Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 7(4); 2016 > Article
-
Original Article
Evaluating Service Quality from Patients' Perceptions: Application of Importance–performance Analysis Method - Rafat Mohebifar, Hana Hasani, Ameneh Barikani, Sima Rafiei
-
Osong Public Health and Research Perspectives 2016;7(4):233-238.
DOI: https://doi.org/10.1016/j.phrp.2016.05.002
Published online: May 14, 2016
Department of Health Management, School of Health, Qazvin University of Medical Sciences, Qazvin, Iran
- ∗Corresponding author. sima.rafie@gmail.com
• Received: March 14, 2016 • Revised: April 25, 2016 • Accepted: May 2, 2016
Copyright © 2016 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- Providing high service quality is one of the main functions of health systems. Measuring service quality is the basic prerequisite for improving quality. The aim of this study was to evaluate the quality of service in teaching hospitals using importance–performance analysis matrix.
-
Methods
- A descriptive–analytic study was conducted through a cross-sectional method in six academic hospitals of Qazvin, Iran, in 2012. A total of 360 patients contributed to the study. The sampling technique was stratified random sampling. Required data were collected based on a standard questionnaire (SERVQUAL). Data analysis was done through SPSS version 18 statistical software and importance–performance analysis matrix.
-
Results
- The results showed a significant gap between importance and performance in all five dimensions of service quality (p < 0.05). In reviewing the gap, “reliability” (2.36) and “assurance” (2.24) dimensions had the highest quality gap and “responsiveness” had the lowest gap (1.97). Also, according to findings, reliability and assurance were in Quadrant (I), empathy was in Quadrant (II), and tangibles and responsiveness were in Quadrant (IV) of the importance–performance matrix.
-
Conclusion
- The negative gap in all dimensions of quality shows that quality improvement is necessary in all dimensions. Using quality and diagnosis measurement instruments such as importance–performance analysis will help hospital managers with planning of service quality improvement and achieving long-term goals.
- Quality improvement acts as a strategy to attain a competitive advantage in an industry and improve the reputation and profitability of a health organization during time [1]. All hospitals have found it necessary to measure, monitor, and improve the quality of healthcare services in order to survive and achieve patient satisfaction [2]. Also, the provision of high quality services is crucial to achieve the Millennium Development Goals. Healthcare managers need a thorough understanding of the ways to increase the quality of care in practical terms. Under such circumstances, hospital managers put their main emphasis on attracting as many patients as possible and making loyal customers by recognizing their expectations and trying to respond to them in an effective manner [3]. Davis and colleagues [4] confirmed the necessity of measuring healthcare quality in a competitive environment. Service production in the industry is dramatically different from the healthcare services provision in many aspects: e.g., in terms of service quality assessment, one of the most common ways in healthcare is to use the consumers' (patients) perception about the services provided [5].
- To evaluate patients' satisfaction and expectations of service quality, the SERVQUAL model was introduced by Parasuraman and Zeithaml [6] in 1985. They concluded that customers assess quality by comparing their expectations with real performance insights. If the customer's performance perceptions exceed their expectations, then the service provider provides quality service. The difference in scores determines the level of service quality.
- Many researches have been conducted to assess service quality gap in hospitals and other healthcare organizations worldwide 7, 8, 9, 10, 11, 12, 13, 14, 15. In this study, five dimensions of service quality were measured including tangibility, reliability, responsiveness, assurance, and empathy.
- A principle element in quality assurance, evaluating the current level of performance and developing appropriate strategies for improvement is importance–performance analysis (IPA). This technique is based on a four-quadrant matrix which identifies the strengths and weaknesses of the services and determines improvement opportunities to develop strategic planning. IPA has recently been used to assess service quality in healthcare systems [16]. This method is also beneficial for managerial purposes such as allocating insufficient resources to those areas of performance with considerable effect on consumer satisfaction [17].
