Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(6); 2023 > Article
-
Original Article
Characteristics and related factors of waterborne and foodborne infectious disease outbreaks before and after the onset of the COVID-19 pandemic (2017–2021) in the Republic of Korea: a descriptive study -
Eunkyoung Kim
 , Bryan Inho Kim
, Bryan Inho Kim
-
Osong Public Health and Research Perspectives 2023;14(6):483-493.
DOI: https://doi.org/10.24171/j.phrp.2023.0221
Published online: December 14, 2023
Division of Infectious Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Bryan Inho Kim Division of Infectious Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, 200 OsongSaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: globalepi@korea.kr
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 796 Views
- 43 Download
Abstract
-
Objectives
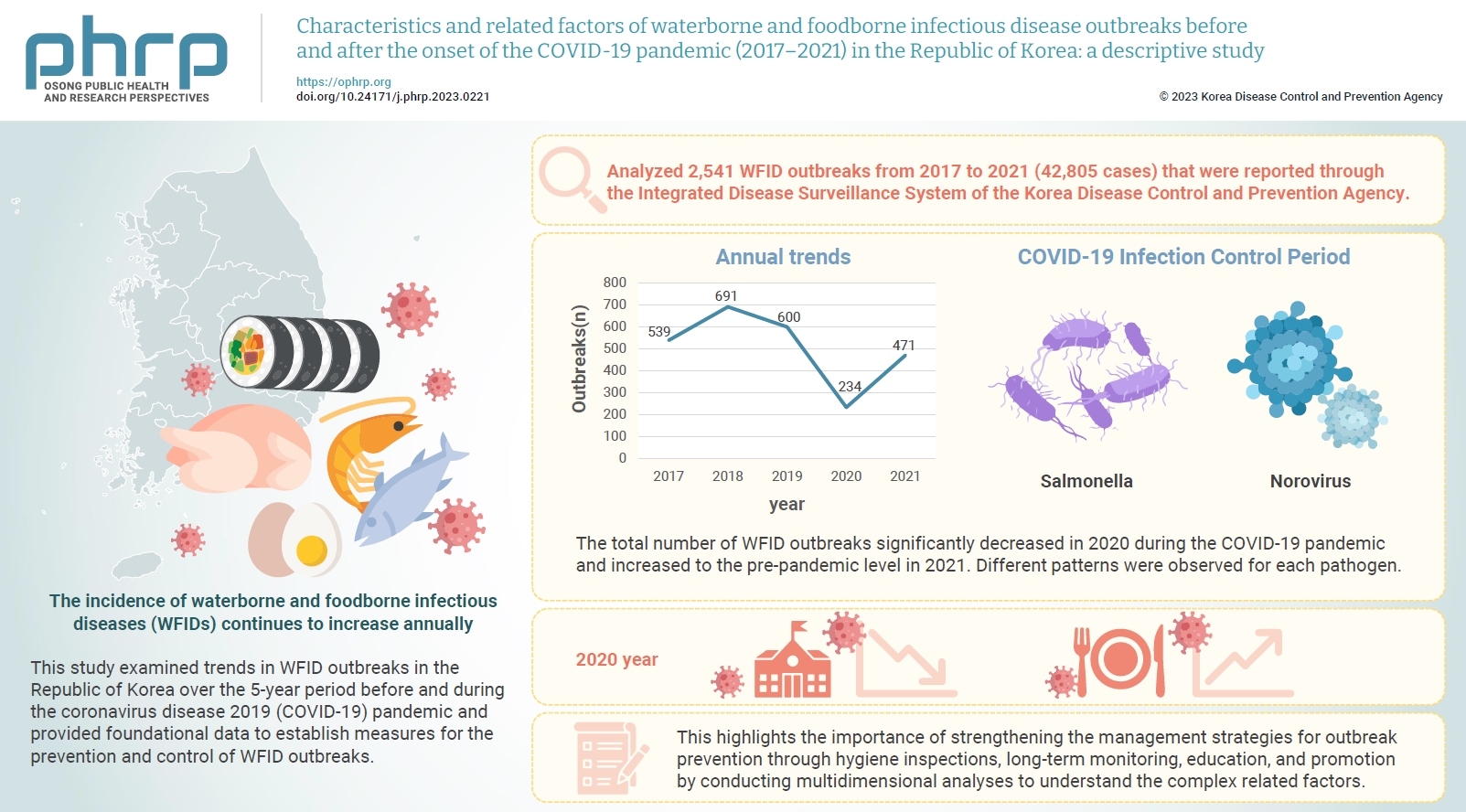
- The incidence of waterborne and foodborne infectious diseases (WFIDs) continues to increase annually, attracting significant global attention. This study examined trends in WFID outbreaks in the Republic of Korea over the 5-year period before and during the coronavirus disease 2019 (COVID-19) pandemic and provided foundational data to establish measures for the prevention and control of WFID outbreaks.
-
Methods
- We analyzed 2,541 WFID outbreaks from 2017 to 2021 (42,805 cases) that were reported through the Integrated Disease Surveillance System of the Korea Disease Control and Prevention Agency. Outbreaks were defined as the occurrence of gastrointestinal symptoms in ≥2 individuals within a group with temporal and regional epidemiological associations. The related factors associated with WFID outbreaks during the observation period were statistically analyzed.
-
Results
- The total number of WFID outbreaks significantly decreased in 2020 during the COVID-19 pandemic and increased to the pre-pandemic level in 2021. Different patterns were observed for each pathogen. The incidence of Salmonella outbreaks more than doubled, while norovirus outbreaks decreased significantly.
-
Conclusion
- WFID outbreaks in the Republic of Korea showed different patterns before and during the COVID-19 pandemic, influenced by infection control measures and changes in dietary consumption patterns. Outbreaks of some diseases increased, but the infection control measures applied during the pandemic resulted in a significant decrease in the overall number of WFID outbreaks. This highlights the importance of strengthening the management strategies for outbreak prevention through hygiene inspections, long-term monitoring, education, and promotion by conducting multidimensional analyses to understand the complex related factors.
- Waterborne and foodborne infectious diseases (WFIDs) are caused by pathogenic bacteria and viruses. Symptoms such as diarrhea, vomiting, fever, and abdominal pain are the typical manifestations of WFIDs. The increasing incidence of WFIDs is a significant global phenomenon. In the Republic of Korea, 400 to 600 WFID cases were reported annually, with an upward trend due to factors such as dining out and institutional food service [1-3].
- In 2017, WFID outbreaks involved numerous cases of shigellosis, typhoid fever, and rotavirus. Recent increases in norovirus and Salmonella, as well as outbreaks of enterohemorrhagic Escherichia coli (EHEC) and hepatitis E, have also been reported. In particular, the changes in WFIDs during pandemics, such as coronavirus disease 2019 (COVID-19), are noteworthy.
