hospitalization. The difference in age distribution of COVID-19 cases compared with China may reflect active surveillance of a cluster of religious groups tied to the outbreak.
- A summary of the epidemiological characteristics of the first 7,755 COVID-19 cases in Korea confirms the contagiousness of COVID-19 that led to a nationwide outbreak in a few weeks. Triaging patients for hospitalization, social distancing (to reduce the number of contacts), and reporting the outbreak amongst vulnerable people in the population may have played a role in the recent decline in cases of COVID-19. However, in the initial response to COVID-19, quarantine, early detection, and isolation of suspected cases of COVID-19, may have contributed to lowering the wave of this epidemic in other parts of Korea. More severe cases were reported in the elderly with existing comorbidities, which warrants clear triage management and a high-risk approach in healthcare access prioritization. COVID-19 does not appear to be fatal among young adults and children, however their role in disease transmission should be further assessed.
- This summary may help in the understanding of early phase disease dynamics for the COVID-19 outbreak, and guide future public health measures in other countries.
Discussion
-
Acknowledgements
- We thank the relevant ministries, including the Ministry of Interior and Safety, Si/Do and Si/Gun/Gu, medical staffs in health centers, and medical facilities for their efforts in responding to the COVID-19 outbreak.
Acknowledgments
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
COVID-19 National Emergency Response Center, Epidemiology and Case Management Team
Korea Centers for Disease Control and Prevention (KCDC):
Eun Kyeong Jeong
Center for Disease Prevention, KCDC: Ok Park, Young Joon Park, Shin Young Park, Young-Man Kim, Jieun Kim, Joongho Jo, Jungwoo Kim, Taeyoung Kim, Sanghui Kweon, Yeonhee Woo, Minwoo Yum, Eunyoung Kim
Center for Public Health Emergency Preparedness and Response, KCDC: Jin Gwack, Jin Lee, Eunmi Park, Seong Sun Kim, Junghee Hyun, Boyeong Ryu, Yoon Suk Jang, Hwami Kim, Yeowon Jin, Hyeyoung Lee, Sangeun Lee, Seung Hwan Shin, Seung Woo Choi, Daehyeon Ko, Seonju Yi, Hee Kyoung Kim
Center for Infectious Disease Control, KCDC: Dongwook Kim, Byoung-Hak Jeon, Miyoung Kim, Si won Choi
Center for Genome Science, KCDC: Jung Hyun Lee, Jae Kyung Park
Bureau of Health Policy, Ministry of Health and Welfare:
Unna Kim
Department of Social and Preventive Medicine, Hallym University College of Medicine: Young June Choe
Article information
- 1. COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Early Epidemiological and Clinical Characteristics of 28 Cases of Coronavirus Disease in South Korea. Osong Public Health Res Perspect 2020;11(1). 8−14. PMID: 10.24171/j.phrp.2020.11.1.03. PMID: 32149037. PMID: 7045878.ArticlePubMedPMC
- 2. World Health Organization [Internet]. Coronavirus disease 2019 (COVID-19) Situation Report – 52 [cited 2020 Mar 13]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 3. Park S, Cho E. National Infectious Diseases Surveillance data of South Korea. Epidemiol Health 2014;36:e2014030PMID: 10.4178/epih/e2014030. PMID: 25420951. PMID: 4272235.ArticlePubMedPMCPDF
- 4. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223). 497−506. PMID: 10.1016/S0140-6736(20)30183-5. PMID: 31986264.ArticlePubMedPMC