- Quality is a multidimensional concept with patient satisfaction as one of the most important facets which mirrors the quality of services in a hospital setting. Patient satisfaction is defined as patients' opinions of “how well” services meet their needs and expectations, also considered as a valid indicator to measure service quality 18, 19. Since the 1990s, patient satisfaction has been considered as a method to measure care recipients' perceptions about the quality of health services and to analyze their willingness to pay or utilize such services provided in healthcare facilities [20]. However, the IPA model is based on comparing the importance level (expected satisfaction) and performance level (perceived satisfaction) of service quality to extract improvement strategies that will be effective for increasing customer satisfaction [21].
- Considering the importance and necessity of evaluating health service quality, particularly those provided in health facilities and hospitals, the current study aimed to evaluate the quality of inpatient services in teaching hospitals affiliated with Qazvin University of Medical Services, Qazvin, Iran using an IPA model.
Introduction
- 2.1 Study design and research setting
- This descriptive–analytic study was carried out through a cross-sectional method in six training hospitals affiliated with Qazvin University of Medical Sciences in 2015. A total of 360 patients from different clinical wards of under-study hospitals contributed to the study (randomly 60 patients from each hospital).
- 2.2 Sample size
- By conducting a literature review, the prevalence of patients' satisfaction was assumed to be 20% with a 95% confidence interval and 5% margin of error. The minimum number of required samples was calculated to be 300 patients. To consider a 20% nonresponse rate, 60 samples were added to this sample size. Therefore, 60 patients were randomly selected from each hospital.
- 2.3 Inclusion criteria
- The inclusion criteria for the study participants were they had to be older than 18 years and had to have been hospitalized for at least 24 hours at the hospital to truly express their attitude toward quality of care. Those inpatients in the intensive care unit, critical care unit, and the emergency ward that had a severe physical condition or mental disorder were extracted from the study.
- 2.4 Data collection tool
- Data collection was conducted using a standard SERVQUAL questionnaire developed by Parasuraman and Zeithaml [6] in 1985. The questionnaire contained an “expectation” section with 22 items and a “perception” section consisting of a set of matching statements. The statements in both expectation and perception sections were categorized into five dimensions of tangibility, reliability, responsiveness, assurance, and empathy. A 5-point Likert scale was used for the scoring system with 1 representing “strongly disagree” and 5 representing “strongly agree.”
- Considering the standard questionnaire, the face and content validity of the questionnaire has been confirmed in previous studies. Also, to assure the questionnaire reliability, Ranjbar Ezzatabadi et al [5] in 2012, Tabibi et al [9] in 2012, and Mohammadi and Shoghli [22] in 2009 calculated the Cronbach α upper as 85%.
- 2.5 Statistical analysis
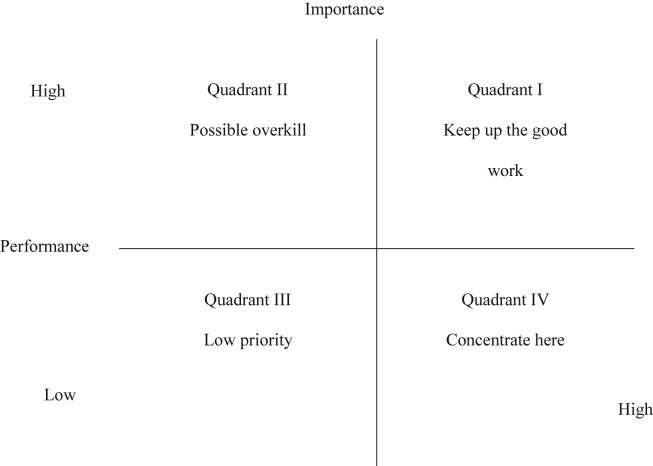
- Statistical analysis was performed using SPSS version 18 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarize patients and hospitals characteristics. A four-quadrant matrix was plotted on the X–Y coordinate plane based on the combination of two factors including patients' perceptions on the current level of performance and the importance of each eight quality dimensions which helped to classify study parameters and use as a main guide for improvement strategies 23, 24. The meanings of these four quadrants are summarized in Figure 1.
- Quadrant I with both a high level of performance and importance represents a priority which needs an immediate action. Quadrant II with high performance but low importance indicates that the organization has over emphasized the related items of this quadrant. Quadrant III with both low performance and importance shows that there is no necessity for improvement, while Quadrant IV requires immediate attention for improvement.