- On March 11, 2020, COVID-19 was declared a pandemic by the World Health Organization. Subsequently, the nationwide implementation of nonpharmaceutical interventions in the Republic of Korea significantly reduced the weekly positivity rates for respiratory viral infections in 2020. Infection control measures, including personal hygiene and social distancing, may have also reduced the positivity rates for non-respiratory infectious diseases [4–7].
- A comparative study investigating trends in the occurrence of gastrointestinal (GI) infections in the United States (US) and the Republic of Korea before and during the COVID-19 pandemic revealed a notable decline in both bacterial and viral GI infections in the US. In the Republic of Korea, only the decrease in viral GI infections was statistically significant [8].
- The occurrence of WFID outbreaks has demonstrated diverse trends for individual pathogens, influenced by seasonal variations and the prolonged impact of the COVID-19 pandemic. This study analyzed and assessed temporal (2017–2021) and regional (17 municipalities and provinces in the Republic of Korea) trends in WFID occurrence, and compared the epidemiological characteristics of WFID outbreaks before and during the pandemic.
Introduction
- Study Population
- A total of 2,541 reported outbreaks and 42,805 cases of WFIDs, reported from January 2017 to December 2021 through the Integrated Disease Surveillance System of the Korea Disease Control and Prevention Agency (KDCA), were analyzed. Data were obtained from 17 administrative regions nationwide and were classified according to the addresses of the reporting institutions.
- The types of WFIDs included Class II (cholera, typhoid and paratyphoid fever, bacterial dysentery, EHEC, and hepatitis A and E), Class III (Vibrio sepsis), and Class IV (20 other GI infections) infectious diseases. The related pathogens included 17 bacterial species (including enteroadherent E. coli), 6 viral species, 4 protozoal species, and Kudoa septempunctata. Class II and Class III infectious diseases were managed under the mandatory surveillance system, and Class IV infectious diseases (GI infections) were managed under the sentinel surveillance system implemented at 208 facilities nationwide [2].
- The reported cases of WFIDs included in this study were cases in which the causative pathogens were confirmed through laboratory analysis of human samples. An outbreak was defined as a concurrent infection in ≥2 individuals who experienced symptoms of an enteric infection such as diarrhea and vomiting after consuming the same food. According to the operational criteria of the epidemiological investigation team, outbreaks with ≥7 and 2 to 6 related cases were classified as large- and small-scale outbreaks, respectively.
- Data Analysis
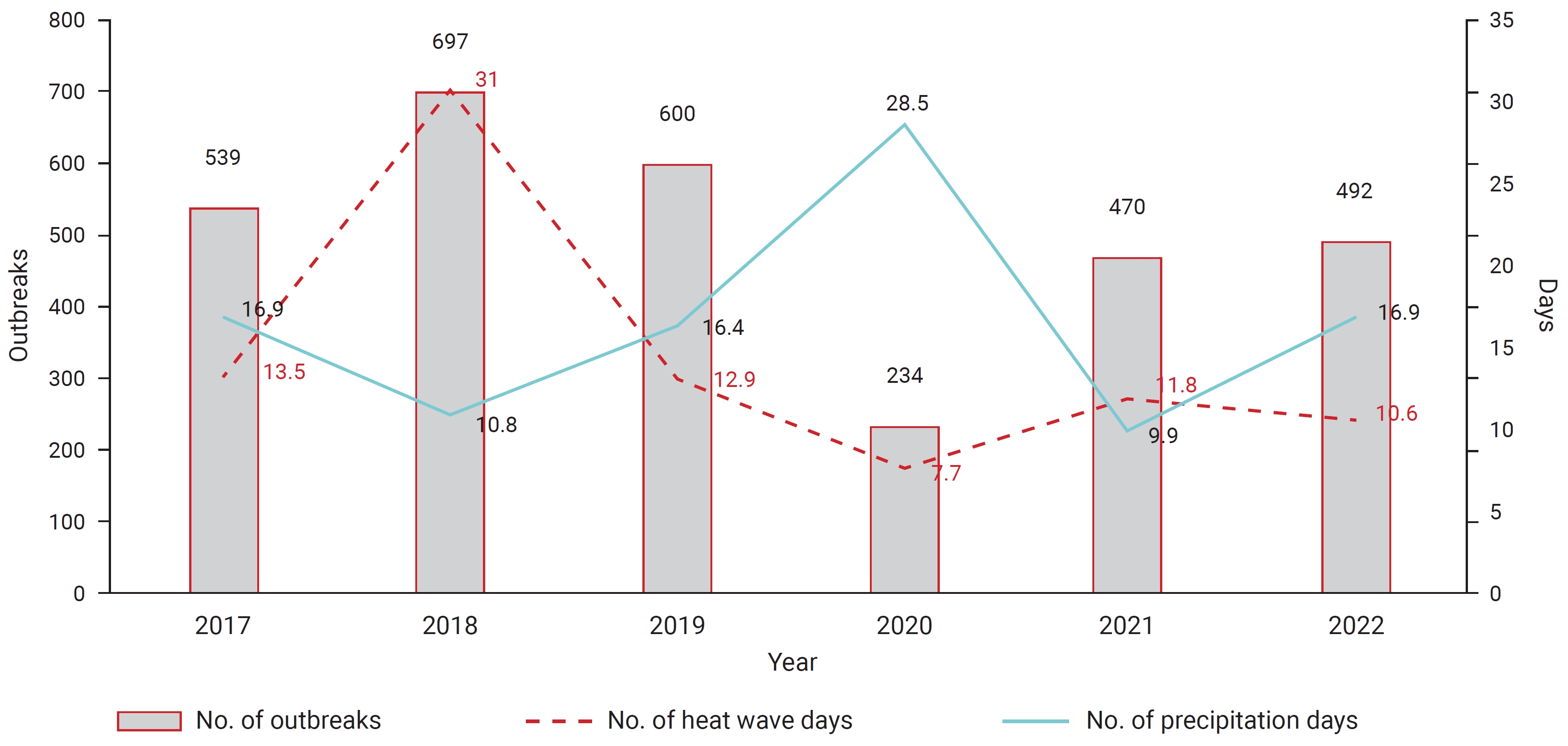
- To describe the general characteristics of WFID outbreaks and to provide temporal and regional occurrence trends, data analysis was performed using Excel ver. 2016 (Microsoft Corp.). The WFID incidence rate per 100,000 population in each region was calculated to examine the population-standardized rates and regional variations, using the mid-year (July 1) population data from the resident population registry released by the Ministry of the Interior and Safety. To calculate WFID incidence rates, the annual population data from 2017 to 2021, as categorized by year, age group, region, and district, were used as the denominator, and the number of WFID cases in the corresponding category was used as the numerator. Meteorological data for each year were obtained from the weather data portal service provided by the Korea Meteorological Administration [9]. We analyzed trends in WFID outbreaks according to meteorological factors such as the number of days with heat waves and days with precipitation from 2017 to 2021.
