Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 15(1); 2024 > Article
-
Original Article
Risk factors for SARS-CoV-2 transmission during a movie theater outbreak in Incheon in the Republic of Korea, November 2021: a retrospective study -
Hye Young Lee1,2
 , Young-Joon Park1,2
, Young-Joon Park1,2 , Sang-Eun Lee2
, Sang-Eun Lee2 , Han-Na Yoo3
, Han-Na Yoo3 , Il-Hwan Kim4
, Il-Hwan Kim4 , Jin Sun No4
, Jin Sun No4 , Eun-Jin Kim4
, Eun-Jin Kim4 , Jungyeon Yu5
, Jungyeon Yu5 , Sanghwan Bae5
, Sanghwan Bae5 , Mi Yu1,2
, Mi Yu1,2
-
Osong Public Health and Research Perspectives 2024;15(1):45-55.
DOI: https://doi.org/10.24171/j.phrp.2023.0269
Published online: January 31, 2024
1Division of Epidemiological Investigation Analysis, Bureau of Public Health Emergency Preparedness Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
2Team of Epidemiological Investigation, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
3Department of Infectious Disease Control, Bureau of Health & Sports, Incheon Metropolitan Government, Incheon, Republic of Korea
4Division of Emerging Infectious Diseases, Bureau of Infectious Disease Diagnosis Control, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
5Department of Building Research, Korea Institute of Civil Engineering and Building Technology, Goyang, Republic of Korea
- Co-Corresponding author: Young-Joon Park Team of the Epidemiological Investigation, Korea Disease Control and Prevention Agency, Osong Health Technology Administration Complex, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: pahmun@korea.kr
- Corresponding author: Sang-Eun Lee Team of Epidemiological Investigation, Korea Disease Control and Prevention Agency, Osong Health Technology Administration Complex, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: ondalgl@korea.kr
© 2024 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 10,674 Views
- 327 Download
Abstract
-
Objectives
- We examined factors contributing to the transmission of an acute respiratory virus within multi-use facilities, focusing on an outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a movie theater in the Republic of Korea.
-
Methods
- This retrospective cohort study involved a descriptive analysis of 48 confirmed cases. Logistic regression was applied to a cohort of 80 theater attendees to identify risk factors for infection. The infection source and transmission route were determined through gene sequencing data analysis.