- 5. Spiteri G, Fielding J, Diercke M, et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill 2020;25(9). 2000178PMID: 10.2807/1560-7917.ES.2020.25.9.2000178. PMID: 7068164.ArticlePubMedPMC
References

| Variables | n | (%) |
|---|---|---|
| Age (y), median (range) | 77 | (35–93) |
|
|
||
| Sex | ||
| Female | 29 | (43.9) |
| Male | 37 | (56.1) |
|
|
||
| Coexisting condition* | ||
| Any | 61 | (96.8) |
| Cerebrovascular disease | 5 | (7.9) |
| Heart disease | 10 | (15.9) |
| Pulmonary disease | 11 | (17.5) |
| Kidney disease | 5 | (7.9) |
| Diabetes | 23 | (36.5) |
| Hypertension | 30 | (47.6) |
| Cancer | 7 | (11.1) |
| Neurodegenerative disorder | 16 | (25.4) |
| Under investigation | 5 | (6.5) |
|
|
||
| Region | ||
| Daegu | 47 | (71.2) |
| Gyeongbuk | 16 | (24.2) |
| Others | 3 | (4.5) |
|
|
||
| Death while in home | 5 | (7.6) |
| Diagnosis after death | 11 | (16.7) |
| Interval, days, median (range) | ||
| Symptom → Death | 10 | (1–24) |
| Symptom → Diagnosis | 4 | (0–20) |
| Symptom → Hospitalization | 4.5 | (0–11) |
| Hospitalization → Death | 5 | (0–16) |
| Total | 66 | |
Figure & Data
References
Citations

- Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Increased risk of SARS-CoV-2 infection and COVID-19 death among older patients at long-term care hospitals in Korea
Jeong-Yeon Seon, Sunjea Kim, Min Kyoung Lim, In-Hwan Oh
Frontiers in Public Health.2023;[Epub] CrossRef - Effects of COVID-19 Pandemic on Young Individuals - A Mini Review
Rohan Rishabh Susarla, Rania Zein Eldin, Ritika Coelho
New Emirates Medical Journal.2023;[Epub] CrossRef - Mortality among COVID-19 Patients with Different Comorbidities in Kermanshah, West of Iran (2020)
Leila Rezakhani, Mozafar Khazaei, Siavash Vaziri, Fatemeh Khosravi Shadmani
Journal of Occupational Health and Epidemiology.2023; 12(1): 4. CrossRef - Prevalence of cancer as a comorbid in COVID-19 patients and their characteristics: a meta-analysis study
Johan S. Sitanggang, Kamal B. Siregar, Henry H. Sitanggang, Noverita Sprinse Vinolina
F1000Research.2022; 10: 975. CrossRef - Correction of menopausal disorders: new possibilities of menopausal hormone therapy
L. Yu. Karakhalis
Meditsinskiy sovet = Medical Council.2022; (5): 112. CrossRef - On the Parametrization of Epidemiologic Models—Lessons from Modelling COVID-19 Epidemic
Yuri Kheifetz, Holger Kirsten, Markus Scholz
Viruses.2022; 14(7): 1468. CrossRef - Clinical Outcomes and Severity of Acute Respiratory Distress Syndrome in 1154 COVID-19 Patients: An Experience Multicenter Retrospective Cohort Study
Abbas Al Mutair, Saad Alhumaid, Laila Layqah, Jinan Shamou, Gasmelseed Y. Ahmed, Hiba Chagla, Khulud Alsalman, Fadhah Mohammed Alnasser, Koritala Thoyaja, Waad N. Alhuqbani, Mohammed Alghadeer, Mohammed Al Mohaini, Sana Almahmoud, Jaffar A. Al-Tawfiq, Jav
COVID.2022; 2(8): 1102. CrossRef - Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea
Seong Hoon Kim, Euna Min, Young Mi Hwang, Yun Suk Choi, Jin Wook Yi
Cancers.2022; 14(17): 4338. CrossRef - Epidemiological and Clinical Profile of COVID-19 cases attending Rural Health Training Centre of one of the Medical Colleges of Ahmedabad, Gujarat, India
Sheetal Vyas, Bansi Davda, Krushna Modi, Minal Patel