Material and methods
- The majority of participants (60.5%) belonged to the 18–35-year age group in which 73.8% were women and the rest were men. Furthermore, among the studied patients 98% were hospitalized between 1 day and 5 days (Table 1).
- Evaluating the possible relationships between the respondents' characteristics and their perceptions or expectations toward service quality merely confirmed a statistical significant relationship between the patients' length of stay and perception toward service quality, and there was also a significant association between sex and patients' expectation (Table 2).
- Table 3 depicts that in Hospitals A, B, and F, the highest and lowest means of negative gaps were related to reliability (gap score = −3.08, gap score = −2.54, and gap score = −2.32, respectively) and responsiveness (gap score = −2.25, gap score = −2.06, and gap score = −2.07, respectively); in Hospital C the highest and lowest means of negative gaps belonged to assurance (gap score = −1.91) and tangibles (gap score = −1.45); in Hospital D they were related to tangibles (gap score = −2.83) and responsiveness (gap score = −1.57); and, finally, in Hospital E they belonged to empathy (gap score = −2.23) and responsiveness (gap score = −1.79).
- Table 4 depicts the means of the patients' perceptions and expectations related to five quality dimensions for each of the six under-study hospitals. Findings confirmed that the greatest total gap between patients' perception and expectation related to Hospital A, while the least gap belonged to Hospital C. Furthermore, among five quality dimensions, the highest gap was related to reliability and the lowest belonged to responsiveness.
- IPA matrix analysis showed that tangibles and assurance in Hospital A, assurance in Hospital B, reliability and empathy in Hospital D, and assurance and empathy in Hospital C were placed in Quadrant III. As this area represents the least important aspects from the patients' viewpoints, service providers should therefore transfer resources to other sectors that are faced with serious weaknesses. The “keep up the good” quadrant captured quality dimensions of reliability for Hospitals A and B, assurance and reliability for Hospital C, reliability, responsiveness, and tangibility for Hospital F. Being in this area shows that hospitals have performed well in respect to the mentioned quality dimensions and must try to maintain their current status. As per the data provided in Table 5, patients of all hospitals, except for Hospital F, mentioned responsiveness as an important area which required closer attention for improvement (Table 5).
Results
- This study aimed to measure the quality of services provided in under-study hospitals using an IPA model. The study results confirmed a statistically significant difference between the means of patients' expectations and their perceptions in almost all dimensions which were consistent with similar studies 9, 25, 26, 27. Karassavidou and Papadopoulos [11], Baldwin and Sohal [28], Luke [14], and Mohammadi and Shoghli [22] also reported a significant difference between patients' perceptions and expectations toward service quality so that patients' expectations surpassed the actual quality provided for service recipients. Similar to our study, some researchers declared a negative gap between patients' perceptions and expectations in all quality dimensions [29].
- According to the study results, in all hospitals the minimum gap between patients' perceptions and expectations was observed in the responsiveness dimension, while Karydis et al [30] and Lim and Tang [31] achieved completely different results. In this regard, Hekmatpo et al [32] reported that the lowest gap belonged to assurance.
- Through the matrix analysis results showed that in order to maintain a competitive advantage, Hospitals A–D should pay more attention to tangibles, responsiveness, and assurance. Therefore, resources should be allocated to either improve the quality dimensions of the “keep up the good work” quadrant including reliability or resolve the main weaknesses of the “concentrate here” quadrant from patients' points of view. Similar to our findings, Wu et al [33] revealed that reliability and assurance were considered to be in quadrant “keep up the work” which reflects the importance and at the same time acceptable performance of these dimensions. Findings also declared that perceived quality of services was mainly dependant on the tangibility dimension confirming that the highest mean of patients' expectations was related to physical environment, equipment, payment process, and cleanliness. Results reported by Parasuraman and Zeithaml [6] and Boshoff and Gray [34] approved the results and stated that patients' perceptions of quality were mainly affected by environment and physical evidence than the core services. Sohail [10] also emphasized the importance of modern equipment, cleanliness, and visual conditions of facilities in his study.