-
Results
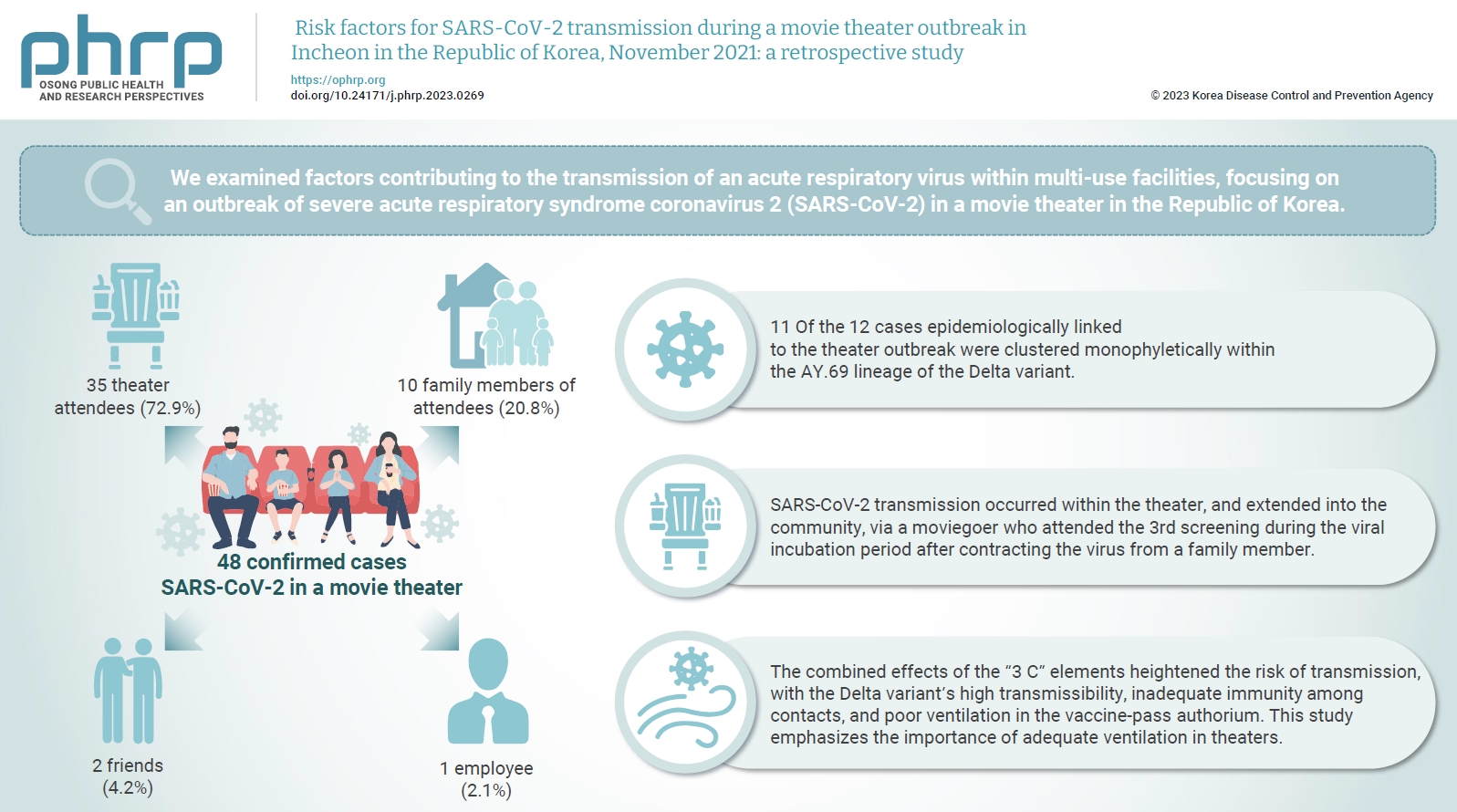
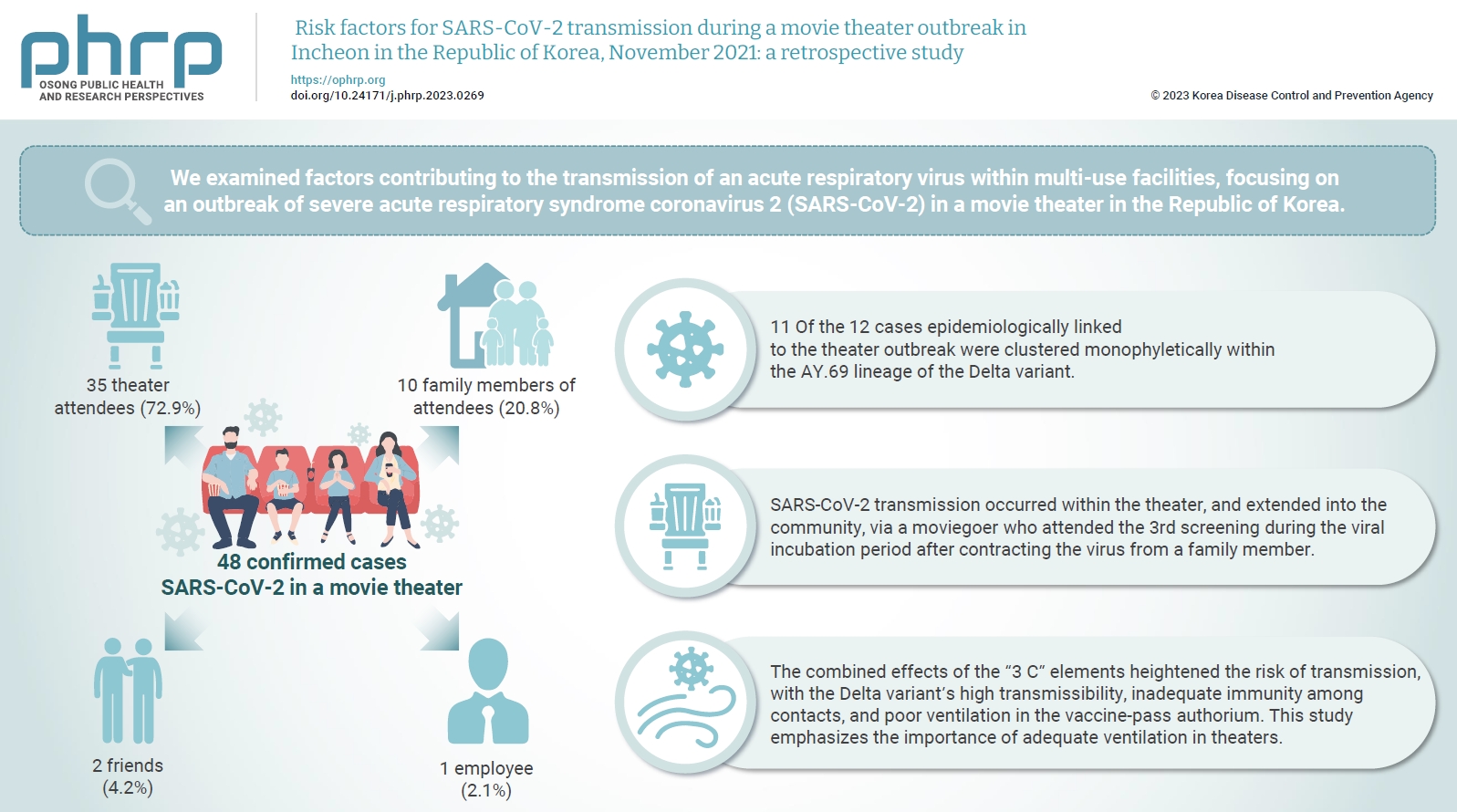
- Of the 48 confirmed cases, 35 were theater attendees (72.9%), 10 were family members of attendees (20.8%), 2 were friends (4.2%), and 1 was an employee (2.1%). Among the 80 individuals who attended the 3rd to 5th screenings of the day, 35 became infected, representing a 43.8% attack rate. Specifically, 28 of the 33 third-screening attendees developed confirmed SARS-CoV-2, constituting an 84.8% attack rate. Furthermore, 11 of the 12 cases epidemiologically linked to the theater outbreak were clustered monophyletically within the AY.69 lineage. At the time of the screening, 35 individuals (72.9%) had received 2 vaccine doses. However, vaccination status did not significantly influence infection risk. Multivariate analysis revealed that close contacts had a 15.9-fold higher risk of infection (95% confidence interval, 4.37–78.39) than casual contacts.
-
Conclusion
- SARS-CoV-2 transmission occurred within the theater, and extended into the community, via a moviegoer who attended the 3rd screening during the viral incubation period after contracting the virus from a family member. This study emphasizes the importance of adequate ventilation in theaters.
- In the early stages of the coronavirus disease 2019 (COVID‐19) pandemic, the primary mode of transmission for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was considered to be respiratory droplets within a 2-meter radius of infected individuals [1,2]. Consequently, initial public health measures to control SARS-CoV-2 infection focused on social distancing [3–5]. However, reports of transmission occurring at greater distances from infected persons have emerged worldwide, suggesting airborne transmission as a major route and emphasizing the importance of ventilation over social distancing [6]. In the Republic of Korea, the critical role of indoor ventilation was increasingly recognized following large-scale infections in March 2021, which were thought to be due to airborne transmission in fitness and call centers [7–10]. In May 2021, the World Health Organization and the United States Centers for Disease Control and Prevention officially acknowledged the potential for airborne transmission of SARS-CoV-2 in indoor settings that are poorly ventilated and crowded for prolonged periods [11,12].