- IRB/IACUC Approval
- This study was granted an exemption from review by the Institutional Review Board of the KDCA (IRB No: 2023-03-01-PE-A).
Materials and Methods
- Outbreak Status
- The number of WFID outbreaks peaked at 600 to 700 in 2018–2019. Following the implementation of social distancing measures in February 2020 due to the COVID-19 pandemic, the number of outbreaks sharply decreased to approximately 200. Since 2021, the number of outbreaks has rebounded to the previous average level.
- While WFID outbreaks decreased overall because of the COVID-19 infection control measures, different patterns were observed for specific pathogens. Among bacterial infections, the incidence rate of salmonellosis more than doubled. Among viral infections, the incidence rate of norovirus outbreaks decreased significantly.
- Salmonellosis outbreaks occurred at or above the average level. In 2020, salmonellosis outbreaks accounted for 8.5% of all WFID outbreaks, which was the highest proportion during the observation period.
- On average, salmonellosis outbreaks accounted for 4.2% of all WFID outbreaks during the observation period, with a consistent proportion of roughly 3% to 4% each year and a trend toward a high number of cases per outbreak. Notable outbreaks of Salmonella included the “chocolate cake,” “gimbap restaurant,” and “cold noodle restaurant” outbreaks in 2018 and 2021. A continued increase was expected with the increase in outdoor activities related to seasonal factors (summer), the relaxation of infection control measures, and the increased use of recreational facilities during the vacation season.
- The number of norovirus outbreaks decreased significantly to 51 in 2020, half the pre-pandemic levels. However, norovirus still accounted for 21.8% of all WFID outbreaks, and this proportion remained at the pre-pandemic level. During the observation period, the average number of norovirus outbreaks accounted for 31.9% of all WFID outbreaks, ranging between 20% and 30% each year. Notable norovirus outbreaks include the PyeongChang Olympics outbreak in 2018.
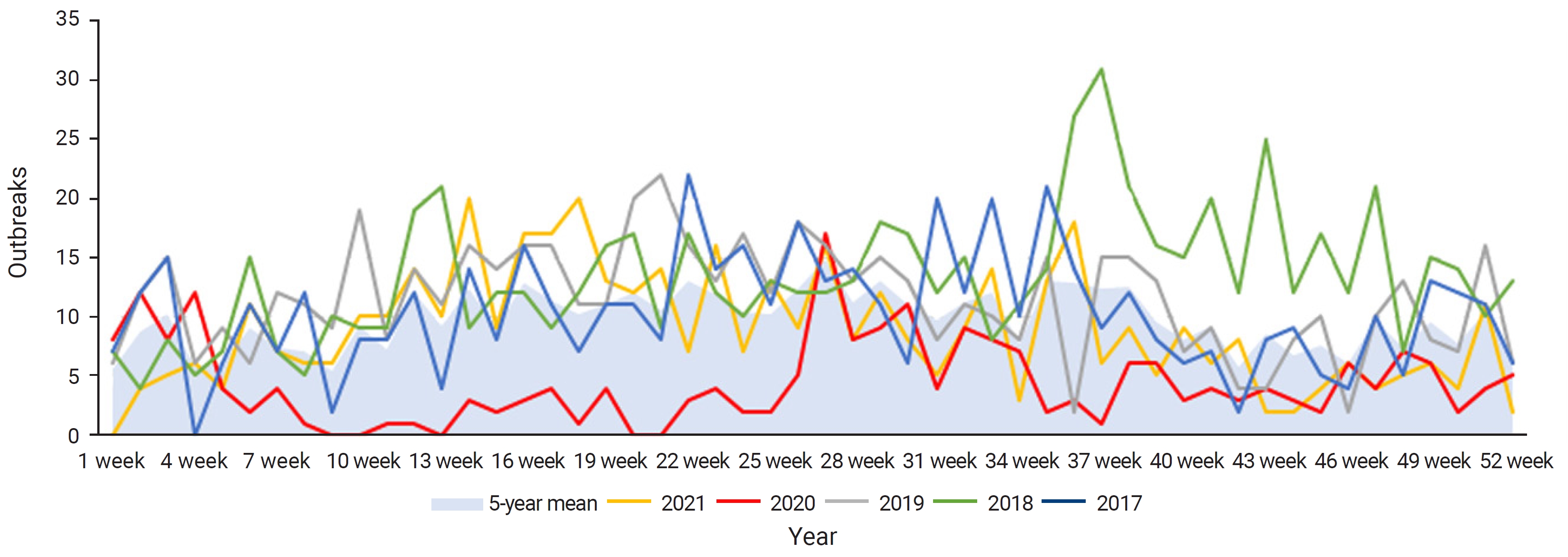
- During the observation period, WFID outbreaks mainly occurred between May and September of each year. In 2018, an earlier increase in the number of outbreaks than seen in the average year was observed, starting in early spring and continuing into winter. In 2020, a significant decrease in monthly outbreaks, compared with the average level, was observed (Figure 1).
- Among the bacterial infections investigated, the average monthly number of salmonellosis outbreaks was 1.8, with a seasonal concentration of outbreaks during the summer (June to October). The highest number of salmonellosis outbreaks occurred in October 2017, September 2018, August 2019, August 2021, and May 2022; these also demonstrated a pattern for earlier onset over the same 5 years. In 2022, the cumulative number of salmonellosis outbreaks reached 40, approximately 2.5 times higher than the average level. This may be attributed to the relaxation of COVID-19 infection control measures and the increase in outdoor activities.
- In the analysis of viral infections by month during the observation period, norovirus outbreaks predominantly occurred in early spring (January to April) and in winter (November and December). In 2020, a notable decrease in monthly outbreaks compared to a typical year was observed (Table 1).
- During the observation period of this study, the highest incidence of WFID outbreaks nationwide was recorded in 2018, with 25.1 cases per 100,000 population. The regions with the highest incidence rates, in descending order, were Sejong (58.6 cases), Gyeongsangbuk-do (51.0 cases), Seoul (36.8 cases), Jeju (34.2 cases), and Gangwon and Chungcheongnam-do (33 cases each). Conversely, Daejeon (3.2 cases), Gwangju (4.4 cases), and Ulsan (9.8 cases) had the lowest incidence rates. In 2020, the incidence rates per 100,000 population decreased to <10 cases in most regions, with a national average of 6.4 cases, which was the lowest during the observation period. Seoul and Jeju had the lowest and highest incidence rates of 2.7 and 48.8 cases, respectively (Table 2).
- During the observation period, norovirus was the most prevalent causative pathogen of WFID outbreaks, followed by Salmonella and Campylobacter. In 2020, norovirus outbreaks substantially decreased (51 cases), while the number of Salmonella and Campylobacter outbreaks remained constant or increased when compared with a typical year (Table 3).