- To achieve the highest level of quality in hospital services and to determine current gaps, there is a need to evaluate and analyze patients' perceptions toward different quality dimensions and compare it with their expectations of service quality. This study emphasized the IPA model as an applicable tool using an X–Y coordinate plane with a four quadrant matrix, which interprets the current situation of each healthcare provider from the perspective of different quality dimensions. Applying this tool can also help managers improve service quality and patients' satisfaction through emphasizing service recipients' perceptions of importance and performance revealed in each quadrant. Furthermore, decision makers can use the matrix analysis results to allocate scarce resources efficiently by putting more emphasis on areas which need special attention. Such an assessment is essential to reduce costs in todays competitive health market.
Discussion
- The authors have no conflict of interest to declare.
Conflicts of interest
-
Acknowledgements
- The authors appreciate Qazvin University of Medical Sciences and affiliated hospitals which facilitated the gathering data process.
Acknowledgments
- 1. Fitriati R., Rahmayanti K.P.. Government support in Triple Helix Collaboration to provide health service delivery: case study government hospital in Bengkulu Hospital. Procedia Soc Behav Scie 52:2012;160−167.Article
- 2. Punnakitikashem R.N., Buavaraporn P., Leelartapin M.K.. Health care service quality: Case example of a hospital with lean implementation. POMS 23rd Annual Conference, Chicago, IL, USA. 2012.
- 3. Sodani P.. Managing quality in health care. WHO South East Asia J Public Health 1(1). 2012;119−120.Article
- 4. Davis B.A., Kiesel C.K., McFarland A.. Evaluating instruments for quality: testing convergent validity of the consumer emergency care satisfaction scale. J Nurs Care Qual 20(4). 2005 Oct–Dec;364−368. PMID: 16177589.ArticlePubMed
- 5. Ranjbar Ezzatabadi M., Bahrami M.A., Hadizadeh F.. Nurses' emotional intelligence impact on the quality of hospital services. Iran Red Crescent Med J 14(12). 2012 Dec;758−763. PMID: 23482866.ArticlePubMed
- 6. Parasuraman A.V.A., Zeithaml L.L.. A conceptual model of service quality and its implications for future research. J Marketing 29:1985 Sep;41−50.ArticlePDF
- 7. Nekoei-Moghadam M., Amiresmaili M.. Hospital services quality assessment: Hospitals of Kerman University of Medical Sciences, as a tangible example of a developing country. Int J Health Care Qual Assur 24(1). 2011;57−66. PMID: 21456498.ArticlePubMed
- 8. Aghamoulaei T.S., Zare A., Kebriaei A.. Quality gap in primary health care services in Bandar Abbas: Woman's perspective. Payesh 7(2). 2008 Apr;121−127.
- 9. Tabibi S.J., Gohari M.R., Shahri S.. Assessment of health care services in outpatient clinics based on SERVQUAL model in hospitals of Tehran. Payavard Salamat 5(4). 2012;49−56.
- 10. Sohail S.M.. Service quality in hospitals: more favourable than you might think. Manag Serv Qual 13(3). 2003;197−206.Article
- 11. Karassavidou E.N., Papadopoulos C.T.. Quality in NHS hospitals: no one knows better than patients. Meas Bus Excell 13(1). 2009 Mar;34−46.Article
- 12. Anbori A., Ghani H., Yadav A.. Patient satisfaction and loyalty to the private hospitals in Sana'a. Yemen. Int J Qual Health Care 22(4). 2010 Aug;310−315. PMID: 20543208.Article
- 13. Çaha H.. Service quality in private hospitals in Turkey. J Econ Soc Res 9(1). 2007;55−69.
- 14. Al Momani M.. Patient experience of nursing quality in a Teaching Hospital in Saudi Arabia. Iran J Public Health 41(8). 2012;42−49. PMID: 23113223.
- 15. Figen Y., Ebru D.. Health care service quality: A comparison of public and private hospitals. Afr J Bus Manag 4(6). 2010 Jul;962−971.