Healthline.2022; 13(3): 244. CrossRef - Epidemiological Description of COVID-19 Cases at selected Counties in Kenya that border Uganda and Tanzania, March-July 2020
Gladys Mutethya Francis, Josephine Waihuini Ihahi, Adow Aden Buul, Florence Wanjiru Mugo, Robert Mburu Kuria, Kenneth Kipkoech Korir, Sora Jatani Biid, Julius Shem Otwabe, Ahmed Abade Mohamed, Waqo Boru, Elvis Omondi Oyugi, Maurice Omondi Owiny, Josephine
Journal of Interventional Epidemiology and Public .2022;[Epub] CrossRef - COVID-19 Vaccination in Korea: Past, Present, and the Way Forward
Eliel Nham, Joon Young Song, Ji Yun Noh, Hee Jin Cheong, Woo Joo Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature
Kalpana Thapa Bajgain, Sujan Badal, Bishnu B. Bajgain, Maria J. Santana
American Journal of Infection Control.2021; 49(2): 238. CrossRef - First results of the “Lean European Open Survey on SARS-CoV-2-Infected Patients (LEOSS)”
Carolin E. M. Jakob, Stefan Borgmann, Fazilet Duygu, Uta Behrends, Martin Hower, Uta Merle, Anette Friedrichs, Lukas Tometten, Frank Hanses, Norma Jung, Siegbert Rieg, Kai Wille, Beate Grüner, Hartwig Klinker, Nicole Gersbacher-Runge, Kerstin Hellwig, Luk
Infection.2021; 49(1): 63. CrossRef - Angiotensin‐converting enzyme as a new immunologic target for the new SARS‐CoV‐2
Shahin Hallaj, Anahita Ghorbani, Seyed Ali Mousavi‐Aghdas, Mohammad Mirza‐Aghazadeh‐Attari, Andrey Sevbitov, Vida Hashemi, Tooba Hallaj, Farhad Jadidi‐Niaragh
Immunology & Cell Biology.2021; 99(2): 192. CrossRef - Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis
Amirhossein Hessami, Amir Shamshirian, Keyvan Heydari, Fatemeh Pourali, Reza Alizadeh-Navaei, Mahmood Moosazadeh, Saeed Abrotan, Layla Shojaie, Sogol Sedighi, Danial Shamshirian, Nima Rezaei
The American Journal of Emergency Medicine.2021; 46: 382. CrossRef - Older Adults With Coronavirus Disease 2019: A Nationwide Study in Turkey
Mert Esme, Meltem Koca, Ayse Dikmeer, Cafer Balci, Naim Ata, Burcu Balam Dogu, Mustafa Cankurtaran, Meltem Yilmaz, Osman Celik, Gulnihal Gokce Unal, Mustafa Mahir Ulgu, Suayip Birinci, Anne B Newman
The Journals of Gerontology: Series A.2021; 76(3): e68. CrossRef - Taiwan's COVID-19 response: Timely case detection and quarantine, January to June 2020
Hao-Yuan Cheng, Yu-Neng Chueh, Chiu-Mei Chen, Shu-Wan Jian, Shu-Kuan Lai, Ding-Ping Liu
Journal of the Formosan Medical Association.2021; 120(6): 1400. CrossRef - Metabolic Syndrome and COVID-19 Mortality Among Adult Black Patients in New Orleans
John Xie, Yuanhao Zu, Ala Alkhatib, Thaidan T. Pham, Frances Gill, Albert Jang, Stella Radosta, Gerard Chaaya, Leann Myers, Jerry S. Zifodya, Christine M. Bojanowski, Nassir F. Marrouche, Franck Mauvais-Jarvis, Joshua L. Denson
Diabetes Care.2021; 44(1): 188. CrossRef - Epidemiologic Linkage of COVID-19 Outbreaks at Two University-affiliated Hospitals in the Seoul Metropolitan Area in March 2020
Kuenyoul Park, Jaewoong Lee, Kihyun Lee, Jiwon Jung, Sung-Han Kim, Jina Lee, Mauricio Chalita, Seok-Hwan Yoon, Jongsik Chun, Kyu-Hwa Hur, Heungsup Sung, Mi-Na Kim, Hae Kyung Lee
Journal of Korean Medical Science.2021;[Epub] CrossRef - Exploration of sex-specific and age-dependent COVID-19 fatality rate in Bangladesh population
Md Abdul Alim Al-Bari, Showna Hossain, Md Kudrat-E Zahan
World Journal of Radiology.2021; 13(1): 1. CrossRef - Coronavirus disease 2019 and neurodegenerative disease: what will the future bring?
