Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(6); 2023 > Article
-
Original Article
The effect of the COVID-19 pandemic on the trends and characteristics of natural and unnatural deaths in an urban Sri Lankan cohort viewed through retrospective analysis of forensic death investigations from 2019 to 2022 -
Sameera Anuruddha Gunawardena1,2
 , Nishani Dassanayake1
, Nishani Dassanayake1 , Buddhika Indeewarie Keerawelle1
, Buddhika Indeewarie Keerawelle1 , Shivasankarie Kanthasamy1
, Shivasankarie Kanthasamy1 , Hasini Ranganatha1
, Hasini Ranganatha1 , Jayani Wathsala Gunawardana1
, Jayani Wathsala Gunawardana1
-
Osong Public Health and Research Perspectives 2023;14(6):468-482.
DOI: https://doi.org/10.24171/j.phrp.2023.0175
Published online: November 23, 2023
1Department of Forensic Medicine and Toxicology, Faculty of Medicine, University of Colombo, Colombo, Sri Lanka
2Department of Pathology, School of Medicine, International Medical University, Kuala Lumpur, Malaysia
- Corresponding author: Sameera Anuruddha Gunawardena Department of Pathology, School of Medicine, International Medical University, No. 126, Jln Jalil Perkasa 19, Bukit Jalil, 57000 Kuala Lumpur, Malaysia E-mail: sameera@imu.edu.my; sameera@fortox.cmb.ac.lk
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,200 Views
- 46 Download
Abstract
-
Objectives
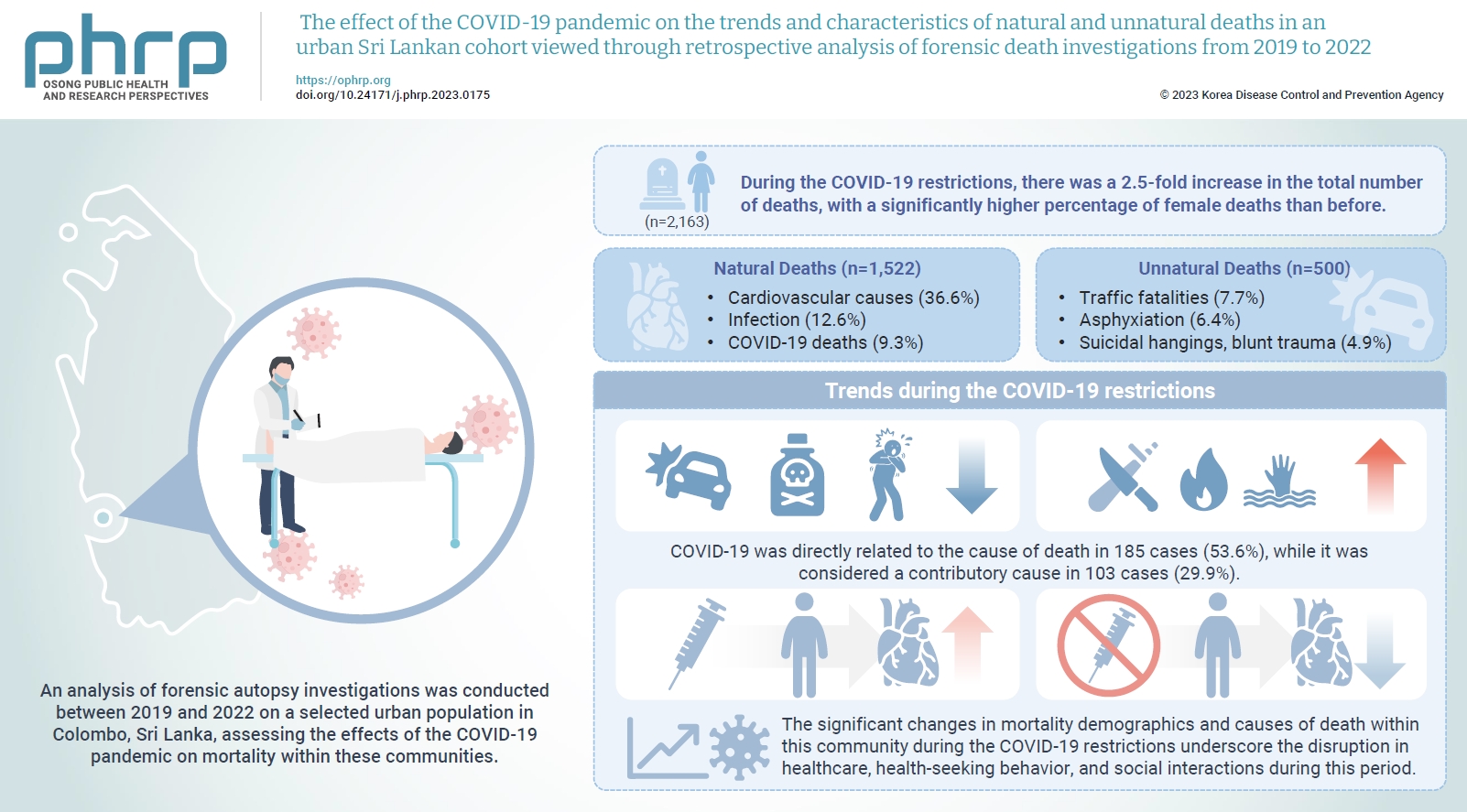
- The coronavirus disease 2019 (COVID-19) pandemic has had a severe impact on global health. Apart from the disease itself, the strict restrictions and lockdowns enforced to minimize its spread have also substantially disrupted personal and public health.
-
Methods
- An analysis of forensic autopsy investigations was conducted between 2019 and 2022 on a selected urban population in Colombo, Sri Lanka, assessing the effects of the COVID-19 pandemic on mortality within these communities.
-
Results
- During the COVID-19 restrictions, there was a 2.5-fold increase in the total number of deaths, with a significantly higher percentage of female deaths than before. The majority of these deaths were due to cardiovascular causes, while COVID-19-related deaths ranked third overall. The highest proportion of COVID-19 deaths occurred among unvaccinated females. The monthly frequency of deaths from traffic accidents, poisoning, and asphyxiation decreased, while deaths from blunt trauma, sharp trauma, burns, and immersion increased. There was also a rise in blunt homicides and a greater number of femicides during the COVID-19 restrictions than in the pre-pandemic period. A significantly higher percentage of males who received the COVID-19 vaccine died from cardiovascular causes compared to those in the unvaccinated group.
-
Conclusion
- The significant changes in mortality demographics and causes of death within this community during the COVID-19 restrictions underscore the disruption in healthcare, health-seeking behavior, and social interactions during this period. The vulnerability of individuals residing in highly urbanized areas with lower socioeconomic status, particularly women, is brought into sharp focus.