- 16. Miranda F.J., Chamorro A., Murillo L.R.. An importance-performance analysis of primary health care services: managers vs. patients perceptions. JSSM 3(2). 2010;227−234.Article
- 17. Vandamme R., Leunis J.. The development of multiple-item scale for measuring hospital service quality. Int J Serv Ind Manag 4(3). 1993 Aug;30−49.Article
- 18. Untachai S.. Modeling service quality in hospital as a second order factor. Thailand. Procedia Soc Behav Sci 88:2013 Oct;118−133.Article
- 19. Yunus N., Latiff S.D., Din S.C.. Patient satisfaction with access to 1Malaysia clinic. Procedia Soc Behav Sci 91:2013 May;395−402.Article
- 20. Schulmeister L.K., Mayer K.. Quality of life, quality of care and patient satisfaction: perceptions of patients undergoing outpatient autologous stem cell transplantation. Oncol Nurs Forum 32(1). 2005 Jan;57−67. PMID: 15660144.ArticlePubMed
- 21. Lu Y.M., Wu H.H.. Applying IPA in evaluating service quality requirements of passengers of Taiwan high speed rail. J Qual 17(1). 2010 Jan;21−43.
- 22. Mohammadi A., Shoghli A.. Survey on quality of primary health cares in Zanjan District Health Centers. J Zanjan Univ Med Sci 16(65). 2009 Jun;89−100.
- 23. Olfat L., Barati M.. An importance-performance analysis of supply chain relationships metrics in small and medium sized enterprises in automotive parts industry. J Ind Manag 9:2013;21−42.
- 24. Anderson E.A., Zwelling L.A.. Measuring service quality at the University of Texas MD Anderson Cancer Center. Int J Health Care Qual Assur 9(7). 1996;9−22. PMID: 10162922.Article
- 25. Lotfee A.. Service quality measurement in branches of Eghtesad Novin bank. International Conference on Bank Services Marketing, Tehran 2009;[in Persian].
- 26. Butt M.M., de Run E.C.. Private healthcare quality: applying a SERVQUAL model. Int J Health Care Qual Assur 23(7). 2010;658−673. PMID: 21125961.ArticlePubMed
- 27. Bakar C., Akgun H.S., Al Assaf A.F.. The role of expectations in patient assessments of hospital care: an example from a university hospital network, Turkey. Int J Health Care Qual Assur 21(4). 2008;343−355. PMID: 18785460.ArticlePubMed
- 28. Baldwin A., Sohal A.. Service quality factors and outcomes in dental care. Manag Serv Qual 13(3). 2003;207−216.Article
- 29. Abolghasem Gorji H.S., Tabatabaei A., Akbari S.. Using the service quality gap's model (SERVQUAL) in Imam Khomeini Teaching Hospital. J Health Adm 16(51). 2013 Nov;7−18.
- 30. Karydis A.M., Komboli-Kodovazeniti D., Panis H.V.. Expectations and perceptions of Greek patients regarding the quality of dental health care. Int J Qual Health Care 13(5). 2001 Oct;409−416. PMID: 11669569.ArticlePubMed
- 31. Lim P.C., Tang N.K.. A study of patients' expectations and satisfaction in Singapore hospitals. Int J Health Care Qual Assur Inc Leadersh Health Serv 13(6–7). 2000;290−299. PMID: 11484647.ArticlePubMed
- 32. Hekmatpo D.M., Sorani A., Lashgarara B.A.. Survey on the quality of medical services in teaching hospitals of Arak University of Medical Sciences with SERVQUL model in Arak. AMUJ 15(66). 2012;1−9.