Lindsay S. McAlpine, Arman Fesharaki-Zadeh, Serena Spudich
Current Opinion in Psychiatry.2021; 34(2): 177. CrossRef - Network study of responses to unusualness and psychological stress during the COVID-19 outbreak in Korea
Seunghyong Ryu, In-Hoo Park, Mina Kim, Yu-Ri Lee, Jonghun Lee, Honey Kim, Min Jhon, Ju-Wan Kim, Ju-Yeon Lee, Jae-Min Kim, Sung-Wan Kim, Akihiro Nishi
PLOS ONE.2021; 16(2): e0246894. CrossRef - Factors Influencing the Preventive Practice of International Students in South Korea against COVID-19 during the Pandemic
Gun Ja Jang, Ginam Jang, Sangjin Ko
International Journal of Environmental Research an.2021; 18(5): 2259. CrossRef - Epidemiology, clinical spectrum, viral kinetics and impact of COVID‐19 in the Asia‐Pacific region
Kin On Kwok, Ying Huang, Margaret Ting Fong Tsoi, Arthur Tang, Samuel Yeung Shan Wong, Wan In Wei, David Shu Cheong Hui
Respirology.2021; 26(4): 322. CrossRef - Clinical Reviews of COVID-19 for Otorhinolaryngologists
Ki-Il Lee, Dong Kyu Kim, Ji-Hun Mo
Journal of Rhinology.2021; 28(1): 1. CrossRef - Validation of the Korean Version of the COVID-19 Phobia Scale (K-C19PS)
Mihyeon Seong, Misoon Lee, Insook Kim, Miran Kang
International Journal of Environmental Research an.2021; 18(7): 3747. CrossRef - Risk Assessment of Importation and Local Transmission of COVID-19 in South Korea: Statistical Modeling Approach
Hyojung Lee, Yeahwon Kim, Eunsu Kim, Sunmi Lee
JMIR Public Health and Surveillance.2021; 7(6): e26784. CrossRef - Impact of obesity on the health of men and women during the COVID-19 pandemic
L.V. Adamyan, E.N. Andreeva, E.V. Sheremetyeva, G.A. Manushakyan
Problemy reproduktsii.2021; 27(3): 28. CrossRef - SARS-CoV-2 Seroprevalence and Neutralizing Antibody Response after the First and Second COVID-19 Pandemic Wave in Croatia
Tatjana Vilibic-Cavlek, Vladimir Stevanovic, Maja Ilic, Ljubo Barbic, Krunoslav Capak, Irena Tabain, Jasna Lenicek Krleza, Thomas Ferenc, Zeljka Hruskar, Renata Zrinski Topic, Vanja Kaliterna, Arlen Antolovic-Pozgain, Jasmina Kucinar, Iva Koscak, Dijana M
Pathogens.2021; 10(6): 774. CrossRef - Clinical Features and Outcomes of Coronavirus Disease 2019 Among People With Human Immunodeficiency Virus in the United States: A Multicenter Study From a Large Global Health Research Network (TriNetX)
George A Yendewa, Jaime Abraham Perez, Kayla Schlick, Heather Tribout, Grace A McComsey
Open Forum Infectious Diseases.2021;[Epub] CrossRef - The first 1000 symptomatic pediatric SARS-CoV-2 infections in an integrated health care system: a prospective cohort study
Leigh M. Howard, Kathryn Garguilo, Jessica Gillon, Kerry LeBlanc, Adam C. Seegmiller, Jonathan E. Schmitz, Daniel W. Byrne, Henry J. Domenico, Ryan P. Moore, Steven A. Webber, Natasha B. Halasa, Ritu Banerjee
BMC Pediatrics.2021;[Epub] CrossRef - Prevalence and characteristics of cancer patients with COVID-19: a meta-analysis study
Johan S. Sitanggang, Kamal B. Siregar, Henry H. Sitanggang, Noverita Sprinse Vinolina
F1000Research.2021; 10: 975. CrossRef - Factors shaping the COVID-19 epidemic curve: a multi-country analysis
Su Yeon Jang, Laith Hussain-Alkhateeb, Tatiana Rivera Ramirez, Ahmed Asa’ad Al-Aghbari, Dhia Joseph Chackalackal, Rocio Cardenas-Sanchez, Maria Angelica Carrillo, In-Hwan Oh, Eduardo Andrés Alfonso-Sierra, Pia Oechsner, Brian Kibiwott Kirui, Martin Anto,
BMC Infectious Diseases.2021;[Epub] CrossRef - Experience from five Asia-Pacific countries during the first wave of the COVID-19 pandemic: Mitigation strategies and epidemiology outcomes
Clotilde El Guerche-Séblain, Lina Chakir, Gopinath Nageshwaran, Rebecca C. Harris, Caroline Sevoz-Couche, Olivier Vitoux, Philippe Vanhems
Travel Medicine and Infectious Disease.2021; 44: 102171. CrossRef - Policy Review and Modeling Analysis of Mitigation Measures for Coronavirus Disease Epidemic Control, Health System, and Disease Burden, South Korea