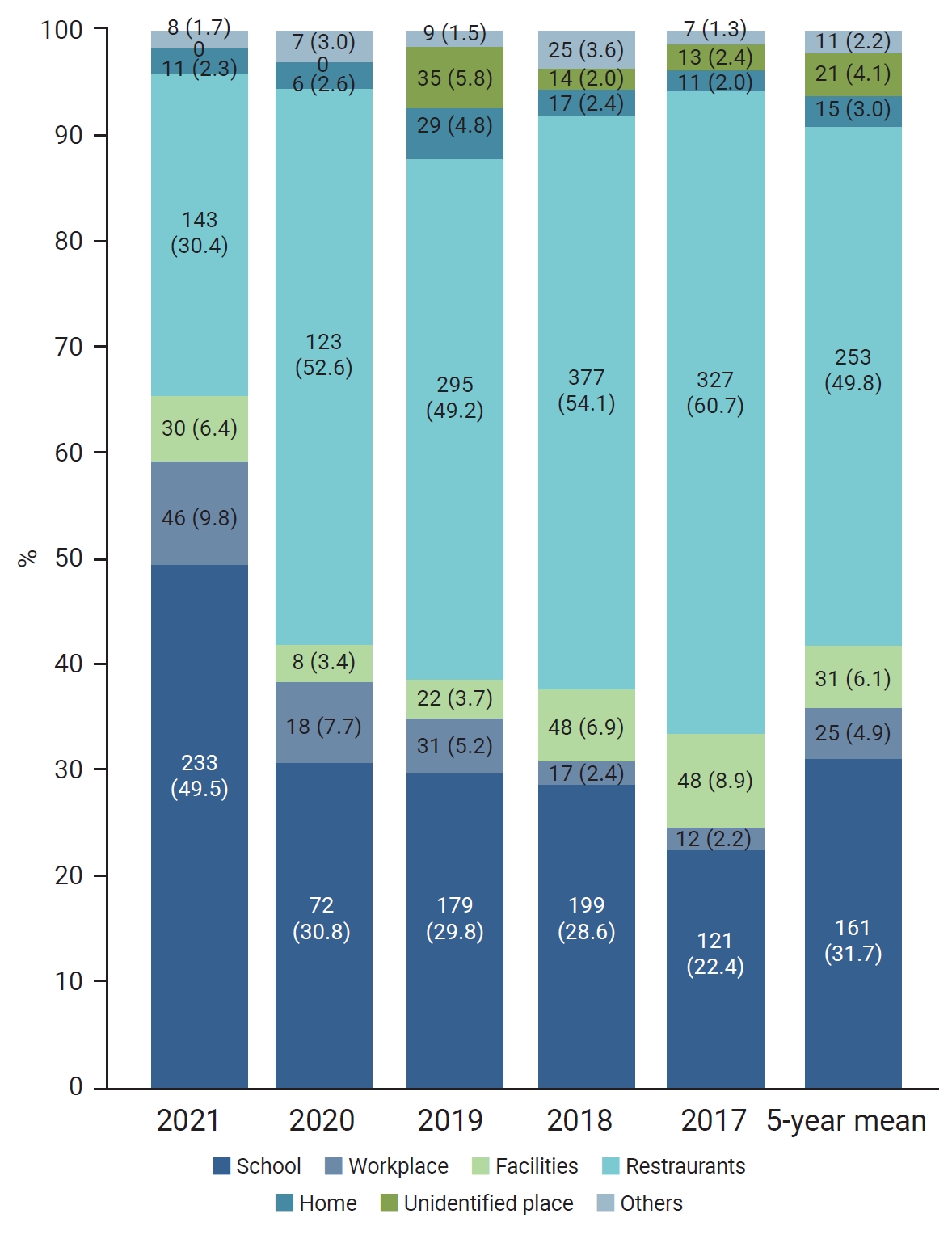
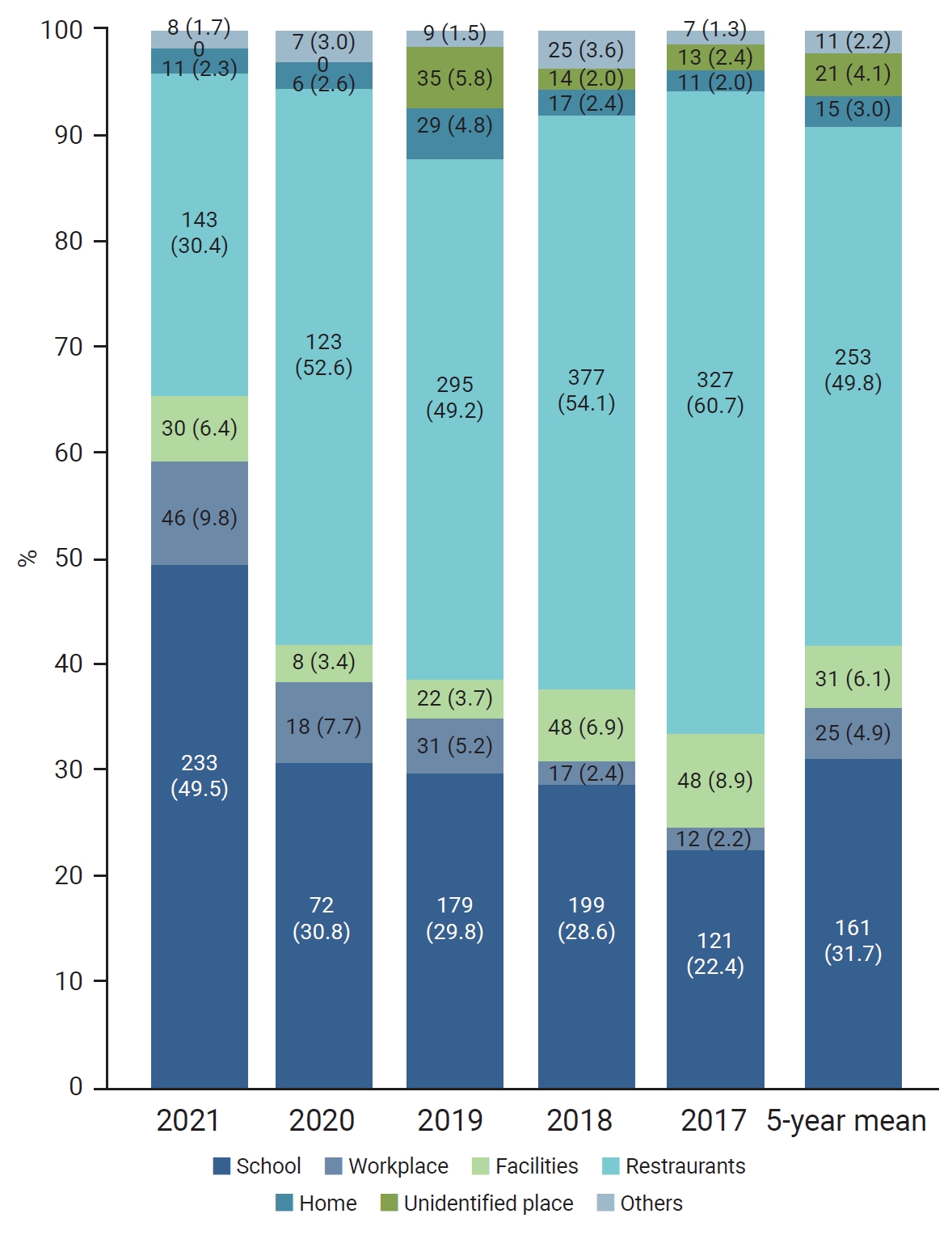
- During the observation period, WFID outbreaks occurred most frequently in restaurants (253 cases, 49.8%), followed by schools (including kindergartens and daycare centers; 161 cases, 31.7%) (Figure 2). While outbreaks in restaurants remained constant at 200 to 300 cases (50%–60%) per year, the number of cases significantly decreased to 123 in 2020.