- As the approach to quarantine measures evolved, the need for proper indoor ventilation in theaters was not adequately addressed. On November 1, 2021, the government of the Republic of Korea introduced the “living with COVID-19” strategy. This was prompted by the achievement of a 70% nationwide completion rate of the second dose of the SARS-CoV-2 vaccine (as of October 26, 2021), along with a gradual decrease in the number of confirmed cases in the country [13]. In response, major multiplex operators began to designate certain screens as “vaccine-pass” auditoriums. These screens were accessible to individuals who had received both vaccine doses or who could present a negative real-time polymerase chain reaction (RT-PCR) test result from within the previous 48 hours, excluding minors under 19 years old. Unlike a general auditorium, a vaccine-pass auditorium had no policy of maintaining an empty seat between audience members, and eating and drinking were permitted during the movie. However, after a SARS-CoV-2 infection outbreak in a cinema, a reassessment of the health and safety policies of theaters was initiated. As a result, beginning on December 6, 2021, all screens were restricted to allow entry only to vaccinated individuals, again excluding minors; additionally, the consumption of food, excluding water and other beverages, was banned [14].
- The potential for respiratory virus transmission via droplets and aerosolized particles in enclosed indoor settings, often described by the 3 “Cs” (close contact, confined spaces, and crowded places), was acknowledged prior to the SARS-CoV-2 pandemic [15]. Nevertheless, documented instances of large-scale outbreaks of respiratory infections occurring in theaters are rare on a global scale. In the present case, not only were theatergoers attending the 3rd screening of the day directly exposed to the infection source, but attendees of the subsequent screening, theater employees, family members, and friends were also confirmed through genetic analysis to have contracted the same viral genotype. This case carries serious implications, highlighting the extensive reach of transmission beyond the initial group exposed in the theater and eventually impacting the wider community. Moreover, it underscores the critical need for prioritizing quarantine measures in theaters, where people exist in close quarters for prolonged periods, even without engaging in strenuous physical activity.
- Therefore, the objective of this study was to identify the risk factors associated with SARS-CoV-2 transmission in theater settings. To achieve this, we formulated hypotheses that considered epidemiological elements—specifically, the pathogen, host, and environment—that contribute to disease occurrence. These hypotheses were then subjected to rigorous scientific scrutiny and analysis.
Introduction
- Outbreak Recognition
- On November 3, 2021, an Incheon resident attended the 3rd screening of the day at a local theater. By November 6, 2021, she began to experience symptoms such as muscle pain and headaches, and SARS-CoV-2 infection was confirmed that day. While monitoring local SARS-CoV-2 incidence, the Incheon metropolitan government identified additional confirmed cases that corresponded with the theater name, the date of the visit, and the screening time of the initial confirmed patient who had attended the theater. In response, the government conducted RT-PCR tests on audience members who attended the 3rd screening, as well as on the theater staff, in accordance with the guidelines outlined in Article 18 of the Infectious Disease Prevention and Control Act [16]. When the number of confirmed cases reached 10, the situation was classified as a theater outbreak. To minimize community transmission, the testing was then extended to include individuals who had attended subsequent screenings. In addition, the Incheon metropolitan government and the local public health clinic conducted a preliminary field epidemiological investigation to evaluate the risk of transmission within the theater, adhering to the COVID-19 response guidelines [14].
- Case Definition and Study Population
- This investigation was conducted as a retrospective cohort analysis. Confirmed cases were identified as individuals with infection verified by RT-PCR, irrespective of the presence of clinical symptoms [14]. In the context of this outbreak, the patient with the earliest diagnosis date was considered the index case. The suspected primary case was identified as the confirmed case that presented with the earliest symptom onset, as established by the basic epidemiological investigation. Among the potential sources of infection linked to the suspected primary case, the source with the earliest onset of symptoms was designated as the preceding source of infection.
- The case definition for this study included individuals who attended the 3rd to 5th screenings of the day as well as staff members working at the theater in Incheon on November 3, 2021. It also encompassed patients who came into contact with a confirmed theater-related case during the infectious period, spanning from 2 days before to 14 days after symptom onset, and who subsequently tested positive for the infection. By November 23, 2021, a total of 48 individuals, comprising audience members, theater staff, family members, and friends, fulfilled the case definition criteria. However, of the 92 audience members who attended the 3rd, 4th, and 5th screenings, only 80 were selected for the associated analysis of risk factors. The remaining 12 were excluded due to inconsistencies between the reservation information and the actual details of the attendees.
- Epidemiological Investigation
- On November 24, 2021, we conducted an extensive field epidemiological investigation in collaboration with the Korea Institute of Construction Technology, with the goal of examining facility-related risk factors.
- First, we conducted a thorough assessment of the structural characteristics of the building housing the theater. The theater auditoriums occupy the 4th to 7th floors of a building with 7 underground and 7 above-ground levels. Specifically, auditoriums numbered 1 through 6 are found on the 4th floor, while auditoriums 7 through 14 are on the sixth floor. The outbreak took place in auditorium 13, which has a stadium-style layout and a seating capacity of 213 people. The index case was present at the 3rd of 5 screenings held that day, and the movie was approximately 3 hours long—double the length of a typical film.
- The auditorium was equipped solely with natural ventilation, facilitated by 2 doors. The entrance was positioned on the left side at the rear of the seating area, while the exit was situated on the left side near the screen. This arrangement presented difficulties in providing adequate ventilation on the right side of the space.
- During interviews with theater managers, we sought detailed information regarding the ventilation system. These managers reported that approximately 5 minutes separated the exit of an audience and the entry of the next group, during which time intensive ventilation was achieved by opening doors and introducing 100% outdoor air. However, the absence of recorded data from the heating, ventilation, and air conditioning (HVAC) systems posed a challenge in verifying specific operational details. We also reviewed the operation manual for the auditorium’s automatic HVAC system. While the system’s capacity was considered adequate for the size of the auditorium, the operational guidelines were not explicitly stated. Notably, the manual lacked specifics on the duration of operation and the proportion of outside air introduced during a movie’s runtime. Furthermore, the air conditioning system was not providing cooling at the time of viral transmission, due to prevailing cool weather conditions.
- Consequently, we inferred that inadequate indoor ventilation may have contributed to the risk of airborne transmission. Additionally, we contemplated the potential for short-range droplet transmission, given the low airflow speed [17].