Hae-Young Kim, In-Hwan Oh, Jacob Lee, Jeong-Yeon Seon, Woo-Hwi Jeon, Jae Seok Park, Sung-Il Nam, Niket Thakkar, Prashanth Selvaraj, Jessica McGillen, Daniel Klein, Scott Braithwaite, Anna Bershteyn, Seung Heon Lee
Emerging Infectious Diseases.2021;[Epub] CrossRef - A Review on the Role of Stem Cells against SARS-CoV-2 in Children and Pregnant Women
Fatemeh Sanie-Jahromi, Yaser NejatyJahromy, Rahim Raoofi Jahromi
International Journal of Molecular Sciences.2021; 22(21): 11787. CrossRef - COVID-19 Vaccination in Pregnancy, Paediatrics, Immunocompromised Patients, and Persons with History of Allergy or Prior SARS-CoV-2 Infection: Overview of Current Recommendations and Pre- and Post-Marketing Evidence for Vaccine Efficacy and Safety
Nicoletta Luxi, Alexia Giovanazzi, Annalisa Capuano, Salvatore Crisafulli, Paola Maria Cutroneo, Maria Pia Fantini, Carmen Ferrajolo, Ugo Moretti, Elisabetta Poluzzi, Emanuel Raschi, Claudia Ravaldi, Chiara Reno, Marco Tuccori, Alfredo Vannacci, Giovanna
Drug Safety.2021; 44(12): 1247. CrossRef - Therapeutic opportunities for improving the course of coronavirus disease and reducing the frequency of gestional complications
V.V. Kaminskyi, R.O. Tkachenko, A.V. Kaminskyi, O.I. Zhdanovych, L.I. Vorobei, T.V. Kolomiichenko, O.I. Gervaziuk, R.R. Tkachuk, S.I. Mudryi
REPRODUCTIVE ENDOCRINOLOGY.2021; (62): 8. CrossRef - The Outbreak of COVID-19 and Diabetes in Korea: “We Will Find a Way as We Have Always Done”
Kyu Chang Won, Kun Ho Yoon
Diabetes & Metabolism Journal.2020; 44(2): 211. CrossRef - Transmission dynamics, serial interval and epidemiology of COVID-19 diseases in Hong Kong under different control measures
Yung-Wai Desmond Chan, Stefan Flasche, Tin-Long Terence Lam, Mei-Hung Joanna Leung, Miu-Ling Wong, Ho-Yeung Lam, Shuk-Kwan Chuang
Wellcome Open Research.2020; 5: 91. CrossRef - Clinical Course of Asymptomatic and Mild COVID-19: Early Clinical Features of Patients Admitted to a Living and Treatment Support Center in Jecheon, South Korea (Part II)
Soomin Nam, Yeon Ho Lee, Se Hwan An, Eun Hee Kim, So Hee Hong, Jeon Wook Kwon, Seung Wook Lee, Hyoung Seop Kim
SSRN Electronic Journal .2020;[Epub] CrossRef - Clinical Course of COVID-19 in Asymptomatic and Mildly Symptomatic Patients: Archives of a Living and Treatment Support Center in South Korea (Part I)
Soomin Nam, Yeon Ho Lee, Kye Seon Jang, Mun Young Chang, Do Hyeon Yun, Hye Seon Park, Jin Kyu Lee, Hyoung Seop Kim
SSRN Electronic Journal .2020;[Epub] CrossRef - Surveillance of the first cases of COVID-19 in Sergipe using a prospective spatiotemporal analysis: the spatial dispersion and its public health implications
Lucas Almeida Andrade, Dharliton Soares Gomes, Marco Aurélio de Oliveira Góes, Mércia Simone Feitosa de Souza, Daniela Cabral Pizzi Teixeira, Caíque Jordan Nunes Ribeiro, José Antônio Barreto Alves, Karina Conceição Gomes Machado de Araújo, Allan Dantas d
Revista da Sociedade Brasileira de Medicina Tropic.2020;[Epub] CrossRef - Evaluation of COVID-19 epidemic outbreak caused by temporal contact-increase in South Korea
Sungchan Kim, Yong Dam Jeong, Jong Hyuk Byun, Giphil Cho, Anna Park, Jae Hun Jung, Yunil Roh, Sooyoun Choi, Ibrahim Malik Muhammad, Il Hyo Jung
International Journal of Infectious Diseases.2020; 96: 454. CrossRef - Children in the Eye of the Pandemic Storm—Lessons From New York City
Jason G. Newland, Kristina A. Bryant
JAMA Pediatrics.2020; 174(10): e202438. CrossRef - COVID-19 and the re-opening of schools: a policy maker’s dilemma
Maria Pia Fantini, Chiara Reno, Giovanni Battista Biserni, Elena Savoia, Marcello Lanari
Italian Journal of Pediatrics.2020;[Epub] CrossRef - Easing lockdown for school children: why so contentious?