- Coronavirus disease 2019 (COVID-19) was first reported in Wuhan, Hubei Province, China, on December 12, 2019. Shortly thereafter, the Wuhan Municipal Health Commission officially reported a cluster of severe pneumonia cases [1–3]. This marked the beginning of a global crisis caused by a novel and highly contagious coronavirus, known as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The symptoms of COVID-19 range from mild fever, cough, and shortness of breath to more severe and potentially fatal pneumonia and respiratory distress [4,5]. By June 2023, the global death toll had exceeded 6.9 million, with over 760 million people infected [6]. COVID-19 transmission by asymptomatic carriers is a particular concern [7,8]. In response, the world has undergone dramatic shifts in social behavior and lifestyle. Preventive measures such as the use of respiratory masks and face shields, hand sanitization, social distancing, travel restrictions, and community lockdowns have been enforced worldwide.
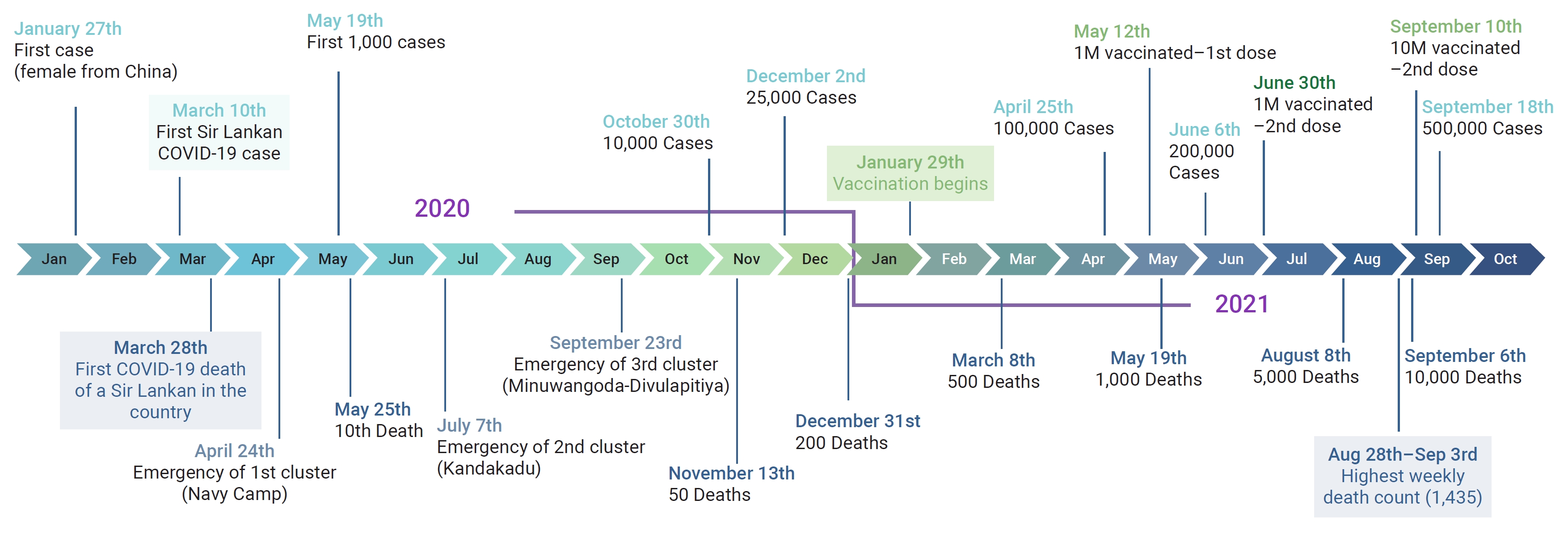
- By the time the World Health Organization declared the outbreak a pandemic on March 11, 2020 [9], the Sri Lankan government had already established a national action committee. This committee, composed of government officials, public health administrators, and military officials, was tasked with planning and implementing strategies to control the disease [10]. Law enforcement and military personnel enforced mandatory quarantine, an island-wide curfew, and travel restrictions after several cases were detected and the first death due to COVID-19 occurred in March 2020 [11–13]. By May 2020, the number of cases had reached 1,000, with a case fatality rate of 1% (Figure 1). This figure included the first reported case of post-mortem detection of SARS-CoV-2 through reverse-transcription polymerase chain reaction (RT-PCR) in a forensic autopsy [14]. Despite the emergence of 3 distinct clusters of COVID-19 by the end of October 2020 [15–17], the case fatality rate remained below 0.5%. On November 13, 2020, a new government circular mandated RT-PCR testing of all deaths within the Western province [18]. This resulted in all home deaths being sent to medicolegal institutions within the country for COVID-19 screening. Autopsies were only conducted after nasopharyngeal swabs were confirmed negative. The number of COVID-19 cases continued to rise, and by January 1, 2021, Sri Lanka had recorded a total of 43,299 cases with 204 deaths [19].
- Sri Lanka initiated its vaccination program in late January 2021, initially targeting frontline healthcare workers and security personnel. The public vaccination campaign began in early March, achieving coverage of over 1 million individuals by May 2021. However, following the New Year celebrations in April, a third wave of infections struck, pushing the death toll past 3000 by mid-2021 [20]. Travel restrictions and public place closures were intermittently enforced, and specific areas with high case rates were isolated. The highest weekly death toll (1,435) was recorded between August 28 and September 3, which brought the overall death toll to 10,000 [21]. This third wave was attributed to the Delta variant, which increased the case fatality rate from 0.6% to 3% [22]. However, a significant decline in the daily death toll and case density was observed from mid-September. By the end of October, the government officially lifted travel restrictions and curfews [23]. Most public and private services gradually resumed normal operations in the following months, and the requirement for PCR screening of deaths was also removed. COVID-19 deaths continued at a significantly reduced rate, and aside from a minor surge in mid-February, very few deaths were reported in 2022.
- Numerous secondary social, economic, and political factors have played a role in disrupting lifestyles and overall health and well-being during the COVID-19 pandemic [24]. Beyond government-imposed social restrictions, apprehension and mistrust among individuals also led to increased distancing, psychosocial discord, and isolation. Social stigma emerged as a powerful determinant influencing the reporting and presentation of those affected by COVID-19 [25]. In line with the global trend of disbelief, conspiracy theories, and myths related to the pandemic [26,27], Sri Lanka also grappled with many misconceptions about COVID-19. One contentious issue was the mandate to cremate all COVID-19 victims within 24 hours, which sparked considerable social, political, and religious controversy [28–31]. These factors collectively resulted in a health burden surpassing the actual pathogenicity of SARS-CoV-2.
- Many studies have demonstrated an increase in mortality during the pandemic, primarily due to cardiovascular and cerebrovascular causes [32–35]. The presence of co-morbidities, particularly cardiovascular disease, is a significant risk factor for mortality [36]. Nearly all studies and reviews have highlighted the disruption of healthcare, unequal access to healthcare services, and the collapse of social and communal infrastructure during the pandemic period [37–39]. Reports have also described escalated levels of domestic violence and abuse during lockdown periods, further exacerbating the psychosocial health of the affected communities [40–42].