- Case Investigation
- The Incheon metropolitan government compiled a list of individuals who were potentially exposed to the virus by utilizing a visitor management system known as “Safety Call for Entry Control.” This system automatically logs the date and time of entry when a visitor dials the facility’s unique number. Subsequently, text messages were dispatched to these individuals, recommending that they undergo testing for SARS-CoV-2. Local public health clinics interviewed individuals who tested positive, generated basic epidemiological investigation reports, traced the contacts of confirmed cases, and uploaded collected information to the COVID-19 information management system of the Korea Disease Control and Prevention Agency (KDCA). This digital surveillance system enabled us to access information about confirmed cases and their contacts. Additionally, we obtained data on the SARS-CoV-2 vaccination status of the study population from the KDCA’s COVID-19 vaccination management system. The Korea Institute of Construction Technology assessed the adequacy of ventilation and the patterns of airflow within the auditorium. To determine the genetic relationship of the virus found in confirmed cases, the KDCA’s Division of Emerging Infectious Diseases conducted whole-genome sequencing on viral RNA extracted from nasopharyngeal swab samples that tested positive for SARS-CoV-2, with a cycle threshold of less than 30 for the E and N genes. The sequences were aligned using MAFFT ver. 7 (https://mafft.cbrc.jp/alignment/server/index.html) [18], and maximum likelihood phylogenetic trees were created using Fast Tree ver. 2.1.9 (http://www.microbesonline.org/fasttree) [19]. A total of 77 genome sequences were submitted to the Global Initiative on Sharing All Influenza Data (Supplementary Material 1).
- Data Analysis
- Descriptive statistics, presented as percentages, were utilized to examine differences in demographic, clinical, and epidemiological characteristics among the 48 confirmed cases identified during the epidemiological investigation of this outbreak. Risk factors for infection were examined using univariate and multivariate logistic regression analyses, with adjustments for potential confounding variables of SARS-CoV-2 infection among the 80 attendees of the 3rd to 5th screenings. In line with the Republic of Korea vaccination policy at the time, minors (those under 19 years old) were not eligible for vaccination. Consequently, we categorized the study population into 2 groups based on this age cutoff. Contacts were classified based on the criteria for determining contacts of individuals with airborne-transmitted tuberculosis during flights. Specifically, attendees seated in the same row as the index case, as well as those in the 2 rows in front of and the single row behind that individual, were designated as close contacts. All other attendees were deemed casual contacts [20,21]. R ver. 4.1.0 (The R Foundation) was used for statistical analysis, and an alpha level of 0.05 was employed to determine statistical significance. Values were presented along with 95% confidence intervals (CIs).
- IRB/IACUC Approval
- This study was reviewed and approved by the Institutional Review Board of the KDCA (No: KDCA-2023-05-04-PE-01) and was performed in accordance with the principles of the Declaration of Helsinki. Due to the retrospective nature of the study, the requirement for informed consent was waived.
Materials and Methods
- Descriptive Analysis
- To understand the temporal pattern of the outbreak, we constructed an epidemic curve based on the symptom onset date for symptomatic patients and the confirmation date for asymptomatic cases. The curve indicated a single exposure outbreak with a propagated pattern, suggesting that infections occurred continuously through person-to-person transmission following shared exposure to a common vehicle during the movie screening on November 3, 2021. Within the group of epidemiologically linked confirmed cases, members of 1 household exhibited symptoms starting on November 4, 2021, representing the likely source of the infection. Furthermore, since symptoms began among the moviegoers 2 days after the screening, the minimum incubation period was considered to be 2 days (Figure 1).
- A spot map was created to assess the spatial distribution of the outbreak. Audience members were seated in close proximity to each other without social distancing, predominantly in the rear seats. During the 3rd screening, most individuals identified as close contacts contracted the virus. In contrast, for the 4th screening, the outbreak was not confined to a particular area; rather, the confirmed cases were more uniformly dispersed throughout the venue (Figure 2).
- Of the 48 confirmed cases, the majority were theater attendees, at 35 individuals (72.9%). They were followed by 10 family members (20.8%), 2 friends (4.2%), and 1 member of the janitorial staff (2.1%). At the time of diagnosis, 38 patients (79.2%) presented with symptoms, and 35 (72.9%) had completed secondary vaccination. The confirmed cases had potential contact points not only in the movie theater but also in their homes and schools (Table 1).
- Hypothesis Formulation
- Based on the results of the descriptive analysis, we established the following hypotheses concerning the cause of the outbreak.
- First, the transmission of SARS-CoV-2 within the theater is believed to have originated from a primary case who, despite being asymptomatic, had contracted the virus through contact with a household member. Furthermore, the immune responses among individuals who had received a second vaccine dose were inadequate in preventing SARS-CoV-2 infection. Finally, insufficient indoor ventilation in the auditorium substantially contributed to a widespread outbreak, which then extended into the local community.