Amelia Swift
Evidence Based Nursing.2020; 23(3): 65. CrossRef - Children are unlikely to be the main drivers of the COVID‐19 pandemic – A systematic review
Jonas F. Ludvigsson
Acta Paediatrica.2020; 109(8): 1525. CrossRef - Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies
Alessandro Mantovani, Christopher D. Byrne, Ming-Hua Zheng, Giovanni Targher
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(8): 1236. CrossRef - Prevalence of comorbidities in patients and mortality cases affected by SARS-CoV2: a systematic review and meta-analysis
Omar Ariel Espinosa, Andernice dos Santos Zanetti, Ednardo Fornanciari Antunes, Fabiana Gulin Longhi, Tatiane Amorim de Matos, Paula Franciene Battaglini
Revista do Instituto de Medicina Tropical de São P.2020;[Epub] CrossRef - SARS‐CoV‐2 testing and outcomes in the first 30 days after the first case of COVID‐19 at an Australian children's hospital
Laila F Ibrahim, Shidan Tosif, Sarah McNab, Samantha Hall, Hyun Jung Lee, Stuart Lewena, Andrew J Daley, Nigel W Crawford, Andrew C Steer, Penelope A Bryant, Franz E Babl
Emergency Medicine Australasia.2020; 32(5): 801. CrossRef - The Epidemiology of Severe Acute Respiratory Syndrome Coronavirus 2 in a Pediatric Healthcare Network in the United States
William R Otto, Sarah Geoghegan, Leila C Posch, Louis M Bell, Susan E Coffin, Julia S Sammons, Rebecca M Harris, Audrey R Odom John, Xianqun Luan, Jeffrey S Gerber
Journal of the Pediatric Infectious Diseases Socie.2020; 9(5): 523. CrossRef - The role of children in transmission of SARS-CoV-2: A rapid review
Xue Li, Wei Xu, Marshall Dozier, Yazhou He, Amir Kirolos, Evropi Theodoratou
Journal of Global Health.2020;[Epub] CrossRef - Improving Preparedness for and Response to Coronavirus Disease 19 (COVID-19) in Long-Term Care Hospitals in Korea
Tark Kim
Infection & Chemotherapy.2020; 52(2): 133. CrossRef - Encountering COVID-19 as Endocrinologists
Eun-Jung Rhee, Jung Hee Kim, Sun Joon Moon, Won-Young Lee
Endocrinology and Metabolism.2020; 35(2): 197. CrossRef - Coronavirus Disease 2019 and Diabetes: The Epidemic and the Korean Diabetes Association Perspective
Junghyun Noh, Hyun-Ha Chang, In-Kyung Jeong, Kun Ho Yoon
Diabetes & Metabolism Journal.2020; 44(3): 372. CrossRef - Covid-19: a comprehensive review of a formidable foe and the road ahead
Arafat Hussain, Suniti Yadav, Vijay Hadda, Tejas M Suri, Pawan Tiwari, Saurabh Mittal, Karan Madan, Anant Mohan
Expert Review of Respiratory Medicine.2020; 14(9): 869. CrossRef - COVID‐19 breakthroughs: separating fact from fiction
Paraminder Dhillon, Manuel Breuer, Natasha Hirst
The FEBS Journal.2020; 287(17): 3612. CrossRef - The Mental Health and Sleep Quality of the Medical Staff at a Hub-Hospital against COVID-19 in South Korea
Doo Hyuk Kwon, Jihye Hwang, Yong Won Cho, Mei Ling Song, Keun Tae Kim
Journal of Sleep Medicine.2020; 17(1): 93. CrossRef - Diabetes and COVID-19: Global and regional perspectives
In-Kyung Jeong, Kun Ho Yoon, Moon Kyu Lee
Diabetes Research and Clinical Practice.2020; 166: 108303. CrossRef - Epidemiology of COVID-19 and Predictors of Recovery in the Republic of Korea
Ashis Kumar Das, Saji Saraswathy Gopalan