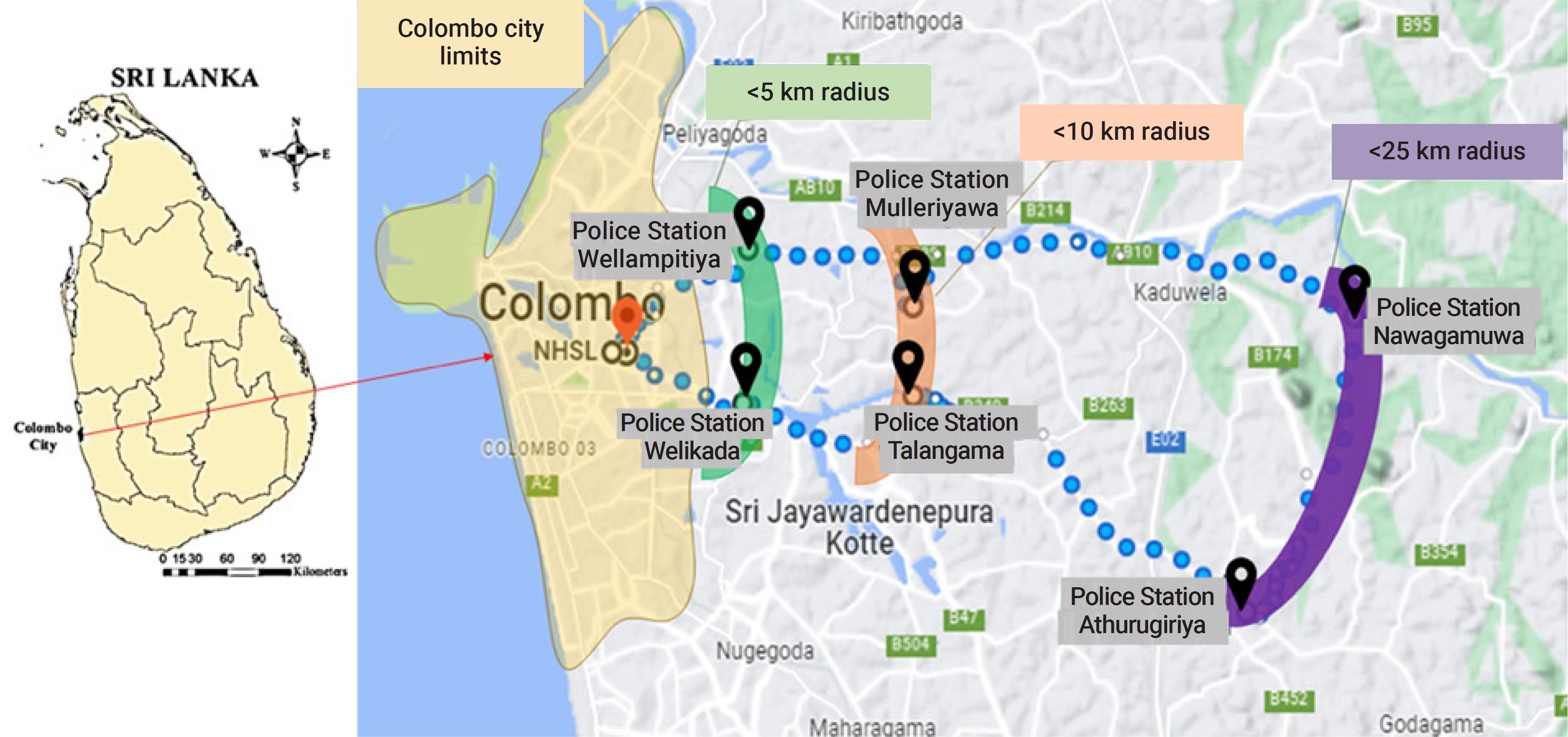
- Within this context, we conducted a retrospective analysis of the forensic autopsies performed at the Department of Forensic Medicine and Toxicology (DFMT) of the University of Colombo. This department has been exclusively providing medicolegal services to 6 police areas within the Colombo district for over 50 years (Figure 2).
- The aims of our study included (1) determining whether there were any shifts in the patterns of natural and unnatural deaths within this community during the COVID-19 restrictions, compared to the periods before and after, (2) establishing the frequency of deaths attributed to COVID-19, and (3) contrasting the mortality trends between individuals who received the COVID-19 vaccine and those who did not.
Introduction
- Study Setting and Case Selection
- Cases were selected from the forensic autopsies conducted at the DFMT from January 1, 2019 to December 31, 2022. We only selected cases that fell within the jurisdiction of the department’s 6 police areas, which serve fixed populations with distinct regional and communal characteristics, constituting approximately one-eighth of the Colombo district population. Depending on their geographic location relative to the city limits of Colombo, this cohort could be divided into 3 groups of residents living within 5 km, 10 km, and 25 km, respectively. The first 2 subgroups are highly urbanized [43]. There is little variation in socioeconomic standards among the 6 police divisions, except for a higher proportion of slum dwellings in the group living within 5 km. Sudden natural deaths, as well as all types of unnatural and suspicious deaths that occur within this community, are referred to the DFMT for forensic autopsies. Information about the deceased, including the circumstances surrounding death, past medical conditions, and vaccination history, is obtained from next of kin, medical records, eyewitnesses, and attending police officers. Forensic pathologists conduct autopsies, and upon completion, a medical certificate of cause of death is issued, including an opinion on whether the death is natural, accidental, suicidal, or homicidal. In some situations, cases remain under investigation until further tests can be conducted or are deemed as deaths due to unascertainable causes. This practice remained unchanged during the COVID-19 restrictions. However, when home deaths occurred within quarantined families or in lockdown areas, law enforcement personnel transported the bodies for forensic autopsies following the inquest. In these situations, the family was interviewed via telephone or video conferencing. We excluded deaths referred for a second autopsy or review, deaths of unidentified individuals, and skeletonized remains referred for forensic anthropological examination. For specific statistical analyses and comparisons, such as age, vaccination details, or causes of death, cases where the relevant data was not available were excluded accordingly.
- Data Collection
- All records, encompassing personal details, autopsy reports, medical certificates of cause of death, and digital copies of documented information from police and medical records provided to the DFMT at the time of autopsy, are preserved in the departmental database, from which relevant data were retrieved. The average number of autopsies conducted each month over the previous 8 years (2010–2018) was also determined from the departmental registers. Information regarding COVID-19 positivity was based on RT-PCR test reports issued by authorized government laboratories, which were incorporated into the autopsy reports. Only cases where COVID-19 was listed in part 1 of the cause of death form were classified as COVID-19 deaths.
- Details about the epidemiology and transmission of COVID-19, the duration of lockdowns and travel restrictions, and the extent of vaccination coverage were gathered from government press releases and news media. The period from January 1, 2019 to March 20, 2020 was designated as the pre-COVID-19 era. The period of COVID-19 restrictions was identified as spanning from March 21, 2020 to October 31, 2021. The post-COVID-19 period was defined as the period from November 1, 2021 to December 31, 2022.
- The official vaccination program began on January 29, 2021, but the initial recipients were restricted to healthcare workers, security personnel, and individuals over 65 years of age. The general public did not start receiving routine vaccinations until March 2021. As such, we designated the period after March 15, 2021 as the post-vaccination period. The vaccination status of the deceased was determined based on information provided by the next of kin. If the deceased had received at least 1 dose, they were classified as part of the vaccinated group.