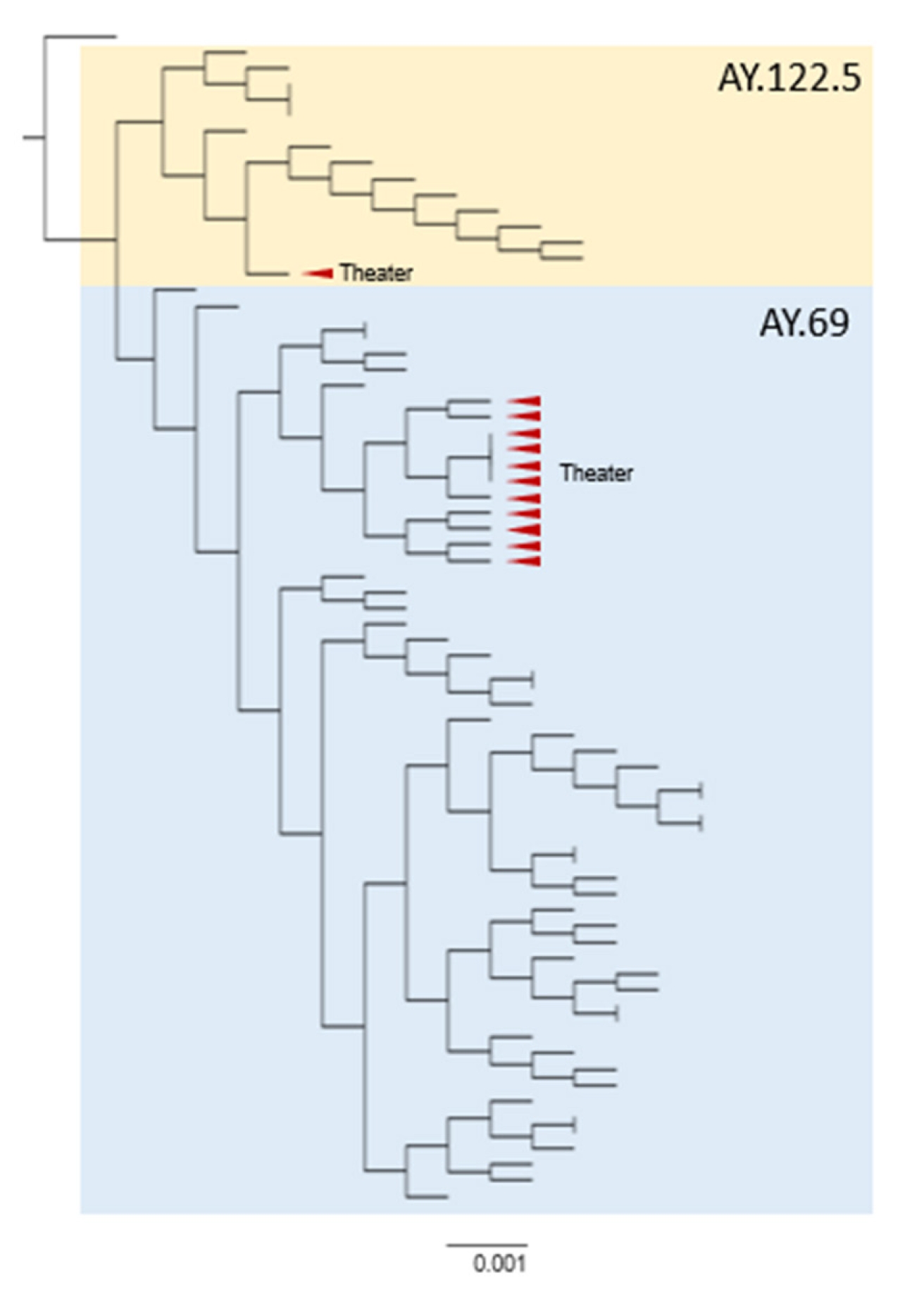
- Gene Sequencing Analysis
- Next-generation sequencing analysis was performed on 77 cases—12 cases from the theater outbreak and 65 domestically identified positive cases from the same timeframe—to determine the source of infection and the molecular pathways of transmission. All cases were confirmed to have been caused by the SARS-CoV-2 Delta variant. Within the theater outbreak, 11 of the 12 cases were found to cluster within the AY.69 lineage (Figure 3). The remaining case from this outbreak was classified as belonging to the AY.122.5 lineage. Through genetic analysis and epidemiological investigation, a transmission chain was established (Figure 4). Experimental evidence confirmed that transmission occurred during a screening in the theater and continued into the subsequent screening, confirming airborne transmission. Infection also spread to family members and friends within the community.
- Risk Factor Analysis
- Among the 80 participants who attended the 3rd to 5th screenings, 35 individuals were confirmed to have contracted SARS-CoV-2 infection. This represents an attack rate of 43.8% within the theater (95% CI, 33.4%–54.7%). While only slight differences in attack rate were observed based on demographic characteristics such as sex and age, significant variations were observed with respect to epidemiological factors. Specifically, of the 33 participants who attended the 3rd screening, 28 tested positive, corresponding to an attack rate of 84.4% (95% CI, 69.1%–93.3%). In contrast, 7 of 37 attendees at the 4th screening were confirmed to have the infection, constituting an attack rate of 18.9% (95% CI, 69.1%–93.3%). No cases were detected among attendees of the 5th screening. Notably, all 6 individuals who consumed food during the movie screening tested positive for SARS-CoV-2. Regarding vaccination status, the attack rate was 70.0% (95% CI, 39.7%–89.2%) for those who had received 1 or fewer doses of the vaccine, compared to 40.0% (95% CI, 29.3%–51.7%) for those who had received 2 doses. With regard to proximity of exposure, the attack rate among casual contacts was 31.1 (95% CI, 20.9–43.6), while it was 84.2% (95% CI, 62.4%–94.5%) among close contacts.
- To evaluate the risk factors associated with transmission, we conducted univariate and multivariate analyses, adjusting for potential confounders such as sex, age, screening attended, food consumption, vaccination status, and proximity of exposure. At the time of movie viewing, 35 individuals (72.9%) had received 2 vaccine doses, a status that was associated with 0.2-fold lower risk ratio (RR) (95% CI, 0.02–1.26) of infection compared to those with 1 or fewer doses, according to multivariable logistic regression analysis. However, this difference was not statistically significant. Significant associations were only detected in the analyses concerning screening attended and proximity of exposure. Relative to the 4th screening, the RR for the 3rd screening was 24.0 (95% CI, 7.4–93.8), while for close contacts, the RR was 11.8 (95% CI, 3.44–55.17) when compared to casual contacts. Moreover, the RR for close contacts rose to 15.9 (95% CI, 4.37–78.39) in the multivariable logistic regression analysis (Table 2).
Results
- We investigated risk factors for acute respiratory virus transmission in multi-use facilities through a case study of a SARS-CoV-2 outbreak in a movie theater. Throughout the infectious period, from November 3, 2021 to November 23, 2021, we identified 48 confirmed cases linked to the theater. Specifically, during the 3rd screening—which included the suspected primary case—28 of 33 attendees contracted the virus, representing an extremely high attack rate of 84.8%. Univariate analysis revealed that the risk of SARS-CoV-2 infection during the 3rd screening was 24 times greater than during the 4th screening, indicating direct airborne transmission. Moreover, after adjusting for potential confounding variables, individuals in close contact with the index case exhibited a RR approximately 15 times that of casual contacts. The extent of and risk factors identified in this outbreak underscore the potential for theater settings to become key hotspots for SARS-CoV-2 transmission, contributing to the spread of the virus.
- In this study, we focused on exploring the transmission dynamics of SARS-CoV-2 within a theater environment by employing hypothesis testing methods. The results provide important insights into the various factors facilitating the rapid spread of the virus in a theater.