- 33. Wu H.H., Tang Y.T., Shyu J.W.. A case of applying importance-performance analysis in identifying key success factors to develop marketing strategies. Qual Quant 44(6). 2010 Oct;1207−1218.Article
- 34. Boshoff C., Gray B.. The relationship between service quality, customer satisfaction and buying intentions in the private hospital industry. S Afr J Bus Manag 35(4). 2004 Jan;27−37.Article
References
Table 1Descriptive characteristics of respondents.
| Variable | N | % | |
|---|---|---|---|
| Sex | Women | 220 | 73.8 |
| Men | 78 | 28.2 | |
| Age (y) | 18–35 | 180 | 60.5 |
| 35–55 | 94 | 31 | |
| 55–75 | 18 | 6.5 | |
| > 75 | 6 | 2 | |
| Length of hospitalization (d) | 1–5 | 292 | 98 |
| 5–10 | 4 | 1.3 | |
| > 10 | 2 | 0.67 | |
Table 2Association between patients' characteristics and their expectations or perceptions toward service quality.
| Variable |
Expectation |
Perception |
|---|---|---|
| p | p | |
| Age | 0.88 | 0.11 |
| Sex | < 0.05 | 0.32 |
| Education | 0.06 | 0.34 |
| Length of hospitalization (d) | 0.62 | 0.09 |
Table 3Comparison of the quality gap in the five dimensions of quality in hospitals.
Table 4Comparison of the performance–importance gap between hospitals.
Table 5Comparison of the hospitals' situations in the importance performance analysis matrix.
Figure & Data
References
Citations
Citations to this article as recorded by 

- A New Model to Consolidate Long-Term Intersectoral Partnerships in Humanitarian and Social Crises Management
Anderson Nunes da Silva, Marcele Elisa Fontana
Public Organization Review.2024; 24(1): 27. CrossRef - Evaluation of outpatient service quality: What do patients and providers think?
Pouria Farrokhi, Aidin Aryankhesal, Rafat Bagherzadeh, Asgar Aghaei Hashjin
International Journal of Healthcare Management.2023; 16(3): 394. CrossRef - Assessing the Challenges and Opportunities of Agricultural Information Systems to Enhance Farmers’ Capacity and Target Rice Production in Indonesia
Agung Budi Santoso, Setia Sari Girsang, Budi Raharjo, Arlyna Budi Pustika, Yanter Hutapea, Mahargono Kobarsih, Agus Suprihatin, Erpina Delina Manurung, Deddy Romulo Siagian, Sidiq Hanapi, Tommy Purba, Dorkas Parhusip, Sri Wahyuni Budiarti, Yeyen Prestyani
Sustainability.2023; 15(2): 1114. CrossRef - Patients’ views on health promotion and disease prevention services provided by healthcare workers in a South African tertiary hospital
Herbert I. Melariri, Chester Kalinda, Moses J. Chimbari
BMC Health Services Research.2023;[Epub] CrossRef - Telecommunication service quality analysis using integration of SIPA and modified Kano
Hanny Kanavika Rizky Munawar, Annisa Kesy Garside, Adhi Nugraha, Amelia Khoidir
Jurnal Sistem dan Manajemen Industri.2023; 7(1): 53. CrossRef - Identifying service quality gaps between patients and providers in a Native American outpatient clinic
Robert Dorsey, David Claudio, María A. Velázquez, Polly Petersen
BMC Health Services Research.2022;[Epub] CrossRef - Assessing the Utility and Patient Satisfaction of Virtual Retina Clinics During COVID-19 Pandemic
Leire Juaristi, Cristina Irigoyen, Jaione Chapartegui, Ane Guibelalde, Javier Mar
Clinical Ophthalmology.2022; Volume 16: 311. CrossRef - A social-media-based improvement index for urban renewal
Zhifang Wang, Hua Jie, Hongpeng Fu, Lu Wang, Hezhishi Jiang, Lu Ding, Yingjie Chen
Ecological Indicators.2022; 137: 108775. CrossRef - On the comparative use of social media data and survey data in prioritizing ecosystem services for cost-effective governance
Zhifang Wang, Hongpeng Fu, Yuqing Jian, Salman Qureshi, Hua Jie, Lu Wang