- Statistical Analysis
- We utilized Microsoft Excel ver. 15.20 (Microsoft Corp.) for managing descriptive data. IBM SPSS ver. 24.0 (IBM Corp.) was employed for comparative statistical analysis and significance tests. The Kolmogorov-Smirnov test revealed that the age distributions did not follow a normal distribution (p<0.001). Consequently, the Mann-Whitney U test was used for age comparisons. We did not remove any outliers. The chi-square test was used for comparisons between groups of ordinal variables. We considered a p-value of ≤0.05 as statistically significant for all tests. When analyzing the broad categories of deaths, we excluded those that were still under investigation or due to unascertainable causes. To better represent the changes in death rates within the community, we calculated the monthly frequency for each category of death.
- Ethical Approval
- Ethical approval for this study was granted by the Ethics Review Committee of Faculty of Medicine, University of Colombo, Sri Lanka (EC-21-055).
Materials and Methods
- General Demographic Characteristics
- Between 2019 and 2022, the DFMT received 2,197 death referrals, of which 2,163 cases met the inclusion criteria. Table 1 illustrates the breakdown of these cases before, during, and after COVID-19 restrictions, with age ranges and the sex distribution. The monthly autopsy load from 2010 to 2018 typically ranged between 25 and 35 cases. However, after the implementation of COVID-19 restrictions in March, the monthly case load dropped noticeably compared to the pre-COVID-19 period. This was followed by a significant increase starting in December 2020 (Figure 3A). During the COVID-19 restrictions, there were 1,162 deaths, accounting for 53.7% of the total for all 4 years. After the vaccination program started in March, there were 739 deaths (33.6%) in the final 8 months of the COVID-19 restrictions (Figure 3B). There was then a swift decline in the number of cases until the end of 2022.
- In all 3 periods, males constituted the majority of deaths (76.1%, 62.4%, and 76.6%, respectively). During the COVID-19 restrictions, a higher proportion of deaths occurred among females (37.6%) than in both the pre-COVID-19 (23.9%) and post-COVID-19 (23.4%) periods. This difference was statistically significant (χ2(2)=48.69, p<0.001). For 55 deaths (40 males and 15 females), reliable age information was not available, and these cases were therefore excluded from age comparisons. The mean (standard deviation) and median (interquartile range) ages of the total populations were 60.13 (±18.69) and 62.00 (49.00–74.00) respectively. The Mann-Whitney U test revealed significant differences in the median age between the pre-COVID-19 and COVID-19 periods (p<0.001), the COVID-19 and post-COVID-19 periods (p<0.001), and the pre-COVID-19 and post-COVID-19 periods (p=0.001). In all 3 periods, the median ages of females were significantly higher than those of males (p<0.001) (Table 1). However, during the COVID-19 restrictions, there was a notable number of females who died at very young ages (Figure 3C).
- Significant differences were also observed in the proportion of deaths before and during COVID-19 restrictions among police divisions (χ2(2)=9.93, p=0.007). The group located less than 5 km from the city experienced the highest number of deaths during the COVID-19 restrictions, marking a 7.6% increase from the numbers recorded prior to the pandemic.
- Trends and Characteristics of Natural and Unnatural Deaths
- Excluding 141 cases where the circumstances were either unascertainable or still under investigation (Figure 4A), the most common broad category of death was cardiovascular diseases (36.6%). This was followed by non-COVID-19-related infections (12.6%), and then COVID-19 deaths (9.3%). Among deaths due to unnatural circumstances, traffic fatalities were the most prevalent (7.7%), followed by asphyxiation (6.4%), which primarily included suicidal hangings, and blunt trauma (4.9%). The distribution of these broad categories of death across the 3 periods is presented in Table 2. Significant differences were observed in the proportions of natural, accidental, suicidal, and homicidal circumstances of death across the 3 periods (χ2(6, n=2,022)=45.78, p<0.001). Most deaths in all 3 periods were due to natural circumstances. Compared to accidents and homicides, there was a more significant reduction in the proportion of suicides during the COVID-19 restrictions.
- The proportions and monthly frequencies of both natural and unnatural causes of death varied significantly across the 3 periods (Table 2; Figure 4B). During the COVID-19 restrictions, the monthly frequencies of all categories of natural deaths, with the exception of venous thrombosis, increased (Figure 4B). Chronic lung diseases and malignancies experienced more than a 2-fold increase, while chronic liver disease, chronic kidney disease, and diabetic complications showed approximately 3-fold increases. The monthly frequency of cardiovascular deaths rose from 13.2 to 21.8 during the COVID-19 restrictions, before falling to 9.1 in the post-COVID-19 period. Traffic fatalities decreased from 4.5 per month to 2.8 per month, and firearm deaths fell from 0.3 to 0.1 per month. The reduction in the proportion of traffic fatalities during the COVID-19 restrictions, from 12.0% to 4.6%, was statistically significant (χ2(1)=31.10, p<0.001) (Table 2). Conversely, the proportions of deaths due to blunt trauma, immersion (drowning), and burns were higher during the COVID-19 restrictions, and cases of blunt homicidal trauma were only observed during this period (Table 2). No homicidal deaths among females were reported in the pre-COVID-19 period, but 5 females were killed during the COVID-19 restrictions. In the post-COVID-19 restriction period, 90% of male homicides were due to sharp weapon trauma.
- Post-mortem PCR screening for COVID-19 was conducted on 1,133 bodies from November 1, 2020 to March 4, 2022. Of these, 345 bodies tested positive. Among the positive cases, COVID-19 was directly related to the cause of death in 185 cases (53.6%), while it was considered a contributory cause in 103 cases (29.9%). The remaining cases were classified as incidental findings. There were 2 instances where the clinical history and pathological features strongly suggested COVID-19 as the cause of death, yet the post-mortem PCR results were negative. One case was classified as a COVID-19 death despite the absence of a PCR confirmation. Over 75% of the COVID-19 deaths originated from police divisions located within the <5 km and <10 km groups. The majority of the deceased were over 65 years old, and the proportion of females who died from COVID-19 was higher than that of males, with a female-to-male ratio of 102:86.
- Natural Deaths during the Post-Vaccination Period
- In the post-vaccination period, starting on March 15, 2021, there were 1,145 recorded deaths. Of these, 495 individuals (362 males and 133 females) had received some form of COVID-19 vaccination, while 381 (222 males and 159 females) had not. For 269 deaths (175 males and 94 females), vaccination data was unavailable. The most widely distributed vaccines were Sinopharm (80%) and Covishield (13.1%). Among those vaccinated, 77.3% of males and 60.9% of females had received both doses. Of the 876 deaths for which vaccination data was available, 657 were attributed to confirmed natural causes, with cardiovascular diseases being the most common, followed by COVID-19. All but 5 COVID-19-related deaths occurred during the post-vaccination period. Table 3 provides a comparison of the broad causes of death between vaccinated and non-vaccinated individuals, broken down by sex.