- First, the high transmissibility of the Delta variant played a crucial role. Studies have shown that the Delta variant replicates more quickly within the body than non-variant viruses, with initial viral loads during infection reportedly 20 to 300 times higher than those seen in previous waves [22]. Notably, the Delta variant is characterized by increased viral shedding before the onset of symptoms and a higher volume of virus shed compared to earlier variants, which are critical factors in its rapid spread [23]. Given these virological characteristics, it is likely that the suspected primary case, who contracted the virus from a household contact, transmitted the virus in the theater during the pre-symptomatic incubation period [22,24,25].
- Second, the diminished immune response observed among individuals exposed to the Delta variant is of considerable importance. The basic reproduction number (R0) for the original coronavirus strain is 2.79, whereas the Delta variant exhibits an R0 of 5.08, reflecting its greater transmissibility [26]. Of the 80 theater attendees, 70 individuals (87.5%) had received a second vaccine dose and fell beyond the 14-day post-vaccination period; however, no significant difference was found in incidence risk based on vaccination status. Research from various sources, including the US Centers for Disease Control and Prevention, indicates that the protective effectiveness of vaccines developed against the original coronavirus strain is substantially diminished for the Delta variant [27]. Consequently, even the immunity conferred by a second vaccine dose appears inadequate in combating the Delta variant’s more formidable epidemiological characteristics.
- Lastly, inadequate ventilation that leads to indoor air contamination represents an additional risk factor. Next-generation sequencing analysis confirmed that the genotype present in attendees of the 3rd screening was also found in audience members at the following screening, as well as family and friends. This suggests transmission among attendees through shared contaminated air in the theater, with further spread to the community via direct and indirect contact. A multidisciplinary systematic review indicated that ventilation rates and airflow patterns are directly associated with the airborne diffusion of infectious agents [28]. In the present case, when the HVAC system is active in the auditorium, air is drawn out through exhaust vents located on the back walls of the seating area. This air is then purified by the system to remove contaminants before being supplied back into the room through ceiling vents. The ventilation and airflow investigation in this study revealed that the HVAC system was set to internal circulation mode, causing indoor air to diffuse throughout the entire auditorium within 3 minutes. If the filtration capacity of this system is inadequate, and if proper ventilation and expulsion of contaminated air are not achieved, the system faces the risk of recirculating contaminated air, leading to cross-contamination. Notably, the rear seats are particularly impacted by the HVAC system and are more vulnerable to air circulation issues due to the smaller space between the ceiling and the floor.
- Transmission of SARS-CoV-2 can also occur through contact with surfaces or objects that have been contaminated with the virus, followed by touching the mouth, nose, or eyes with hands that have not been cleaned [2]. However, the virus does not exhibit high survival on surfaces [14]. Moreover, the risk of transmission via fomites is deemed to be low due to widespread adherence to personal hygiene practices, including mask-wearing and hand hygiene [29].
- This study had several limitations. First, we were unable to confirm whether the index case and the suspected primary cases were infected with the same viral genotype, due to the lack of a specimen for genetic analysis from the index case. Second, the omission of 12 attendees from the 3rd to 5th screenings because of incomplete personal information may have contributed to an overestimation of the attack rate within the theater. Third, this case reflects an outbreak influenced by a variety of epidemiological factors; therefore, it should not be generalized as a definitive instance of airborne transmission in movie theaters overall. Moreover, the potential contribution of mask usage to transmission cannot be dismissed, as no survey has been conducted to assess the mask-wearing rate and the types of masks used by audiences. Given the ongoing COVID-19 pandemic, theaters, as popular cultural venues, have implemented rigorous control and management measures. Consequently, it is crucial to also develop comprehensive infection prevention protocols for these settings. This necessitates a quantitative analysis of the dynamic properties of respiratory viruses, which underscores the need for additional research in the future.
Discussion
- In summary, this study substantially contributes to an understanding of the mechanisms of acute respiratory infection spread in multi-use facilities. This was specifically accomplished by analyzing the risk factors for SARS-CoV-2 transmission in a theater. The combined effects of the “3 C” elements heightened the risk of transmission, with the Delta variant’s high transmissibility and inadequate immunity among contacts further accelerating the spread. Additionally, poor ventilation and suboptimal operation of the HVAC systems led to increased indoor air pollution, enabling wider virus dissemination. These findings underscore the need for a range of management strategies and infection control protocols to improve the safety of multi-use facilities. In particular, they emphasize the importance of ensuring that cultural venues, such as theaters, are safe environments. Future research should be focused on analyzing the effects of ventilation and sanitation measures through simulations, with the goal of developing practical guidelines applicable to real-world settings.
Conclusion
- • Our objective was to identify risk factors for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission during an outbreak originating in a movie theater in November 2021.
- • Next-generation sequencing analysis confirmed that attendees of the 3rd screening of the day shared a viral genotype not only with individuals from the subsequent screening with whom they had no direct contact, but also with family members and friends.
- • Inadequate ventilation and audience proximity in the auditorium were key factors in the SARS-CoV-2 outbreak.
- • Insights from this study may contribute to the improvement of multi-use facilities and highlight the importance of establishing safe environments within cultural venues, including theaters.
HIGHLIGHTS
Supplementary Material
-
Ethics Approval
This study was reviewed and approved by the Institutional Review Board of the KDCA (No: KDCA-2023-05-04-PE-01) and was performed in accordance with the principles of the Declaration of Helsinki. Due to the retrospective nature of the study, the requirement for informed consent was waived.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
This investigation was conducted as part of a primary initiative of the Center for Epidemiological Investigation and Analysis at the KDCA. The name of this initiative is “Reinforcement of epidemiological investigation capacity and establishment of a research base” (grant No: 6231-3335-210-01).
-
Availability of Data
The SARS-CoV-2 whole-genome sequences have been submitted to the Global Initiative on Sharing All Influenza Data (GISAID) EpiCoV database (http://gisaid.org). The GISAID accession IDs for these sequences can be found in Supplementary Material 1.