- When confirmed COVID-19 cases were detected within a facility, the operation of the institution’s cafeteria was temporarily suspended, and packed meals were delivered by external vendors or food delivery services. This measure led to an increase in WFID outbreaks. Unlicensed packaged meal providers were identified through hygiene inspections.
- The average 5-year incidence of school-related WFID outbreaks was 163 cases, which decreased significantly to 72 cases in 2020. In 2021, school-related outbreaks outnumbered restaurant-related outbreaks. Among the school-related outbreaks in 2021, the number of cases in daycare centers nearly tripled compared with the 5-year average, while the number of cases in primary, middle, and high schools declined.
- Outbreaks in workplaces and facilities decreased in 2020 and subsequently increased. School-related norovirus outbreaks displayed a seasonal pattern, with a higher concentration in the spring (March/April) and late autumn/early winter (November/December) semesters.
- Before COVID-19, approximately 60% of outbreaks were small-scale. In 2020, the proportion of small-scale group outbreaks increased to 64.1%, while in 2021, the proportion of large-scale outbreaks reached 53.8%. In 2020, the scale of outbreaks significantly decreased (approximately 100 people) compared to the pre-pandemic period. In 2021, the number of Salmonella cluster cases (>300 people) related to gimbap restaurants and milmyeon restaurants increased.
- Results from the sentinel surveillance of WFID outbreaks revealed a significant decrease in viral infections during the pandemic period (2020–2021), with levels half those observed before the pandemic. However, the incidence of bacterial infections was constant or even increased when compared with the pre-pandemic period.
- Despite infection control measures, bacterial infections such as salmonellosis and campylobacteriosis occurred at or above average levels in 2020–2021 when compared with pre-pandemic levels. In 2022, more EHEC cases occurred than during the pre-pandemic period. Although reported cases of salmonellosis decreased nationwide during the COVID-19 pandemic, they subsequently increased to levels surpassing the usual rates.
- Regarding viral infections, Group A rotavirus maintained a decreasing trend since 2019, while norovirus had a consistently high incidence each year. In 2022, the number of astrovirus, enteric adenovirus, and sapovirus outbreaks was higher than during the pre-pandemic period.
- Related Factors
- During the observation period, the most frequently suspected source of infection in WFID outbreaks was seafood (217 cases), followed by mixed foods (59 cases) and eggs and poultry (50 cases). Seafood-related outbreaks peaked around 2018, possibly because the average seawater temperature that year was the highest recorded. Eggs and poultry maintained a relatively stable infection rate of approximately 2%. Notably, an increasing trend of person-to-person (P2P) transmission was observed in 2021.
- The identification rate for suspected sources of infection in WFID outbreaks was approximately 20% during 2017–2021, while unidentified sources remained at approximately 75% to 80%, regardless of COVID-19 infection (Table 4). Even when pathogens were detected in human samples, the rate of obtaining consistent test results from environmental samples (e.g., preserved food) was low. This discrepancy can be attributed to the sampling practices in restaurants, where samples are often taken from leftover food ingredients because preserved food samples are difficult to obtain, unlike in schools and companies that provide institutional food services. The sources of infection in salmonellosis outbreaks have consistently been identified as eggs and poultry, pork, bakery products, and other mixed foods such as gimbap (seaweed rice roll), cold noodles, and pancakes with multiple ingredients.
- During the observation period, 2018 had the highest number of heatwave days (31), WFID outbreaks (697), and cases (16,247). In 2020, the number of heatwave days decreased considerably to 7.7, and the incidence of WFIDs reached a record low with 234 outbreaks and 3,459 cases. Furthermore, the number of wet days in 2018 was 10.8, which was unusually low. However, in 2020, the number of wet days nearly tripled to 28.5 (Figure 3).
Results
Annual trends
Monthly trends
Outbreak status by region
Outbreak status by pathogen
Outbreak status by place of occurrence
Outbreak status by outbreak scale
Reported outbreak status
Suspected sources of infection
Meteorological factors
- This study examined the 5-year trends and related factors of WFID outbreaks before and during the COVID-19 pandemic. In the Republic of Korea, more than 400 to 600 group outbreaks of WFID occur every year. Over the past 10 years, the highest number of group outbreaks was confirmed in 2018, with 697 cases. Norovirus has maintained a high incidence every year, and Group A rotavirus has shown a decreasing trend every year since 2019. In 2022, astrovirus, enteric adenovirus, and sapovirus showed higher trends than before the COVID-19 outbreak.
- In a US study, the incidence of food poisoning during the pandemic decreased by as much as 60% [5]. The incidence rate of foodborne infection in 2020 decreased by 26%, reflecting a record-high single-year fluctuation in incidence rates in over 25 years of the FoodNet surveillance [10]. In a UK study, the number of food poisoning cases decreased by 56.4%, from 191 to 83 cases/week [11].
- In the Republic of Korea, the pre-pandemic period (2017–2019) had the highest number of WFID cases. These significantly decreased in 2020 during the pandemic. Moreover, in the last decade (2011–2021), the lowest number of both outbreaks and cases occurred in 2020. However, an increase has been observed since the gradual relaxation of infection control measures in 2021.
- In 2020, while small-scale group outbreaks increased significantly, large-scale outbreaks decreased significantly when compared to the pre-COVID-19 period. Since 2021, large-scale outbreaks related to general restaurants have increased. It is presumed that the relaxation of quarantine measures increased opportunities for gathering and face-to-face contact.
- The high population density of the Seoul capital area (>50% of the national population) makes this area more susceptible to highly communicable infectious diseases because of the high level of interaction among residents [12]. In a US study, states with earlier re-openings and fewer restrictions had the lowest rates of foodborne infectious diseases during the COVID-19 pandemic [5]. In 2020, the weekly occurrence of WFID outbreaks in the Republic of Korea remained below a typical year’s weekly occurrence level, and this downward trend continued nationwide.