- There was a significantly higher percentage of vaccinated males among those who died due to cardiovascular causes (χ2(1)=22.08, p<0.001). Their median age was not significantly different from that of the non-vaccinated males (z=–0.67, p=0.504). However, the median age of vaccinated females who died of cardiovascular causes was significantly lower than that of non-vaccinated females (z=–2.99, p=0.003). Of the 145 deaths attributed to COVID-19, 29 males and 26 females had received at least 1 dose of the COVID-19 vaccines. The highest percentage of COVID-19 deaths occurred among non-vaccinated females, although this was not statistically significant (χ2(1)=1.786, p=0.181). The majority of deaths occurred in individuals 65 years and older, with no significant difference found between the median ages of the vaccinated and non-vaccinated groups (z=–0.72, p=0.470). There were 10 COVID-19 deaths in those under 40 years, all of whom were non-vaccinated. No significant differences were found in either the percentages or median ages of vaccinated and non-vaccinated males and females in other categories of natural deaths.
Results
- Changes in the Frequency and Demography of Deaths during the COVID-19 Restrictions
- The observed increase in mean and median ages of deaths during the COVID-19 restrictions is attributable to a decrease in unnatural deaths, such as traffic fatalities, which typically involve younger individuals, and an increase in sudden natural deaths among the elderly population. During the COVID-19 restrictions, there was nearly a 15% rise in the proportion of female deaths compared to the other 2 periods. This increase could be partially attributed to the high number of females who succumbed to COVID-19, as discussed in more detail below. It is widely recognized that females often face discrimination during times of disaster and crisis [44], which has been observed globally during the COVID-19 pandemic as well [45,46]. Numerous reports have also highlighted increased instances of domestic violence, sexual violence, and gender-based harassment during the COVID-19 lockdowns, all of which predominantly affect females [47,48]. In Sri Lanka, a predominantly patriarchal society, the responsibility of household duties primarily falls on females, and their health needs are often neglected. A high prevalence of domestic violence, particularly among lower socioeconomic communities, has always been a significant issue. The occurrence of 5 femicides exclusively during the COVID-19 restrictions in our cohort further underscores the vulnerability of females during such crisis periods.
- The higher percentage of deaths within a 5-km radius of Colombo, specifically from the Welikada and Wellampitiya police divisions, during the COVID-19 restrictions is noteworthy. These 2 divisions were frequently subjected to strict curfews and lockdowns during this period. Despite their proximity to major tertiary hospitals and clinics in Colombo, the stringent restrictions likely impeded access to healthcare. These areas are characterized by high levels of housing congestion and limited living space. During the lockdowns, these highly urbanized communities faced numerous challenges, including overcrowded houses, reduced ventilation, decreased sanitation, and the closure of food outlets [49]. These conditions contributed to malnutrition, lower immunity, and a decline in the overall health status of urban residents [50]. In some instances, we found that despite exhibiting severe illness symptoms such as chest pains and headaches, the deceased had resorted to home remedies. Some even refrained from seeking medical treatment due to fear of contracting COVID-19. In contrast, residents in the more distant suburbs of Athurugiriya and Nawagamuwa, located almost 25 km away from the city limits, live in a more dispersed housing layout with ample garden space. Although these residents may not have had access to tertiary healthcare facilities during this period, they had greater freedom of movement to obtain primary and basic community healthcare services. Many households in these areas are also more self-sufficient, growing their own food, which likely contributed to a healthier lifestyle. This disparity in death rates between the 2 communities underscores the negative impacts of urbanization and overcrowding during a pandemic with airborne transmission.
- The Impact of COVID-19 Restrictions on Unnatural Deaths
- In our cohort, traffic fatalities decreased by nearly 50% during the lockdowns, a figure that aligns with studies reported from other regions [51,52]. Although the reduced traffic volume due to lockdowns and travel restrictions has led to fewer traffic collisions, it also encouraged higher speeds and reckless driving, resulting in more fatalities [53]. A review of road traffic fatalities across multiple countries revealed that strict lockdown measures decreased the crash fatality ratio by 0.36% [54]. The most significant reduction was observed in pedestrian deaths, with some studies indicating a decline of over 60% during the lockdown periods [55].
- Sri Lanka is known for its high suicide rate [56,57]. Our study did not reveal a significant shift in the frequency of suicides during the COVID-19 restrictions. A global surge in suicides was anticipated due to social isolation, economic difficulties, and fear of infection during the COVID-19 pandemic [58–60]. However, a paradoxical decrease was observed in most countries, at least during the initial stages [61], and the predicted alarming increase in suicides did not materialize [62]. Another study conducted in Sri Lanka reported a decrease in hospital admissions due to self-harm from poisoning during the COVID-19 restrictions, but no change in the overall suicide trend [63].
- Sri Lankan households typically comprise of extended families. During lockdown periods, the constant presence of family members at home may have served as a mitigating factor for suicidal tendencies. Conversely, increased family contact could potentially lead to more conflicts. This could account for the observed rise in suicidal burns, which are generally considered impulsive suicides.
- It is noteworthy that blunt homicides were only observed during the period of COVID-19 restrictions, potentially reflecting an increased frequency of interpersonal conflicts and domestic violence during lockdowns. An earlier analysis of homicides in Sri Lanka revealed that blunt and sharp weapon trauma were predominantly associated with sudden provocations and robbery homicides, while firearms were typically used in terrorist activities, contractual, and underworld killings [64]. Therefore, the heightened frequency of blunt and sharp weapon homicides during and after the period of COVID-19 restrictions is concerning, as it indicates a growing propensity for violent and aggressive behavior within the community. The COVID-19 restrictions imposed a significant economic burden on many of Sri Lanka’s lower socioeconomic classes, particularly small-scale business enterprises and daily wage workers [65]. While no comprehensive study is available, an uptick in drug-related and property crimes during the pandemic has been reported [66]. The sole case of ligature strangulation homicide and many of the sharp weapon trauma homicides in our study occurred in the context of burglary or mugging, further substantiating this concern.
- The majority of immersion fatalities during the COVID-19 restrictions were accidental. Interestingly, studies have reported an increase in unintentional drowning deaths during the COVID-19 pandemic [67]. This increase has been attributed to a higher participation in water-based recreational activities, which are seen as leisure activities where social distancing can be maintained. In the communities we studied, many households are situated near water sources, which families use for daily tasks such as washing and bathing. The high number of accidental immersion fatalities among males possibly reflects the frequent use of these water sources while under the influence of alcohol or drugs during the COVID-19 restrictions.
- The Impact of COVID-19 on Deaths due to Natural Causes
- The rise in monthly mortality rates from various natural causes reflects a hesitancy to seek hospital care for acute cardiovascular and cerebrovascular conditions, respiratory and neurological conditions, and malignancies, as documented in numerous studies [68–71]. Certain studies have identified a significant decrease in “discretionary” admissions related to cardiovascular disease, such as those for unstable angina, heart failure, chronic obstructive pulmonary disease, and dizziness/syncope. However, these studies also found that admissions for strokes and heart attacks remained constant [72]. This pattern was evident in our cohort, with family members recounting multiple instances where the deceased had ignored non-specific symptoms like chest pain or headaches in the days leading up to their death. During the COVID-19 restrictions, the DFMT observed a high frequency of myocardial rupture cases following acute myocardial infarction among sudden at-home deaths, further substantiating this trend of avoiding emergency care during the COVID-19 pandemic.
