Search
- Page Path
- HOME > Search
Original Article
- Drug resistance and the genotypic characteristics of rpoB and katG in rifampicin- and/or isoniazid-resistant Mycobacterium tuberculosis isolates in central Vietnam
- Thi Binh Nguyen Nguyen, Thi Kieu Diem Nguyen, Van Hue Trương, Thi Tuyet Ngoc Tran, van Bao Thang Phan, Thi Tuyen Nguyen, Hoang Bach Nguyen, Viet Quynh Tram Ngo, Van Tuan Mai, Paola Molicotti
- Osong Public Health Res Perspect. 2023;14(5):347-355. Published online October 18, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0124
- 1,198 View
- 82 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 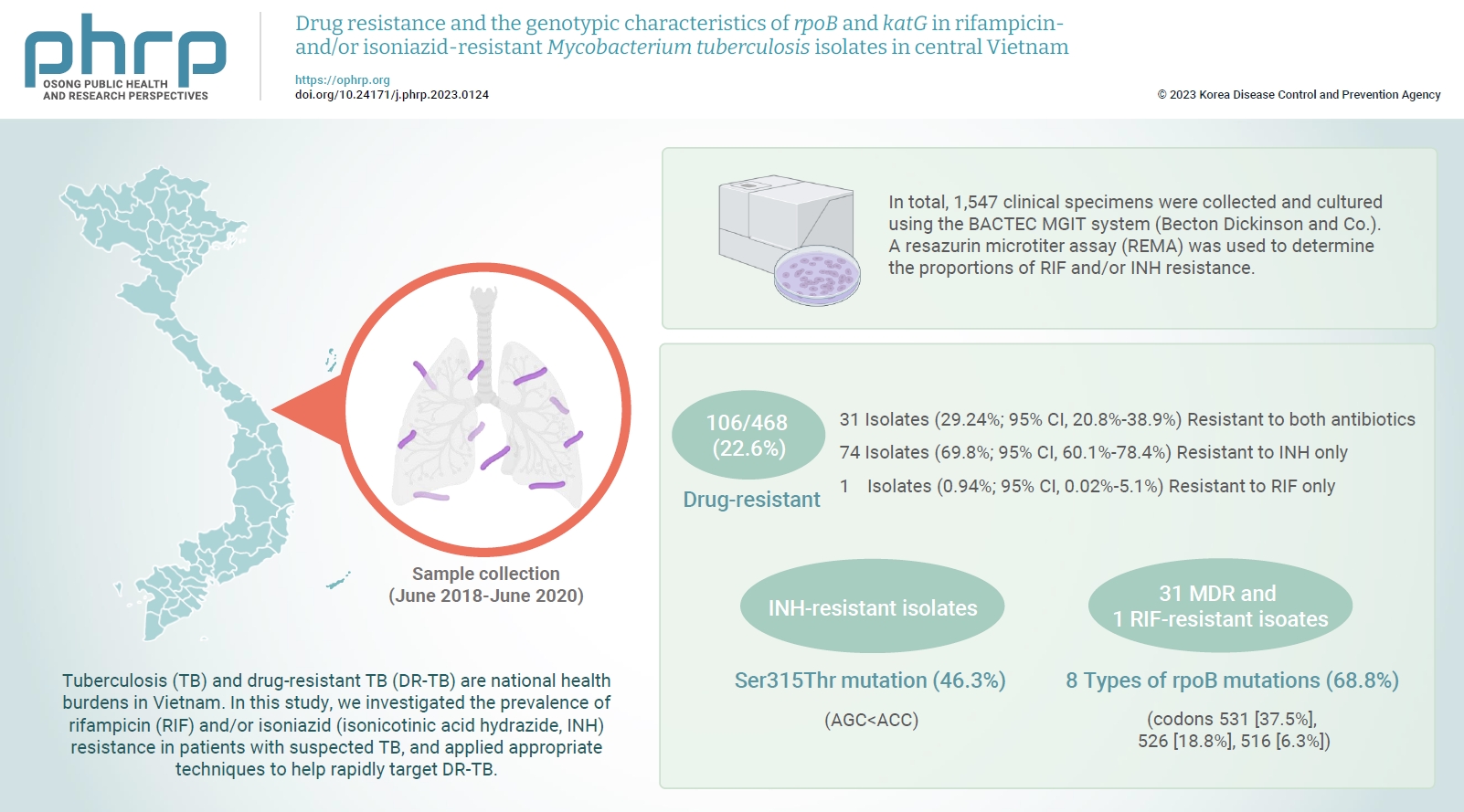
- Objectives
Tuberculosis (TB) and drug-resistant TB (DR-TB) are national health burdens in Vietnam. In this study, we investigated the prevalence of rifampicin (RIF) and/or isoniazid (isonicotinic acid hydrazide, INH) resistance in patients with suspected TB, and applied appropriate techniques to help rapidly target DR-TB. Methods: In total, 1,547 clinical specimens were collected and cultured using the BACTEC MGIT system (Becton Dickinson and Co.). A resazurin microtiter assay (REMA) was used to determine the proportions of RIF and/or INH resistance. A real-time polymerase chain reaction panel with TaqMan probes was employed to identify the mutations of rpoB and katG associated with DR-TB in clinical isolates. Genotyping of the identified mutations was also performed. Results: A total of 468 Mycobacterium tuberculosis isolates were identified using the REMA. Of these isolates, 106 (22.6%) were found to be resistant to 1 or both antibiotics. Of the resistant isolates, 74 isolates (69.8%) were resistant to isoniazid (INH) only, while 1 isolate (0.94%) was resistant to RIF only. Notably, 31 isolates (29.24%) were resistant to both antibiotics. Of the 41 phenotypically INH-resistant isolates, 19 (46.3%) had the Ser315Thr mutation. There were 8 different rpoB mutations in 22 (68.8%) of the RIF-resistant isolates. The most frequently detected mutations were at codons 531 (37.5%), 526 (18.8%), and 516 (6.3%). Conclusion: To help prevent new cases of DR-TB in Vietnam, it is crucial to gain a comprehensive understanding of the genotypic DR-TB isolates.


 First
First Prev
Prev