Pulmonary Medicine.2020; 2020: 1. CrossRef - Clinical characteristics, laboratory outcome characteristics, comorbidities, and complications of related COVID-19 deceased: a systematic review and meta-analysis
Peishan Qiu, Yunjiao Zhou, Fan Wang, Haizhou Wang, Meng Zhang, Xingfei Pan, Qiu Zhao, Jing Liu
Aging Clinical and Experimental Research.2020; 32(9): 1869. CrossRef - The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea
Mi Kyung Kim, Jae-Han Jeon, Sung-Woo Kim, Jun Sung Moon, Nan Hee Cho, Eugene Han, Ji Hong You, Ji Yeon Lee, Miri Hyun, Jae Seok Park, Yong Shik Kwon, Yeon-Kyung Choi, Ki Tae Kwon, Shin Yup Lee, Eon Ju Jeon, Jin-Woo Kim, Hyo-Lim Hong, Hyun Hee Kwon, Chi Yo
Diabetes & Metabolism Journal.2020; 44(4): 602. CrossRef - Rapid Deployment of a Free, Privacy-Assured COVID-19 Symptom Tracker for Public Safety During Reopening: System Development and Feasibility Study
Seble G Kassaye, Amanda Blair Spence, Edwin Lau, David M Bridgeland, John Cederholm, Spiros Dimolitsas, JC Smart
JMIR Public Health and Surveillance.2020; 6(3): e19399. CrossRef - Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: A systematic review and meta-analysis
Yue Zhou, Qing Yang, Jingwei Chi, Bingzi Dong, Wenshan Lv, Liyan Shen, Yangang Wang
International Journal of Infectious Diseases.2020; 99: 47. CrossRef - Quantification of Death Risk in Relation to Sex, Pre-Existing Cardiovascular Diseases and Risk Factors in COVID-19 Patients: Let’s Take Stock and See Where We Are
Amalia Ioanna Moula, Linda Renata Micali, Francesco Matteucci, Fabiana Lucà, Carmelo Massimiliano Rao, Orlando Parise, Gianmarco Parise, Michele Massimo Gulizia, Sandro Gelsomino
Journal of Clinical Medicine.2020; 9(9): 2685. CrossRef - Estradiol, Progesterone, Immunomodulation, and COVID-19 Outcomes
Franck Mauvais-Jarvis, Sabra L Klein, Ellis R Levin
Endocrinology.2020;[Epub] CrossRef - Aging, Male Sex, Obesity, and Metabolic Inflammation Create the Perfect Storm for COVID-19
Franck Mauvais-Jarvis
Diabetes.2020; 69(9): 1857. CrossRef - Evolutionary and structural analyses of SARS-CoV-2 D614G spike protein mutation now documented worldwide
Sandra Isabel, Lucía Graña-Miraglia, Jahir M. Gutierrez, Cedoljub Bundalovic-Torma, Helen E. Groves, Marc R. Isabel, AliReza Eshaghi, Samir N. Patel, Jonathan B. Gubbay, Tomi Poutanen, David S. Guttman, Susan M. Poutanen
Scientific Reports.2020;[Epub] CrossRef - Endocrine Significance of SARS-CoV-2’s Reliance on ACE2
Eric Lazartigues, Mirza Muhammad Fahd Qadir, Franck Mauvais-Jarvis
Endocrinology.2020;[Epub] CrossRef - Epidemiologic, clinical, and laboratory findings of the COVID-19 in the current pandemic: systematic review and meta-analysis
Yewei Xie, Zaisheng Wang, Huipeng Liao, Gifty Marley, Dan Wu, Weiming Tang
BMC Infectious Diseases.2020;[Epub] CrossRef - First-time Diabetic Ketoacidosis in Type 2 Diabetics With Covid-19 Infection: A Novel Case Series
Alexander Croft, Antonino Bucca, Jaclyn H. Jansen, Christine Motzkus, Audrey Herbert, Alfred Wang, Benton R. Hunter
The Journal of Emergency Medicine.2020; 59(5): e193. CrossRef - Can data from paediatric cohorts solve the COVID-19 puzzle?