-
Authors’ Contributions
Conceptualization: HYL, YJP, SEL; Data curation: HNY, IHK, JSN; Formal analysis: HYL, YJP; Funding acquisition: MY, SEL; Investigation: HNY, HYL, YJP, JY, SB, IHK, JSN, MY; Methodology: HYL, YJP, SEL, JY, SB, IHK, EJK; Project administration: YJP, SEL; Resources: YJP, SEL, EJK; Software: HYL, IHK, JSN; Supervision: YJP, SEL, EJK; Visualization: HYL, IHK, JSN; Writing–original draft: HYL, YJP; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Acknowledgements
The authors thank the movie theater for its cooperation in field epidemiological investigations and the evaluation of ventilation conditions. In addition, we would like to thank the COVID-19 managers at the local public health clinics in Incheon Metropolitan City for their efforts to respond to COVID-19.
Article information



| Characteristic | Confirmed case |
|---|---|
| Total | 48 (100.0) |
| Sex | |
| Male | 30 (62.5) |
| Female | 18 (37.5) |
| Age (y) | |
| ≤19 | 10 (20.8) |
| 20–29 | 21 (43.8) |
| 30–39 | 3 (6.3) |
| 40–49 | 6 (12.5) |
| 50–59 | 1 (2.1) |
| 60–69 | 4 (8.3) |
| ≥70 | 3 (6.3) |
| Classification | |
| Third screening audience | 28 (58.3) |
| Fourth screening audience | 7 (14.6) |
| Fifth screening audience | 0 (0.0) |
| Theater staff | 1 (2.1) |
| Family member | 10 (20.8) |
| Friend | 2 (4.2) |
| Symptoms | |
| Asymptomatic | 10 (20.8) |
| Symptomatic | 38 (79.2) |
| Vaccination status | |
| Unvaccinated or first vaccination | 13 (27.1) |
| Second vaccination | 35 (72.9) |
| Place of exposure | |
| Movie theater | 36 (75.0) |
| House | 10 (20.8) |
| Elementary school | 1 (2.1) |
| Othera) | 1 (2.1) |
| Characteristic | Total | Confirmed cases | Attack rate | Crude risk ratioa) | Adjusted risk ratiob) |
|---|---|---|---|---|---|
| Total | 80 (100.0)c) | 35 (100.0) | 43.8 (33.4–54.7) | ||
| Sex | |||||
| Male | 51 (63.8) | 22 (62.9) | 43.1 (30.5–56.7) | Ref. | Ref. |
| Female | 29 (36.3) | 13 (37.1) | 44.8 (28.4–62.5) | 1.1 (0.42–2.69) | 1.7 (0.54–5.60) |
| Age (y) | |||||
| ≤18 | 15 (18.8) | 8 (22.9) | 53.3 (30.1–75.2) | Ref. | Ref. |
| >19 | 65 (81.3) | 27 (77.1) | 41.5 (30.4–53.7) | 0.6 (0.20–1.93) | 1.0 (0.17–7.13) |
| Screening attended | |||||
| Third | 33 (41.3) | 28 (80.0) | 84.8 (69.1–93.3) | 24.0 (7.4–93.8) | NA |
| Fourth | 37 (46.3) | 7 (20.0) | 18.9 (9.5–34.2) | Ref. | Ref. |
| Fifth | 10 (12.5) | 0 (0.0) | 0.0 (0.0–27.8) | NA | NA |
| Food consumption | |||||
| No | 74 (92.5) | 29 (82.9) | 39.2 (28.9–50.6) | Ref. | Ref. |
| Yes | 6 (7.5) | 6 (17.1) | 100.0 (61.0–100.0) | NA | NA |
| Vaccination status | |||||
| Unvaccinated or first vaccination | 10 (12.5) | 7 (20.0) | 70.0 (39.7–89.2) | Ref. | Ref. |
| Second vaccination | 70 (87.5) | 28 (80.0) | 40.0 (29.3–51.7) | 0.4 (0.09–1.42) | 0.2 (0.02–1.26) |
| Proximity of exposure | |||||
| Casual contact | 61 (76.3) | 19 (54.3) | 31.1 (20.9–43.6) | Ref. | Ref. |
| Close contact | 19 (23.8) | 16 (45.7) | 84.2 (62.4–94.5) | 11.8 (3.44–55.17) | 15.9 (4.37–78.39) |
Data are presented as n (%) or % (95% confidence interval).
Ref., reference; NA, not available.
a) The univariable model was adjusted for matching factors, including sex, age, screening attended, food consumption, vaccination status, and proximity of exposure.
b) The multivariable model was adjusted for all variables incorporated within it, with the exceptions of screening attended and food consumption.
c) A total of 12 people were excluded from the study: 1 individual in the 3rd screening, 5 in the 4th screening, and 6 in the 5th screening.
- 1. Prather KA, Marr LC, Schooley RT, et al. Airborne transmission of SARS-CoV-2. Science 2020;370:303−4.Article
- 2. World Health Organization (WHO). Transmission of SARS-CoV-2: implications for infection prevention precautions: scientific brief, 09 July 2020 [Internet]. WHO; 2020 [cited 2023 Mar 20]. Available from: https://iris.who.int/handle/10665/333114.
- 3. Qian M, Jiang J. COVID-19 and social distancing. Z Gesundh Wiss 2022;30:259−61.ArticlePubMedPMCPDF
- 4. Courtemanche C, Garuccio J, Le A, et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood) 2020;39:1237−46.ArticlePubMed
- 5. Johnson CY, Sun LH, Freedman A. Social distancing could buy U.S. valuable time against coronavirus. The Washington Post [Internet]. 2020 Mar 10 [cited 2023 Mar 20]. https://www.washingtonpost.com/health/2020/03/10/social-distancing-coronavirus/.
- 6. Greenhalgh T, Jimenez JL, Prather KA, et al. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet 2021;397:1603−5.ArticlePubMedPMC
- 7. Kim EY, Park SY, Lee SY, et al. Results of epidemiological investigation of the coronavirus disease-19 epidemic that occurred in fitness centers. Public Health Wkly Rep 2021;14:1215−24. Korean.
- 8. Lee SY, Park SY, Kim EY, et al. Quantitative analysis of a coronavirus disease 2019 (COVID-19) call center outbreak, South Korea. Public Health Wkly Rep 2021;14:1225−36. Korean.