- Sri Lanka primarily operates a state-sponsored allopathic healthcare service, which is freely available to all citizens. This is supplemented by private healthcare, consisting of major private hospitals primarily located in metropolitan areas, as well as numerous private general practitioners who provide outpatient treatment in both suburban and rural regions of the country [73]. During the initial phase of the COVID-19 pandemic, state health authorities repurposed many regional hospitals to accommodate the isolation and treatment of COVID-19 patients [74]. Many routine clinics and follow-up centers were unable to operate as usual during this period. Consequently, many patients with noncommunicable diseases and those requiring surgical follow-up received their routine medication without the usual clinical assessments [75]. Some units implemented telephone consultations to reduce hospital attendance [76]. Many patients with long-term, noncommunicable diseases chose to avoid their usual clinic follow-ups. Clinic records provided by the family members of those who passed away during this period revealed that, although these patients had received their usual medications, they had not been seen or evaluated by any medical personnel for many months before their death.
- Sudden, unexpected deaths were also observed among those who had sought hospital care. During the pandemic, hospital authorities faced significant challenges in maintaining continuous service provision [77,78]. To minimize transmission of COVID-19, healthcare staff were strategically scheduled, resulting in many units operating below optimal capacity. All incoming patients were initially screened for COVID-19, and those testing positive were transferred to quarantine units. These procedures inevitably led to delays in initiating acute management, postponements in investigations, a shortage of specialist staff, and extended emergency response times, as evidenced in the medical records of some hospital deaths.
- Analysis of Deaths due to COVID-19
- In this study, we observed a higher proportion of COVID-19-related deaths among females compared to males. In contrast, many studies have reported that males had a higher risk of mortality [79], despite the higher number of infected females [80]. The reason for our finding is unclear, although it could reflect gender disparities in healthcare accessibility. Interestingly, a higher percentage of females had not received the COVID-19 vaccine. Although the difference was not statistically significant, the highest proportion of COVID-19 deaths occurred among unvaccinated females. This gender discrepancy in COVID-19 vaccination is a global trend, with females showing lower intent and acceptance of the vaccines [81]. Regrettably, we lacked reliable data to determine whether this trend was also present in the Sri Lankan context.
- The Impact of COVID-19 Vaccination on Excess Mortality
- The frequency of COVID-19-related deaths in our cohort aligned with national death rates, with the highest proportion occurring in August. Nearly one-third of those who died from COVID-19 had received at least 1 dose of the vaccine. However, we did not have data regarding the interval between vaccination and death, preventing us from establishing a clear link with vaccine efficacy. Despite reports of breakthrough COVID-19 infections post-vaccination, substantial evidence supports a decrease in hospitalization and mortality rates among vaccinated individuals [82–84]. Consistent with this, our study also found a higher proportion of COVID-19-related deaths among the unvaccinated group, further reinforcing the life-saving potential of COVID-19 vaccination.
- The question of whether COVID-19 vaccination leads to increased mortality rates from other causes has been explored. The consensus is that there has been no rise in overall mortality among those who have been vaccinated [85,86]. However, given that 80% of the vaccinations in our study involved the Sinopharm vaccine, the applicability of our findings to these studies may be limited. In our cohort, a significantly higher proportion of vaccinated males died from cardiovascular causes compared to the unvaccinated group. Likewise, while the proportion of vaccinated females who died from cardiovascular causes was lower than that of unvaccinated females, the median age in the vaccinated group was notably lower. These findings necessitate further investigation in a larger population with more rigorous case selection to evaluate any potential association between COVID-19 vaccination and cardiovascular mortality. We observed no significant differences in any other non-COVID-19 categories of natural deaths in relation to COVID-19 vaccination, nor did we record any deaths directly attributable to the vaccination.
- Limitations of the Study
- This study examined mortality trends over the past 4 years, providing a comparative analysis of deaths before, during, and after the COVID-19 pandemic. The data collected were derived from post-mortem registers and autopsy reports. The primary limitation of this study was data availability, particularly concerning vaccination history. Additionally, the number of cases within certain broad death categories was too small to provide reliable analysis. In the early stages of the pandemic, many families were hesitant to disclose any history of contact with COVID-19 or recent respiratory illnesses. This reluctance likely impacted the accuracy of COVID-19 death diagnoses at autopsy. It is also plausible that the composition of these communities may have changed during the COVID-19 restrictions due to various social and occupational factors. The pandemic’s disruption of administrative, health, and judicial services may have influenced decisions to refer deaths for autopsy. These changes would not be reflected in the study's results. Another potential limitation is the subjectivity involved in determining causes of death. However, since most cases were discussed and reviewed among departmental specialists, this bias is likely minimal.
Discussion
- This retrospective analysis examined mortality trends within a specific urban community in Sri Lanka across 3 periods related to the COVID-19 pandemic. During the community’s COVID-19 lockdown, there was an increased fatality rate from various chronic natural conditions. This increase predominantly affected highly urbanized, densely populated communities where COVID-19 restrictions were consistently and stringently enforced. In contrast, unnatural deaths presented a mixed picture. There was a decrease in fatalities from traffic accidents, firearm incidents, suicides by hanging, and poisonings. However, there was also an uptick in deaths resulting from blunt trauma, sharp weapon homicides, and drownings. COVID-19-related deaths peaked approximately 6 months after the vaccination program’s initiation. The majority of these deaths were among individuals over 65, those who were not vaccinated, and females. Aside from a significantly higher proportion of cardiovascular deaths among vaccinated males, and a non-significantly higher proportion of COVID-19 deaths among non-vaccinated females, there were no other discernible differences in mortality trends between the vaccinated and non-vaccinated groups.
Conclusion
- • The mortality rates of natural categories of death increased during the coronavirus disease 2019 (COVID-19) restrictions, indicating disruptions to health care.
- • A significantly higher percentage of females died during the period of lockdown, and the majority of COVID-19 deaths were in females.
- • Higher frequencies of blunt homicides and femicides reflect interpersonal conflicts and domestic violence during the COVID-19 pandemic.
- • Deaths due to COVID-19 were seen mostly among residents in overcrowded, urban communities and in those who were not vaccinated.
HIGHLIGHTS
-
Ethics Approval
This study was granted ethics approval from the Ethics Review Committee of the Faculty of Medicine, University of Colombo under EC-21-055.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets generated during and/or analyzed during the current study are not publicly available due to them being related to forensic death investigations but are available from the corresponding author on reasonable request.
-
Authors’ Contributions
Conceptualization: SAG; Data curation: ND, SK, BIK, HR; Formal analysis: SAG, JWG; Methodology: SAG; Project administration: ND, SK; Resources: ND, HR, SK, JWG; Supervision: SAG; Writing–original draft: SAG, SK, BIK, JWG; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Additional Contributions
We would like to acknowledge Dr Kiritharan Kasilingam, Dr Naveen Wijeweera, Dr Dinesh Pieris, Ms Wasundara Jayawardena for their assistance in data acquisition; Mr Sithija Kesara Gunawardena for assistance in formatting and design of figures and tables; and members of the academic and non-academic staff of the Department of Forensic Medicine & Toxicology of the Faculty of Medicine, University of Colombo for their contributions in providing data for the study.