Lien Anh Ha Do, Jeremy Anderson, Edward Kim Mulholland, Paul V. Licciardi, Carolyn B. Coyne
PLOS Pathogens.2020; 16(9): e1008798. CrossRef - On the Progression of COVID-19 in Portugal: A Comparative Analysis of Active Cases Using Non-linear Regression
Ana Milhinhos, Pedro M. Costa
Frontiers in Public Health.2020;[Epub] CrossRef - Clinical Features and Outcome of SARS-CoV-2 Infection in Children: A Systematic Review and Meta-analysis
Jitendra Meena, Jaivinder Yadav, Lokesh Saini, Arushi Yadav, Jogender Kumar
Indian Pediatrics.2020; 57(9): 820. CrossRef - Fasting Plasma Glucose Level Independently Predicts the Mortality of Patients with Coronavirus Disease 2019 Infection: A Multicenter, Retrospective Cohort Study
Min Cheol Chang, Jong-Moon Hwang, Jae-Han Jeon, Sang Gyu Kwak, Donghwi Park, Jun Sung Moon
Endocrinology and Metabolism.2020; 35(3): 595. CrossRef - Adaptive Feature Selection Guided Deep Forest for COVID-19 Classification With Chest CT
Liang Sun, Zhanhao Mo, Fuhua Yan, Liming Xia, Fei Shan, Zhongxiang Ding, Bin Song, Wanchun Gao, Wei Shao, Feng Shi, Huan Yuan, Huiting Jiang, Dijia Wu, Ying Wei, Yaozong Gao, He Sui, Daoqiang Zhang, Dinggang Shen
IEEE Journal of Biomedical and Health Informatics.2020; 24(10): 2798. CrossRef - Delay-adjusted age- and sex-specific case fatality rates for COVID-19 in South Korea: Evolution in the estimated risk of mortality throughout the epidemic
A.T. Newall, R.N.F. Leong, A. Nazareno, D.J. Muscatello, J.G. Wood, W.J. Kim
International Journal of Infectious Diseases.2020; 101: 306. CrossRef - Transmission dynamics, serial interval and epidemiology of COVID-19 diseases in Hong Kong under different control measures
Yung-Wai Desmond Chan, Stefan Flasche, Tin-Long Terence Lam, Mei-Hung Joanna Leung, Miu-Ling Wong, Ho-Yeung Lam, Shuk-Kwan Chuang
Wellcome Open Research.2020; 5: 91. CrossRef Intensive Care Unit Capacity and Its Associated Risk Factors During the COVID-19 Surge in the Republic of Korea: Analysis Using Nationwide Health Claims Data
Seung Heon Lee, So-Youn Park, Jeong-Yeon Seon, Woo-Hwi Jeon, Sung Il Nam, Jong-Hak Park, Jae Seok Park, Hae-Young Kim, Niket Thakkar, Prashanth Selvaraj, Anna Bershteyn, In-Hwan Oh
Risk Management and Healthcare Policy.2020; Volume 13: 2571. CrossRef- Clinical Features of COVID-19 in Uzbekistan
KyungHee Kim, Jae Wook Choi, Juyoung Moon, Habibulla Akilov, Laziz Tuychiev, Bakhodir Rakhimov, Kwang Sung Min
Journal of Korean Medical Science.2020;[Epub] CrossRef - COVID-19 gender susceptibility and outcomes: A systematic review
Ines Lakbar, David Luque-Paz, Jean-Louis Mege, Sharon Einav, Marc Leone, Andrea Cortegiani
PLOS ONE.2020; 15(11): e0241827. CrossRef - Clinical Outcomes of COVID-19 Patients with Type 2 Diabetes: A Population-Based Study in Korea
Ji Hong You, Sang Ah Lee, Sung-Youn Chun, Sun Ok Song, Byung-Wan Lee, Dae Jung Kim, Edward J. Boyko
Endocrinology and Metabolism.2020; 35(4): 901. CrossRef


 PubReader
PubReader ePub Link
ePub Link Cite
Cite