- The incidence rate of WFID outbreaks was high in areas such as Jeju, Sejong, and Busan (Table 2), potentially as a result of mass food poisoning in those areas. The level of social distancing measures in metropolitan and non-metropolitan areas during the early stage of the COVID-19 pandemic (2020) can also be considered.
- In 2020, WFID outbreaks in schools decreased, while outbreaks in daycare centers and kindergartens increased. Norovirus was identified as the primary cause of most cases of acute gastroenteritis in daycare centers and schools and was spread via P2P contact. School outbreaks were larger, lasted for less time, had more seasonal patterns, and involved fewer contacts compared with outbreaks in childcare centers [13].
- P2P contact was the predominant mode of transmission for both bacterial and viral pathogens. While the transition to online classes partially restricted P2P transmission in schools, facilities like daycare centers continued to experience ongoing exposure. To accurately assess these variations, based on differences in community and school outbreak patterns and the characteristics of pathogens that primarily spread through the P2P route, more in-depth analysis and enhanced monitoring of WFID outbreak trends are necessary.
- The main source of infection for norovirus is human-to-human transmission, which increased following the relaxation of COVID-19 quarantine measures and the normalization of outdoor activities and face-to-face classes at schools. In particular, this indicated that nonpharmaceutical interventions were effective in reducing the spread of disease transmitted through close person-to-person contact. However, the impact of delayed and low reporting during the relevant period must be taken into consideration.
- Salmonella is a common causative agent of WFID outbreaks in the Republic of Korea, ranking second to norovirus. Salmonellosis outbreaks have been steadily increasing due to the increased consumption of convenience foods and seasonal influences. Foodborne illnesses have a markedly higher incidence among individuals with higher education and income levels, despite their access to high-quality healthcare services, possibly due to more frequent international travel, consumption of high-risk foods, and dining out [5,10].
- The incidence of bacterial diseases characteristically increases when the temperature reaches the ideal range for bacterial growth [14]. A time-series regression study using data from 10 European countries revealed a positive linear relationship between temperature and salmonellosis incidence. The strongest correlation was observed 1 week prior to disease onset. Similarly, positive correlations were found between specific temperature thresholds and the incidence of salmonellosis and campylobacteriosis [15,16]. In the Republic of Korea, the monthly and yearly isolation rates of Salmonella begin to increase in March, coinciding with the rise in average temperature to above 10 °C. High isolation rates are observed from June to October, when the average temperature exceeds 20 °C [14].
- Notable salmonellosis outbreaks have occurred in the Republic of Korea. In 2018, contaminated egg whites, mixed into chocolate cake batter, were identified as the suspected source of infection (“chocolate cake case”). This outbreak affected schools across 12 regions nationwide, where students consumed the contaminated cakes. Other salmonellosis outbreaks linked to contaminated eggs include incidents at a gimbap restaurant in Gyeonggi Province, a milmyeon (wheat noodles) restaurant in Busan in July/August 2021, and a naengmyeon (cold noodles) restaurant in Gyeongsangnam-do in May 2022.In 2022, the cumulative number of salmonellosis outbreaks reached 40, displaying an earlier onset of increase than seen in a typical year, reflecting an upward trend in the number of cases [17].
- In 2021, WFID outbreaks related to outdoor activities such as local festivals and gatherings increased, exhibiting different patterns compared with previous years. From a public health perspective, post-pandemic monitoring of the anticipated rebound is crucial, and includes monitoring of the public’s health management behaviors, testing practices, and international travel trends [18]. Continued post-pandemic surveillance may improve our understanding of the pandemic’s impact on foodborne illnesses and help develop appropriate preventive measures and strategies for major pathogens and related food groups [9]. When analyzing and interpreting long-term post-pandemic trends, it will be important to carefully consider evaluation frame to prevention and management strategies from a more comprehensive point of view [19].
- These incidents underscore the importance of adopting a multidimensional analytical approach and fostering enhanced collaboration among various departments, including the Ministries of Drug and Food Safety and Agriculture, to effectively address major foodborne bacterial infections. In addition, monitoring the shifting trends in dietary consumption patterns and healthcare utilization during the pandemic and strengthening the monitoring of seasonal variations in major infectious diseases is crucial.
- Norovirus accounted for approximately 20% to 30% of group outbreaks over the past 5 years. Before 2020, pathogens such as hepatitis A and Vibrio parahaemolyticus tended to be high, but after 2020, Salmonella, Campylobacter, Clostridium perfringens, and EHEC increased more than twofold. In 2022, a group outbreak of hepatitis E was confirmed, and major bacterial pathogens such as norovirus, Salmonella, and Campylobacter bacteria took center stage. Each year, the causative pathogen could not be identified in >40% of cases.
- In 2020, the unknown pathogen rate continued due to delays in reporting (the staffing for epidemiological investigations was focused on responding to COVID-19) and uncollected specimens (due to the nature of WFID epidemiological investigations) during the pandemic. Problems with rapid acquisition and poor cooperation may have had an impact; therefore, it is necessary to strengthen outbreak management and increase the pathogen identification rate during a pandemic.
- The identification rate of the presumptive source of infection in group outbreaks has been approximately 20% over the past 5 years. Before and during the COVID-19 pandemic, the unknown source infection rate was 75% to 80%.
- The highest proportion of fish and shellfish cases was observed in 2018, which may have been linked to the highest average temperature that year, reflecting climate change. Environmental factors, such as climate change, are directly associated with changes in the distribution of WFID causative pathogens [4]. Several domestic and international studies have reported associations between WFID and meteorological factors, including temperature, humidity, wind speed, and precipitation [20].
- In the Republic of Korea, bacterial gastroenteritis primarily occurs during seasons characterized by high temperature and humidity. During 2010–2019, the incidence of enteric infections increased, especially in 2015–2019, where norovirus, Campylobacter, and Salmonella were the predominant pathogens [21]. In 2020, the most commonly reported foodborne pathogens were norovirus, Salmonella, Campylobacter, and C. perfringens. The incidence of campylobacteriosis and salmonellosis outbreaks decreased from the 11th week of 2020 to a record low in monthly incidence. However, the incidence rate of both diseases increased after the summer of 2020 [22,23]. Salmonellosis outbreaks in the Republic of Korea in 2020 and 2021 either maintained the 5-year average level or increased, with a gradually earlier onset.
- Precipitation amounts are associated with an increased risk of viral diarrhea. Intensive rainfall in summer may not provide a favorable environment for viruses [8]. In a country with a temperate climate like the Republic of Korea, lower temperatures are associated with an increased risk of viral gastroenteritis, including norovirus, rotavirus, and adenovirus infections, with a relatively long lag effect. Conversely, higher temperatures are associated with an increased risk of bacterial gastroenteritis, including salmonellosis and campylobacteriosis, with a relatively short lag effect [20].