Ecosystem Services.2022; 56: 101446. CrossRef - Quality Assessment Methods of Hospital Services from the Viewpoint of Patients Based on Standard Assessment Models in Iran: A Narrative Review
Mehdi Rahimi, Fateme Solymani
Modern Care Journal.2022;[Epub] CrossRef - Responsiveness level and its effect on services quality from the viewpoints of the older adults hospitalized during COVID-19 pandemic
Ali Reza Yusefi, Esmat Rezabeigi Davarani, Salman Daneshi, Misagh Bastani, Gholamhossein Mehralian, Peivand Bastani
BMC Geriatrics.2022;[Epub] CrossRef - Ranking Hospital Hoteling Services from Patients’ Perspective Using Importance-Performance Analysis
Amir Karimkhany, Ehsan Zarei, Samira Arabi, Elahe Navvabi, Somayeh Anisi
Shiraz E-Medical Journal.2022;[Epub] CrossRef - Using the Kano model to associate the number of confirmed cases of COVID-19 in a population of 100,000 with case fatality rates: An observational study
Sheng-Yao Hsu, Tsair-Wei Chien, Yu-Tsen Yeh, Willy Chou
Medicine.2022; 101(37): e30648. CrossRef - Patient satisfaction with quality of care in public hospitals in Albania
Rezarta Kalaja, Marsida Krasniqi
Frontiers in Public Health.2022;[Epub] CrossRef - A Crisis in the Health System and Quality of Healthcare in Economically Developed Countries
Magdalena Biel, Katarzyna Grondys, Ane-Mari Androniceanu
International Journal of Environmental Research an.2022; 20(1): 469. CrossRef - An integrated approach for evaluating hospital service quality with linguistic preferences
Xiaobing Li, Zhen He
International Journal of Production Research.2021; 59(6): 1776. CrossRef - Rethinking health services operations to embrace patient experience of healthcare journey
Mahdi Mahdavi, Leila Doshmangir, Ebrahim Jaafaripooyan
The International Journal of Health Planning and M.2021; 36(6): 2020. CrossRef - A STUDY ON QUALITY OF SERVICES IN THE OUTPATIENT DEPARTMENT OF A MULTISPECIALTY TEACHING HOSPITAL
Nirmala Kumari, Keerthana Maria Pinto
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 117. CrossRef - Variation in compliance with safe surgery checklist in hospitals with different levels of patient safety culture
Saeed Asefzadeh, Sima Rafiei, Masoomeh Karimi
International Journal of Healthcare Management.2020; 13(sup1): 12. CrossRef - Assessment of Quality of Services Delivered to Iranian Patients with Cataract
Zahra Hashemi Dehaghi, Soad Mahfoozpour, Mahmoud Modiri, Fateme Alipour
Iranian Red Crescent Medical Journal.2020;[Epub] CrossRef - Gap between patient expectation and perception during pharmacist–patient communication at community pharmacy
Myeong Gyu Kim, Na Eun Lee, Hyun Soon Sohn
International Journal of Clinical Pharmacy.2020; 42(2): 677. CrossRef - Validating Service Quality (SERVQUAL) in Healthcare: Measuring Patient Satisfaction Using their Perceptions in Jordan
Mohammed Shaker Ibrahim
Journal of Information & Knowledge Management.2020; 19(01): 2040021. CrossRef - Evaluating the environmental protection strategy of a printed circuit board manufacturer using a T fuzzy importance performance analysis with Google Trends
Kuen-Suan Chen, Kuo-Ping Lin, Li-Ju Lin
Expert Systems with Applications.2020; 156: 113483. CrossRef - Methodologies for Determining the Service Quality of the Intercity Rail Service Based on Users’ Perceptions and Expectations in Thailand
Sajjakaj Jomnonkwao, Thanapong Champahom, Vatanavongs Ratanavaraha
Sustainability.2020; 12(10): 4259. CrossRef - Patients’ Views on Service Quality in Selected Iranian Hospitals: An Importance-Performance Analysis
Ehsan Zarei, Ali Bagheri, Abbas Daneshkohan, Soheila Khodakarim
