Search
- Page Path
- HOME > Search
Original Articles
- A spatial analysis of the association between social vulnerability and the cumulative number of confirmed deaths from COVID-19 in United States counties through November 14, 2020
- Baksun Sung
- Osong Public Health Res Perspect. 2021;12(3):149-157. Published online June 2, 2021
- DOI: https://doi.org/10.24171/j.phrp.2020.0372
- 6,659 View
- 150 Download
- 4 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 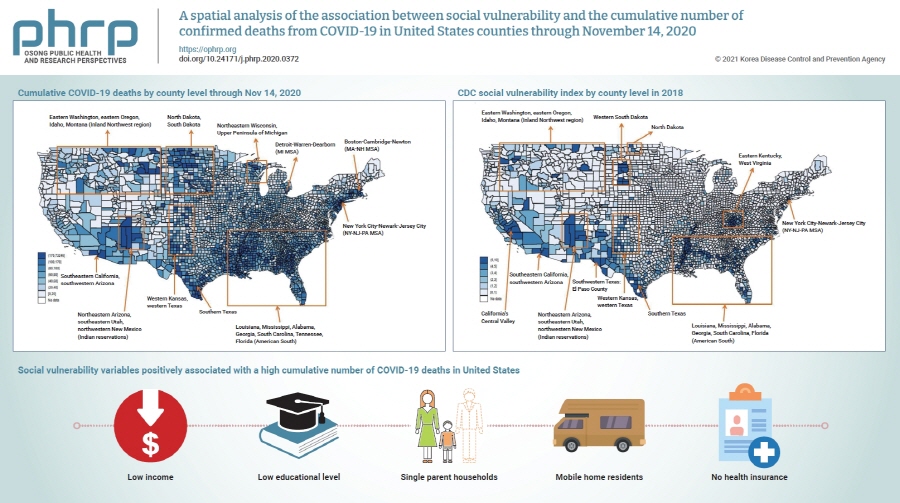
- Objectives
Coronavirus disease 2019 (COVID-19) is classified as a natural hazard, and social vulnerability describes the susceptibility of social groups to potential damages from natural hazards. Therefore, the objective of this study was to examine the association between social vulnerability and the cumulative number of confirmed COVID-19 deaths (per 100,000) in 3,141 United States counties.
Methods
The cumulative number of COVID-19 deaths was obtained from USA Facts. Variables related to social vulnerability were obtained from the Centers for Disease Control and Prevention Social Vulnerability Index and the 2018 5-Year American Community Survey. Data were analyzed using spatial autoregression models.
Results
Lowest income and educational level, as well as high proportions of single parent households, mobile home residents, and people without health insurance were positively associated with a high cumulative number of COVID-19 deaths.
Conclusion
In conclusion, there are regional differences in the cumulative number of COVID-19 deaths in United States counties, which are affected by various social vulnerabilities. Hence, these findings underscore the need to take social vulnerability into account when planning interventions to reduce COVID-19 deaths. -
Citations
Citations to this article as recorded by- Ecological comparison of six countries in two waves of COVID-19
Meiheng Liu, Leiyu Shi, Manfei Yang, Jun Jiao, Junyan Yang, Mengyuan Ma, Wanzhen Xie, Gang Sun
Frontiers in Public Health.2024;[Epub] CrossRef - Social vulnerability and COVID-19 in Maringá, Brazil
Matheus Pereira Libório, Oseias da Silva Martinuci, Patrícia Bernardes, Natália Cristina Alves Caetano Chav Krohling, Guilherme Castro, Henrique Leonardo Guerra, Eduardo Alcantara Ribeiro, Udelysses Janete Veltrini Fonzar, Ícaro da Costa Francisco
Spatial Information Research.2023; 31(1): 51. CrossRef - A county-level analysis of association between social vulnerability and COVID-19 cases in Khuzestan Province, Iran
Mahmoud Arvin, Shahram Bazrafkan, Parisa Beiki, Ayyoob Sharifi
International Journal of Disaster Risk Reduction.2023; 84: 103495. CrossRef - Global mapping of epidemic risk assessment toolkits: A scoping review for COVID-19 and future epidemics preparedness implications
Bach Xuan Tran, Long Hoang Nguyen, Linh Phuong Doan, Tham Thi Nguyen, Giang Thu Vu, Hoa Thi Do, Huong Thi Le, Carl A. Latkin, Cyrus S. H. Ho, Roger C. M. Ho, Md Nazirul Islam Sarker
PLOS ONE.2022; 17(9): e0272037. CrossRef - COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities
Victoria J McGowan, Clare Bambra
The Lancet Public Health.2022; 7(11): e966. CrossRef
- Ecological comparison of six countries in two waves of COVID-19
- Spatial Distribution Analysis of Scrub Typhus in Korea
- Hong Sung Jin, Chaeshin Chu, Dong Yeob Han
- Osong Public Health Res Perspect. 2013;4(1):4-15. Published online February 28, 2013
- DOI: https://doi.org/10.1016/j.phrp.2012.12.007
- 2,927 View
- 21 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objective:
This study analyzes the spatial distribution of scrub typhus in Korea.
Methods
A spatial distribution of Orientia tsutsugamushi occurrence using a geographic information system (GIS) is presented, and analyzed by means of spatial clustering and correlations.