Article information


| Causes of natural and unnatural deaths |
Male |
Female |
||||
|---|---|---|---|---|---|---|
| Pre-COVID-19 | COVID-19 | Post-COVID-19 | Pre-COVID-19 | COVID-19 | Post-COVID-19 | |
| Natural (n=1,522) | 257 | 503 | 211a) | 93 | 374 | 84a) |
| Median age (y) | 66 (55–76) | |||||
| Cardiovascular diseases (n=741) | 156 (60.7) | 253 (50.3) | 99 (46.9) | 42 (45.2) | 162 (43.3) | 29 (34.5) |
| Infection (n=254) | 47 (18.3) | 67 (13.3) | 45 (21.3) | 21 (22.6) | 43 (11.5) | 31 (36.9) |
| COVID-19 (n=188) | 0 (0) | 76 (15.1) | 10 (4.7) | 0 (0) | 96 (25.7) | 6 (7.1) |
| Cerebrovascular disease (n=98) | 16 (6.2) | 25 (5.0) | 17 (8.1) | 9 (9.7) | 26 (7.0) | 5 (6.0) |
| Chronic lung disease (n=59) | 9 (3.5) | 23 (4.6) | 17 (8.1) | 1 (1.1) | 7 (1.9) | 2 (2.4) |
| Other (n=62) | 10 (3.9) | 15 (3.0) | 8 (3.8) | 8 (8.6) | 17 (4.5) | 4 (4.8) |
| Malignancy (n=39) | 5 (1.9) | 15 (3.0) | 5 (2.4) | 3 (3.2) | 8 (2.1) | 3 (3.6) |
| Chronic liver disease (n=25) | 5 (1.9) | 14 (2.8) | 2 (0.9) | 0 (0) | 4 (1.1) | 0 (0) |
| Diabetic complications (n=22) | 3 (1.2) | 8 (1.6) | 1 (0.5) | 1 (1.1) | 8 (2.1) | 1 (1.2) |
| Chronic kidney disease (n=15) | 2 (0.8) | 7 (1.4) | 1 (0.5) | 1 (1.1) | 3 (0.8) | 1 (1.2) |
| Venous thrombosis (n=14) | 4 (1.6) | 0 (0) | 3 (1.4) | 7 (7.5) | 0 (0) | 0 (0) |
| Accidents (n=303) | 82 | 113 | 64 | 16 | 21 | 7 |
| Median age (y) | 55 (39-68) | |||||
| Traffic fatality (n=155) | 57 (69.5) | 48 (42.5) | 30 (46.9) | 10 (62.5) | 6 (28.6) | 4 (57.1) |
| Blunt trauma (n=92) | 16 (19.5) | 41 (36.3) | 22 (34.4) | 2 (12.5) | 9 (42.9) | 2 (28.6) |
| Immersion deaths (Drowning) (n=28) | 4 (4.9) | 16 (14.2) | 5 (7.8) | 2 (12.5) | 1 (4.8) | 0 (0) |
| Electrocution (n=12) | 4 (4.9) | 4 (3.5) | 4 (6.3) | 0 (0) | 0 (0) | 0 (0) |
| Burns (n=8) | 0 (0) | 2 (1.8) | 1 (1.6) | 1 (6.3) | 3 (14.3) | 1 (14.3) |
| Asphyxiation (n=6) | 1 (1.2) | 2 (1.8) | 1 (1.6) | 1 (6.3) | 1 (4.8) | 0 (0) |
| Poisoning & drug overuse (n=1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4.8) | 0 (0) |
| Suicides (n=163) | 47 | 41 | 38 | 13 | 17 | 7 |
| Median age (y) | 39 (28-54) | |||||
| Asphyxiation (Hanging) (n=123) | 38 (80.9) | 34 (82.9) | 33 (86.8) | 7 (53.8) | 7 (41.2) | 4 (57.1) |
| Burns (n=19) | 1 (2.1) | 3 (7.3) | 2 (5.3) | 4 (30.8) | 6 (35.3) | 3 (42.9) |
| Poisoning & drug overuse (n=15) | 6 (12.8) | 3 (7.3) | 2 (5.3) | 1 (7.7) | 3 (17.6) | 0 (0) |
| Immersion deaths (drowning) (n=4) | 1 (2.1) | 0 (0) | 1 (2.6) | 1 (7.7) | 1 (5.9) | 0 (0) |
| Sharp trauma (n=1) | 0 (0) | 1 (2.4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Traffic fatality (n=1) | 1 (2.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Homicides (n=34) | 8 | 10 | 10 | 0 (0) | 5 | 1 |
| Median age (y) | 39 (29-55) | |||||
| Sharp trauma (n=18) | 4 (50.0) | 3 (30.0) | 9 (90.0) | 0 (0) | 2 (40.0) | 0 (0) |
| Firearm deaths (v=7) | 4 (50.0) | 2 (20.0) | 1 (10.0) | 0 (0) | 0 (0) | 0 (0) |
| Blunt trauma (n=7) | 0 (0) | 5 (50.0) | 0 (0) | 0 (0) | 2 (40.0) | 0 (0) |
| Asphyxiation (ligature strangulation) (n=1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (100.0) |
| Immersion deaths (n=1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (20.0) | 0 (0) |
| Total | 394 (19.5) | 667 (33.0) | 323 (16.0) | 122 (6.0) | 417 (20.6) | 99 (4.9) |
| Broad categories of natural deaths among deceased persons with vaccination details (n=657)a) | Vaccinated males | Non-vaccinated males | Vaccinated females | Non-vaccinated females |
|---|---|---|---|---|
| Cardiovascular disease | ||||
| Total (281, 42.8%) | 131 | 50 | 44 | 56 |
| Median age (y) | 64.5 (55.0–73.0) | 64.0 (56.5–75.5) | 69.5 (55.0–79.0) | 81.5 (69.0–87.0) |
| COVID-19 deaths | ||||
| Total (145, 22.1%) | 29 | 36 | 27 | 53 |
| Median age (y) | 73.0 (66.5–82.5) | 69.5 (53.0–79.5) | 77.0 (69.0–85.0) | 78.0 (57.5–88.0) |
| Infections | ||||
| Total (93, 14.2%) | 28 | 28 | 22 | 15 |
| Median age (y) | 62.5 (52.0–75.0) | 62.5 (57.5–82.0) | 70.0 (57.0–81.0) | 72.0 (65.0–83.0) |
| Cerebrovascular disease | ||||
| Total (43, 6.5%) | 14 | 11 | 10 | 8 |
| Median age (y) | 61.5 (49.0–75.0) | 69.0 (46.0–77.0) | 72.0 (60.0–79.0) | 74.5 (65.5–85.0) |
| Chronic lung disease | ||||
| Total (23, 3.5%) | 12 | 8 | 2 | 1 |
| Median age (y) | 67.0 (56.0–72.0) | 61.5 (58.0–75.0) | 73 | - |
| Other | ||||
| Total (20, 3.0%) | 6 | 7 | 3 | 4 |
| Median age (y) | 72.0 (61.0–82.0) | 70.0 (49.0–84.0) | 66 | 72.0 (51.0–90.0) |
| Diabetic complications | ||||
| Total (16, 2.4%) | 3 | 6 | 0 | 7 |
| Median age (y) | 59 | 75.5 (67.0–84.0) | - | 70.0 (44.0–78.0) |
| Malignancy | ||||
| Total (16, 2.4%) | 5 | 4 | 1 | 6 |
| Median age (y) | 63.0 (58–66.0) | 72.0 (63.0–80.5) | 43 | 70.0 (37.0–74.0) |
| Chronic liver disease | ||||
| Total (13, 2.0%) | 7 | 6 | 0 | 0 |
| Median age (y) | 54.0 (53.0–60.0) | 43.0 (39.0–71.0) | - | - |
- 1. Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature 2020;579:265−9.ArticlePubMedPMCPDF
- 2. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270−3.PubMedPMC
- 3. Qian G, Yang N, Ma AH, et al. COVID-19 transmission within a family cluster by presymptomatic carriers in China. Clin Infect Dis 2020;71:861−2.ArticlePubMedPMCPDF
- 4. Li LQ, Huang T, Wang YQ, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol 2020;92:577−83.ArticlePubMedPMCPDF
- 5. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med 2020;9:575. ArticlePubMedPMC
- 6. World Health Organization (WHO). WHO coronavirus (COVID-19) dashboard [Internet]. WHO; 2023 [cited 2023 Oct 26]. Available from: https://covid19.who.int/.