Shiraz E-Medical Journal.2020;[Epub] CrossRef - Identification of quality gaps in healthcare services using the SERVQUAL instrument and importance-performance analysis in medical intensive care: a prospective study at a medical center in Taiwan
Shu-Ju Lu, Hsiu-O Kao, Bao-Lin Chang, Shu-Ing Gong, Shu-Mei Liu, Shih-Chi Ku, Jih-Shuin Jerng
BMC Health Services Research.2020;[Epub] CrossRef - Importance – Performance Analysis (IPA) of bus service attributes: A case study in a developing country
Javad Esmailpour, Kayvan Aghabayk, Mohammad Abrari Vajari, Chris De Gruyter
Transportation Research Part A: Policy and Practic.2020; 142: 129. CrossRef - The Effect of Quality Service Towards Outpatients Satisfaction at Poasia Community Health Centre
Adryan Fristiohady, La Ode Muhammad Fitrawan, Yusniati Dwi Pemudi, Ruslin Ruslin, Sunandar Ihsan, Ruslan Ruslan, La Ode Muhammad Julian Purnama
Borneo Journal of Pharmacy.2020; 3(4): 270. CrossRef - Gap of services quality expectation and perception based on SERVQUAL model in the selected hospital outpatient clinics affiliated with Iran University of Medical Sciences
asgar Aghaei Hashjin, Pouria Farrokhi, Aidin Aryankhesal
Journal of Health Administration.2020; 23(3): 55. CrossRef - An empirical study of willingness to renewable energy installation using importance-performance analysis: the case of Taiwan
Wei-Chuan Chen, Wen-Kuo Chen, Chien-Wen Chen, Chien-Cheng Lo
Journal of Industrial and Production Engineering.2019; 36(7): 451. CrossRef - Assessing management performance of the national forest park using impact range-performance analysis and impact-asymmetry analysis
Pin-Zheng Chen, Wan-Yu Liu
Forest Policy and Economics.2019; 104: 121. CrossRef - Do patients really perceive better quality of service in private hospitals than public hospitals in India?
Swapnarag Swain
Benchmarking: An International Journal.2019; 26(2): 590. CrossRef - Percepción de los usuarios frente a la calidad de atención en salud del servicio de consulta externa según el modelo SERVQUAL
Angélica Viviana Boada-Niño, Adriana Mayeth Barbosa-López, Elisa Andrea Cobo-Mejía
Revista Investigación en Salud Universidad de Boya.2019; 6(1): 55. CrossRef - Application of the SERVQUAL model to evaluate the quality in the transportation service in Morelia, Mexico
Marco Alberto Valenzo-Jiménez, Daniel Adan Lazaro-López, Jaime Apolinar Martínez- Arroyo
DYNA.2019; 86(211): 64. CrossRef - Konya İlinde Bulunan Özel Hastanelerdeki Hizmet Kalitesinin Ölçülmesi: Akademik Personele Yönelik Araştırma
Büşra Güler, Saadettin Erhan Kesen
Selçuk Üniversitesi Sosyal Bilimler Meslek Yükseko.2019; 22(2): 526. CrossRef - A Study on Service Quality and Customer Satisfaction in Nigerian Healthcare Sector
Rajasekhara Mouly Potluri, Gift Angiating
Journal of Industrial Distribution & Business.2018; 9(12): 7. CrossRef - Analysis of customer satisfaction in hospital by using Importance-Performance Analysis (IPA) and Customer Satisfaction Index (CSI)
Vembri Noor Helia, Cahya Putra Abdurrahman, Fety Ilma Rahmillah, S. Ma’mun, H. Tamura, M.R.A. Purnomo
MATEC Web of Conferences.2018; 154: 01098. CrossRef - Evaluating health service quality: using importance performance analysis
Azar Izadi, Younes Jahani, Sima Rafiei, Ali Masoud, Leila Vali
International Journal of Health Care Quality Assur.2017; 30(7): 656. CrossRef - Societal perception toward transportation modes based on online (Go-Jek) In Malang City
D M Buamona
IOP Conference Series: Earth and Environmental Sci.2017; 70: 012007. CrossRef - The Role of Subjective Culture on Consumer Perception towards Service Quality Delivery
Tiara Turay
Journal of Business and Social Review in Emerging .2016; 2(2): 175. CrossRef


 PubReader
PubReader Cite
Cite