Results
The provinces of Gangwon-do and Gyeongsangbuk-do show a low incidence throughout the year. Some districts have almost identical environmental conditions of scrub typhus incidence. The land use change of districts does not directly affect the incidence rate.
Conclusion
GIS analysis shows the spatial characteristics of scrub typhus. This research can be used to construct a spatial-temporal model to understand the epidemic tsutsugamushi. -
Citations
Citations to this article as recorded by- Emergence of “urban scrub typhus” during Monsoon season in an urban pocket and biodiversity hotspot of New Delhi, India
InamDanish Khan, Pradeep Bahal, Bhagwat Singh, Pallawi Priya, Rahul Pandey, Anuradha Makkar, AshokKumar Jindal
Journal of Marine Medical Society.2022; 24(2): 124. CrossRef - Scrub typhus and antibiotic-resistant Orientia tsutsugamushi
Chin-Te Lu, Lih-Shinn Wang, Po-Ren Hsueh
Expert Review of Anti-infective Therapy.2021; 19(12): 1519. CrossRef - Three‐year surveillance (2016–2018) of chigger mites vector for tsutsugamushi disease in the Hwaseong‐Si area of Gyeonggi‐Do, Republic of Korea
Hojong Jun, Seung Jegal, Myung‐Deok Kim‐Jeon, Jong Yul Roh, Wook‐Gyo Lee, Seo Hye Park, Seong Kyu Ahn, Jinyoung Lee, Young Woo Gong, Mun Ju Kwon, Young Yil Bahk, Tong‐Soo Kim
Entomological Research.2020; 50(2): 63. CrossRef - Surveillance of Chigger Mite Vectors for Tsutsugamushi Disease in the Hwaseong Area, Gyeonggi-do, Republic of Korea, 2015
Young Yil Bahk, Hojong Jun, Seo Hye Park, Haneul Jung, Seung Jegal, Myung-Deok Kim-Jeon, Jong Yul Roh, Wook-Gyo Lee, Seong Kyu Ahn, Jinyoung Lee, Kwangsig Joo, Young Woo Gong, Mun Ju Kwon, Tong-Soo Kim
The Korean Journal of Parasitology.2020; 58(3): 301. CrossRef - Scrub Typhus in a Tertiary Care Hospital in Visakhapatnam
Vandana Shankar, Mandarapu Roopalatha, Sudha Lakshmi
Journal of Evolution of Medical and Dental Science.2019; 8(40): 3028. CrossRef - Imported scrub typhus: first case in South America and review of the literature
Thomas Weitzel, Mabel Aylwin, Constanza Martínez-Valdebenito, Ju Jiang, Jose Manuel Munita, Luis Thompson, Katia Abarca, Allen L. Richards
Tropical Diseases, Travel Medicine and Vaccines.2018;[Epub] CrossRef - Geographical Distribution and Seasonal Indices of Chigger Mites on Small Mammals Collected on the East Coast of the Republic of Korea
Gab-Man Park, Ho-Sung Shin
Journal of Parasitology.2016; 102(2): 193. CrossRef - Severe Fever with Thrombocytopenia Syndrome in South Korea, 2013-2015
Seong Jin Choi, Sang-Won Park, In-Gyu Bae, Sung-Han Kim, Seong Yeol Ryu, Hyun Ah Kim, Hee-Chang Jang, Jian Hur, Jae-Bum Jun, Younghee Jung, Hyun-Ha Chang, Young Keun Kim, Jongyoun Yi, Kye-Hyung Kim, Jeong-Hwan Hwang, Yeon-Sook Kim, Hye Won Jeong, Kyoung-H
PLOS Neglected Tropical Diseases.2016; 10(12): e0005264. CrossRef - Urbanization of Scrub Typhus Disease in South Korea
Sang-Won Park, Na-Young Ha, Boyeong Ryu, Ji Hwan Bang, Hoyeon Song, Yuri Kim, Gwanghun Kim, Myoung-don Oh, Nam-Hyuk Cho, Jong-koo Lee, Darren J. Gray
PLOS Neglected Tropical Diseases.2015; 9(5): e0003814. CrossRef - Seroconversions to Rickettsiae in US Military Personnel in South Korea
Ju Jiang, Todd E. Myers, Patrick J. Rozmajzl, Paul C.F. Graf, Jean-Paul Chretien, Joel C. Gaydos, Allen L. Richards
Emerging Infectious Diseases.2015; 21(6): 1073. CrossRef - Scrub Typhus Incidence Modeling with Meteorological Factors in South Korea
Jaewon Kwak, Soojun Kim, Gilho Kim, Vijay Singh, Seungjin Hong, Hung Kim
International Journal of Environmental Research an.2015; 12(7): 7254. CrossRef - Predictors of scrub typhus: a study from a tertiary care center
Vijay Kumar Agarwal, Gangireddy Krishna Mohan Reddy, Malla Rama Krishna, Garalapati Ramareddy, Prusti Saroj, Venkata Chandra Sekher Srinivasarao Bandaru
Asian Pacific Journal of Tropical Disease.2014; 4: S666. CrossRef - The Geographical and Economical Impact of Scrub Typus, the Fastest-growing Vector-borne Disease in Korea
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2013; 4(1): 1. CrossRef
- Emergence of “urban scrub typhus” during Monsoon season in an urban pocket and biodiversity hotspot of New Delhi, India



 First
First Prev
Prev