- 9. Korea Disease Control and Prevention Agency (KDCA). Preparation of “Wise Ventilation Guidelines” to prevent respiratory infectious diseases [Internet]. KDCA; 2021 [cited 2023 Mar 20]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=717354&cg_code=&act=view&nPage=1. Korean.
- 10. Korea Disease and Prevention Agency (KDCA). Guidelines for wise ventilation to prevent the spread of COVID-19 [Internet]. KDCA; 2023 [cited 2023 Mar 20]. Available from: https://www.kdca.go.kr/gallery.es?mid=a20503010000&bid=0002&act=view&list_no=145992. Korean.
- 11. World Health Organization (WHO). Coronavirus disease (COVID-19): how is it transmitted? [Internet]. WHO; 2021 [cited 2023 Mar 20]. Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted?fbclid=IwAR1vAg10CSquSMGj6CvC7SCa0xPuw_N3TcyavlJ0ua5Qdc9CpKhImBPBdUE.
- 12. National Center for Immunization and Respiratory Diseases, Division of Viral Diseases. Scientific brief: SARS-CoV-2 transmission [Internet]. Centers for Disease Control and Prevention; 2021 [cited 2023 Mar 20]. Available from: https://stacks.cdc.gov/view/cdc/105949.
- 13. Ministry of Health and Welfare. Phased daily recovery implementation plan [Internet]. Ministry of Health and Welfare; 2021 [cited 2023 Mar 20]. Available from: https://www.mohw.go.kr/board.es?mid=a10503010100&bid=0027&cg_code=#share. Korean.
- 14. Korea Disease Control and Prevention Agency (KDCA). COVID-19 response guidelines for local government [Internet]. 10th ed. KDCA; 2021 [cited 2022 Apr 1]. Available from: http://www.cncidc.or.kr/user/nd68273.do?View&dmlType=&keyword=&menuCode=krsite&page=3&pageSC=&pageSO=&dmlType=&boardNo=1594&pageSV= Korean. Korean.
- 15. Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control 2016;44(9 Suppl):S102−8.ArticlePubMedPMC
- 16. Infectious disease control and prevention Act, Act No. 13392 (July 6, 2015) [Internet]. Korean Law Information Center; 2016 [cited 2023 Mar 20]. Available from: https://www.law.go.kr/LSW/lsInfoP.do?lsiSeq=172762&viewCls=engLsInfoR&urlMode=engLsInfoR&chrClsCd=010203#0000. Korean.
- 17. Kwon KS, Park JI, Park YJ, et al. Evidence of long-distance droplet transmission of SARS-CoV-2 by direct air flow in a restaurant in Korea. J Korean Med Sci 2020;35:e415.ArticlePubMedPMCPDF
- 18. Katoh K, Rozewicki J, Yamada KD. MAFFT online service: multiple sequence alignment, interactive sequence choice and visualization. Brief Bioinform 2019;20:1160−6.ArticlePubMedPMCPDF
- 19. Price MN, Dehal PS, Arkin AP. FastTree 2: approximately maximum-likelihood trees for large alignments. PLoS One 2010;5:e9490.ArticlePubMedPMC
- 20. European Centre for Disease Prevention and Control. Risk assessment guidelines for infectious diseases transmitted on aircraft (RAGIDA): tuberculosis [Internet]. European Centre for Disease Prevention and Control; 2014 [cited 2023 Mar 20]. Available from: https://www.ecdc.europa.eu/en/publications-data/risk-assessment-guidelines-infectious-diseases-transmitted-aircraft-ragida-0.
- 21. World Health Organization (WHO). Tuberculosis and air travel: guidelines for prevention and control [Internet]. 3rd ed. WHO; 2008 [cited 2023 Mar 20]. Available from: https://www.who.int/publications-detail-redirect/9789241547505.
- 22. Kim JK, Lee NJ, Kim HM, et al. Analysis of respiratory specimens from confirmed cases of the Delta variant and the previous epidemic lineage. Public Health Wkly Rep 2021;14:2494−5. Korean.
- 23. Grant R, Charmet T, Schaeffer L, et al. Impact of SARS-CoV-2 Delta variant on incubation, transmission settings and vaccine effectiveness: results from a nationwide case-control study in France. Lancet Reg Health Eur 2022;13:100278. ArticlePubMedPMC
- 24. Li B, Deng A, Li K, et al. Viral infection and transmission in a large, well-traced outbreak caused by the SARS-CoV-2 Delta variant. Nat Commun 2022;13:460. ArticlePubMedPMCPDF
- 25. Kang M, Xin H, Yuan J, et al. Transmission dynamics and epidemiological characteristics of SARS-CoV-2 Delta variant infections in Guangdong, China, May to June 2021. Euro Surveill 2022;27:2100815. ArticlePubMedPMC
- 26. Liu Y, Rocklov J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J Travel Med 2021;28:taab124. ArticlePubMedPMCPDF
- 27. Oliver S. Framework for booster doses of COVID-19 vaccines [Internet]. Centers for Disease Control and Prevention; 2021 [cited 2023 Mar 27]. Available from: https://stacks.cdc.gov/view/cdc/109498.
- 28. Li Y, Leung GM, Tang JW, et al. Role of ventilation in airborne transmission of infectious agents in the built environment: a multidisciplinary systematic review. Indoor Air 2007;17:2−18.ArticlePubMed
- 29. National Center for Immunization and Respiratory Diseases, Division of Viral Diseases. Science brief: SARS-CoV-2 and surface (fomite) transmission for indoor community environments [Internet]. Centers for Disease Control and Prevention; 2021 [cited 2023 Mar 20]. Available from: https://stacks.cdc.gov/view/cdc/104762.
References
Figure & Data
References
Citations

- Figure
- Related articles
-
- Effect of Paxlovid in COVID-19 treatment during the periods of SARS-CoV-2 Omicron BA.5 and BN.1 subvariant dominance in the Republic of Korea: a retrospective cohort study
- Developing a national surveillance system for stroke and acute myocardial infarction using claims data in the Republic of Korea: a retrospective study
- Risk factors for transmission in a COVID-19 cluster infection in a high school in the Republic of Korea


 Cite
Cite