- When monitoring and surveilling WFID outbreaks, it is necessary to comprehensively analyze climatic factors and consider the seasonal characteristics of major infectious diseases as predictive factors. In this study, we described the current status of domestic meteorological factors and outbreaks over the past 5 years. However, there were limitations in interpretation, and follow-up research is needed to study the relationship with climate factors.
- In Germany and Denmark, during the COVID-19 pandemic, a decrease in shopping frequency was associated with an increase in frozen and canned food consumption, indicating that people substituted fresh foods with frozen or canned alternatives. The decreased consumption of fresh fruits, vegetables, meat, and dairy products contributed to the reduction in foodborne illnesses [18]. Furthermore, consumer purchasing patterns rapidly shifted to online purchases, accelerating the transition to digital services and influencing food purchasing preferences. Dining at home replaced dining out; hence, a significant increase in food delivery expenditures was observed [6].
- The closure of institutional food service facilities in the Republic of Korea led to an explosive increase in food delivery services. However, WFID outbreaks have consistently occurred in relation to unlicensed or small-scale food delivery businesses, which highlights the potential risks associated with the use of such services. Changes in demand and food consumption patterns during the pandemic indicate the need to strengthen the management and supervision of unlicensed businesses, including hygiene inspections and the provision of employee education.
- The decrease in WFID outbreaks can be attributed to infection control measures implemented during the pandemic and to a combination of environmental, behavioral, political, economic, and social factors, including changes in dietary consumption patterns. This study did not analyze social and economic factors; therefore, further research is necessary to evaluate the impact of these factors.
Discussion
- During the COVID-19 pandemic, a significant decrease in overall WFID outbreaks was observed in the Republic of Korea. However, outbreaks of certain bacteria, such as Salmonella, continued to increase (with seasonal fluctuations). The patterns of WFID outbreaks before and during the pandemic exhibited distinctive characteristics, influenced by seasonal factors and infection control measures. Therefore, enhanced monitoring for major infectious diseases should also consider changes in dietary consumption patterns and seasonal factors. Long-term changes in post-pandemic surveillance data must be contextualized to develop specific pathogen-targeted preventive measures and strategies.
Conclusion
- • Waterborne and foodborne infectious disease (WFID) outbreaks significantly decreased during the coronavirus disease 2019 (COVID-19) pandemic, whereas bacterial and viral outbreaks increased and decreased, respectively, depending on the major pathogens.
- • The infection control measures for COVID-19 resulted in different outbreak patterns across various settings. In 2020, school-related outbreaks decreased, whereas restaurant-related outbreaks remained constant. Thus, strengthening outbreak management strategies through hygiene inspections, monitoring, education, and promotion is crucial.
- • During the COVID-19 pandemic, a consistent increase in WFID outbreaks coincided with an increase in food delivery services and convenience food consumption, as well as the sustained occurrence of seasonal outbreaks. Therefore, enhanced monitoring for major infectious diseases should also consider changes in dietary consumption patterns and seasonal factors. For effective prevention and control strategies, multidimensional analyses should be used to determine the predictive factors.
HIGHLIGHTS
-
Ethics Approval
This study was approved by the Institutional Review Board of the KDCA (IRB No: 2023-03-01-PE-A). The requirement for informed consent was waived by the IRB.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
All data generated or analyzed during this study are included in this published article. For other data, these may be requested through the corresponding author.
-
Authors’ Contributions
Conceptualization: all authors; Data curation: EK; Formal analysis: EK; Investigation: EK; Methodology: all authors; Project administration: all authors; Resources: EK; Software: EK; Supervision: BIK; Validation: EK; Visualization: EK; Writing–original draft: EK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Article information

| Region |
2017 |
2018 |
2019 |
2020 |
2021 (estimate) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inc. | Pop. | IRa) | Inc. | Pop. | IRa) | Inc. | Pop. | IRa) | Inc. | Pop. | IRa) | Inc. | Pop. | IRa) | |
| Total | 539 | 7,770 | 15.0 | 691 | 13,033 | 25.1 | 592 | 7,630 | 14.7 | 234 | 3,323 | 6.4 | 470 | 7,874 | 15.2 |
| Seoul | 71 | 1,208 | 12.3 | 103 | 3,591 | 36.8 | 82 | 1,397 | 14.4 | 19 | 261 | 2.7 | 47 | 799 | 8.4 |
| Busan | 15 | 415 | 12.0 | 22 | 747 | 21.7 | 28 | 652 | 19.1 | 20 | 268 | 7.9 | 47 | 1184 | 35.3 |
| Daegu | 21 | 127 | 5.1 | 19 | 395 | 16 | 17 | 297 | 12.2 | 11 | 87 | 3.6 | 10 | 221 | 9.3 |
| Incheon | 31 | 354 | 12.0 | 42 | 521 | 17.6 | 37 | 709 | 24.0 | 10 | 216 | 7.3 | 23 | 280 | 9.5 |
| Gwangju | 15 | 82 | 5.6 | 12 | 64 | 4.4 | 13 | 66 | 4.5 | 6 | 74 | 5.1 | 10 | 65 | 4.5 |
| Daejeon | 8 | 206 | 13.7 | 4 | 47 | 3.2 | 16 | 169 | 11.5 | 4 | 72 | 4.9 | 8 | 28 | 1.9 |
| Ulsan | 9 | 81 | 7.0 | 8 | 113 | 9.8 | 3 | 28 | 2.4 | 4 | 32 | 2.8 | 4 | 35 | 3.1 |
| Sejong | 4 | 22 | 7.9 | 3 | 184 | 58.6 | 5 | 43 | 12.6 | 4 | 40 | 11.2 | 7 | 331 | 89.0 |
| Gyeonggi | 131 | 2,485 | 19.3 | 156 | 2,894 | 22.1 | 118 | 1,583 | 12.0 | 57 | 1,006 | 7.5 | 111 | 2,017 | 14.9 |
| Gangwon | 39 | 343 | 22.1 | 29 | 515 | 33.4 | 26 | 216 | 14.0 | 8 | 98 | 6.4 | 24 | 371 | 24.1 |
| Chungcheongbuk-do | 22 | 288 | 18.1 | 28 | 385 | 24.1 | 49 | 399 | 24.9 | 11 | 168 | 10.5 | 24 | 438 | 27.4 |
| Chungcheongnam-do | 57 | 431 | 20.4 | 78 | 708 | 33.3 | 65 | 439 | 20.7 | 8 | 142 | 6.7 | 46 | 660 | 31.1 |
| Jeollabuk-do | 20 | 433 | 23.3 | 26 | 236 | 12.8 | 33 | 378 | 20.8 | 13 | 126 | 7.0 | 14 | 219 | 12.3 |
| Jeollanam-do | 23 | 180 | 9.5 | 73 | 431 | 22.9 | 2 | 7 | 0.4 | 12 | 100 | 5.4 | 18 | 168 | 9.2 |
| Gyeongsangbuk-do | 21 | 581 | 21.6 | 66 | 1,364 | 51.0 | 37 | 466 | 17.5 | 22 | 276 | 10.5 | 25 | 261 | 9.9 |
| Gyeongsangnam-do | 29 | 259 | 7.7 | 43 | 610 | 18.1 | 28 | 322 | 9.6 | 13 | 150 | 4.5 | 37 | 600 | 18.1 |
| Jeju | 23 | 275 | 41.9 | 9 | 228 | 34.2 | 7 | 120 | 17.9 | 12 | 329 | 48.8 | 15 | 197 | 29.1 |
Values are presented as number only. The reported data for years 2017–2021 are provisional. Incidence rate=(no. of cases/no. of population)×100,000 (based on the status of the resident registered population provided by the Ministry of the Interior and Safety in 2021).
Inc., incidence; pop., population; IR, incidence rate.
a) Incidence per 100,000 population.
- 1. Korea Disease Control and Prevention Agency (KDCA). 2022 Guidelines for water- and foodborne infectious diseases [Internet]. KDCA; 2022 [cited 2023 Nov 13]. Available from: https://www.kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=719059&seq=1. Korean.
- 2. Kim NO, Hong S, Chun JH, et al. Laboratory-based surveillance of water- and food-borne infectious disease-causing bacteria in the Republic of Korea, 2016-2018. Public Health Wkly Rep 2019;12:898−903. Korean.
- 3. Korea Disease Control and Prevention Agency (KDCA). 2020-2021 epidemiological survey of infectious diseases: annual report [Internet]. KDCA; 2022 [cited 2023 Nov 13]. Available from: https://npt.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaView.do?pblctDtaSeAt=5&pblctDtaSn=2780. Korean.
- 4. Kim S, Kim J, Choi BY, et al. Trends in gastrointestinal infections before and during non-pharmaceutical interventions in Korea in comparison with the United States. Epidemiol Health 2022;44:e2022011.ArticlePubMedPMCPDF
- 5. Akil L, Ahmad HA. Socioeconomic impacts of COVID-19 pandemic on foodborne illnesses in the United States. Eur J Environ Public Health 2023;7:em0128.ArticlePubMedPMC
- 6. Ben Hassen T, El Bilali H, Allahyari MS. Impact of COVID-19 on food behavior and consumption in Qatar. Sustainability 2020;12:6973. Article
- 7. Nielsen RT, Dalby T, Emborg HD, et al. COVID-19 preventive measures coincided with a marked decline in other infectious diseases in Denmark, spring 2020. Epidemiol Infect 2022;150:e138.ArticlePubMedPMC
- 8. Sung J, Cheong HK, Kwon HJ, et al. Pathogen-specific response of infectious gastroenteritis to ambient temperature: national surveillance data in the Republic of Korea, 2015-2019. Int J Hyg Environ Health 2022;240:113924. ArticlePubMed
- 9. Korea Meteorological Administration. KMA weather data service [Internet]. Korea Meteorological Administration; 2023 [cited 2023 Nov 13]. Available from: https://data.kma.go.kr/cmmn/main.do. Korean.
- 10. Ray LC, Collins JP, Griffin PM, et al. Decreased incidence of infections caused by pathogens transmitted commonly through food during the COVID-19 pandemic: Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2017-2020. MMWR Morb Mortal Wkly Rep 2021;70:1332−6.ArticlePubMedPMC
- 11. Nash K, Lai J, Sandhu K, et al. Impact of national COVID-19 restrictions on incidence of notifiable communicable diseases in England: an interrupted time series analysis. BMC Public Health 2022;22:2318. ArticlePubMedPMCPDF
- 12. Ha JH, Lee JY, Choi SY, et al. COVID-19 waves and their characteristics in the Seoul Metropolitan Area (Jan 20, 2020-Aug 31, 2022). Public Health Wkly Rep 2023;16:111−36. Korean.
- 13. Mattison CP, Calderwood LE, Marsh ZA, et al. Childcare and school acute gastroenteritis outbreaks: 2009-2020. Pediatrics 2022;150:e2021056002.ArticlePubMedPMCPDF
- 14. Jeong HJ, Shin E, Park J, et al. Trends in serotype distribution of Salmonella enterica isolated from diarrheal patients in Korea, 2019 to 2021. Public Health Wkly Rep 2022;15:2615−31. Korean.
- 15. Anonymous. Annual report on zoonoses in Denmark 2020 [Internet]. National Food Institute, Technical University of Denmark; 2021 [cited 2023 Nov 13]. Available from: https://www.food.dtu.dk/-/media/institutter/foedevareinstituttet/publikationer/pub-2021/rapport-annual-report-on-zoonoses-2020.pdf?la=da&hash=B8240D99D34E8FDDC1524C064B54627651F50179.
- 16. Andhikaputra G, Sharma A, Sapkota A, et al. Quantifying the effects of anomalies of temperature, precipitation, and surface water storage on diarrhea risk in Taiwan. Epidemiol Health 2023;45:e2023024.ArticlePubMedPMC
- 17. Korea Disease Control and Prevention Agency (KDCA). 2022 epidemiological survey of infectious diseases: annual report [Internet]. KDCA; 2023 [cited 2023 Nov 13]. Available from: https://npt.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaView.do?pblctDtaSeAt=5&pblctDtaSn=2780. Korean.ArticlePubMed
- 18. Dougherty B, Smith CR, Forrest RO, et al. Considerations for enteric disease surveillance in a post-COVID-19 pandemic world: a Canadian perspective. Foodborne Pathog Dis 2023;20:121−2.ArticlePubMedPMC
- 19. Qi X, Guo J, Yao S, et al. Comprehensive dynamic influence of multiple meteorological factors on the detection rate of bacterial foodborne diseases under Spatio-Temporal Heterogeneity. Int J Environ Res Public Health 2023;20:4321. ArticlePubMedPMC
- 20. Chen L, Wang J, Zhang R, et al. An 11-year analysis of bacterial foodborne disease outbreaks in Zhejiang Province, China. Foods 2022;11:2382.
- 21. Korea Disease Control and Protection Agency (KDCA). The first climate and health impact assessment report [Internet]. KDCA; 2022 [cited 2023 Nov 13]. Available form: https://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=719063&cg_codc=&act=view&nPage=1. Korean.
- 22. Statens Serum Institut. Outbreak with campylobacter can originate epidemiology and infection 9 from a local dairy [Internet]. Statens Serum Institut; 2020 [cited 2023 Nov 13]. Available from: https://www.ssi.dk/aktuelt/nyheder/2020/campylobacterudbrud. Danish.
- 23. Statens Serum Institut. Several foodborne outbreaks in Denmark at the moment [Internet]. Statens Serum Institut; 2020 [cited 2023 Nov 13]. Available from: https://www.ssi.dk/aktuelt/nyheder/2020/flere-fodevarebarne-udbrud-i-danmark-i-ojeblikket. Danish.
References
Figure & Data
References
Citations



 Cite
Cite