- 7. Yu X, Yang R. COVID-19 transmission through asymptomatic carriers is a challenge to containment. Influenza Other Respir Viruses 2020;14:474−5.ArticlePubMedPMCPDF
- 8. Samui P, Mondal J, Khajanchi S. A mathematical model for COVID-19 transmission dynamics with a case study of India. Chaos Solitons Fractals 2020;140:110173. ArticlePubMedPMC
- 9. Jebril N. World Health Organization declared a pandemic public health menace: a systematic review of the coronavirus disease 2019 “COVID-19” [Internet]. SSRN; 2020 [cited 2023 Oct 26]. Available from: https://ssrn.com/abstract=3566298.
- 10. ColomboPage. National Action Committee on President’s Advice to prevent spread of deadly coronavirus [Internet]. ColomboPage; 2020 [cited 2023 Oct 26]. Available from: http://www.colombopage.com/archive_20A/Jan26_1580061672CH.php.
- 11. Hettiarachchi D, Noordeen N, Gamakaranage C, et al. Ethical responses to the COVID-19 pandemic-lessons from Sri Lanka. Asian Bioeth Rev 2020;13:225−33.ArticlePubMedPMCPDF
- 12. Department of Government Information. Press release 2020.03.20: Declaration of police curfew islandwide [Internet]. Department Of Government Information; 2020 [cited 2021 Feb 22]. Available from: https://www.dgi.gov.lk/news/press-releases-sri-lanka/1956-press-release-2020-03-22.
- 13. Economynext. First coronavirus patient dies in Sri Lanka, total COVID-19 count 113 [Internet]. Economynext; 2020 [cited 2021 Feb 22]. Available from: https://economynext.com/first-coronavirus-patient-dies-in-sri-lanka-total-covid-19-count-113-62718/.
- 14. Department of Government Information. Press release 2020.05.25. A 51 years old woman has died suddnley at Trincomalee quarantine center [Internet]. Department Of Government Information; 2020 [cited 2023 Oct 26]. Available from: https://www.dgi.gov.lk/news/press-releases-sri-lanka/2022-press-release-2020-05-25-a-51-years-old-woman-has-died-suddnley-at-trincomalee-quarantine-center.
- 15. Farzan Z. 4000 sailors and their families quarantine at Welisara Navy Camp [Internet]. News First; 2020 [cited 2021 Feb 22]. Available from: https://www.newsfirst.lk/2020/04/24/4000-sailors-and-their-families-quarantine-at-welisara-navy-camp/.
- 16. Epidemiology Unit, Ministry of Health. Coronavirus disease 2019 (COVID-19): situation report 30.07.2020. Epidemiology Unit, Ministry of Health; 2020.
- 17. Epidemiology Unit, Ministry of Health. Coronavirus disease 2019 (COVID-19): situation report 15.04.2020. Epidemiology Unit, Ministry of Health; 2020.
- 18. Registrar General’s Department. Circulars [Internet]. Registrar General’s Department; 2023 [cited 2023 May 3]. Available from: https://www.rgd.gov.lk/web/index.php/en/downloads/circulars.html#2020.
- 19. Epidemiology Unit, Ministry of Health. Coronavirus disease 2019 (COVID-19): situation report 01.01.2021 - 10 a.m. [Internet]. Epidemiology Unit, Ministry of Health; 2021 [cited 2023 May 3]. Available from: https://www.epid.gov.lk/epid/public/storage/post/pdfs/en_640019ec6ffe4_sitrep-sl-en-01-01_10.pdf.
- 20. Epidemiology Unit, Ministry of Health. Coronavirus disease 2019 (COVID-19): situation report 01.07.2021 - 10 a.m. [Internet]. Epidemiology Unit, Ministry of Health; 2021 [cited 2023 May 3]. Available from: https://www.epid.gov.lk/epid/public/storage/post/pdfs/en_63ff3febace7d_sitrep-sl-en-01-07_10_21.pdf.
- 21. Epidemiology Unit, Ministry of Health. Coronavirus disease 2019 (COVID-19): situation report -06.09.2021- 10 a.m. [Internet]. Epidemiology Unit, Ministry of Health; 2021 [cited 2023 May 3]. Available from: https://www.epid.gov.lk/epid/public/storage/post/pdfs/en_63ff1e0b4323b_sitrep-sl-en-06-09_10_21_1.pdf.
- 22. Rajapaksa LC, De Silva P, Abeykoon P. COVID-19 health system response monitor: Sri Lanka [Internet]. World Health Organization; 2022 [cited 2023 May 5]. Available from: https://policycommons.net/artifacts/2233422/covid-19-health-system-response-monitor/2991353/.
- 23. Presidential Secretariat. Inter-provincial travel restrictions will be lifted on 31st [Internet]. Presidential Secretariat; 2021 [cited 2023 May 5]. Available from: https://www.presidentsoffice.gov.lk/index.php/2021/10/29/inter-provincial-travel-restrictions-will-be-lifted-on-31st/.
- 24. Baig AS, Butt HA, Haroon O, et al. Deaths, panic, lockdowns and US equity markets: the case of COVID-19 pandemic. Financ Res Lett 2021;38:101701. ArticlePubMed
- 25. Sotgiu G, Dobler CC. Social stigma in the time of coronavirus disease 2019. Eur Respir J 2020;56:2002461. ArticlePubMedPMC
- 26. Freckelton Qc I. COVID-19: fear, quackery, false representations and the law. Int J Law Psychiatry 2020;72:101611. ArticlePubMedPMC
- 27. van Mulukom V, Pummerer LJ, Alper S, et al. Antecedents and consequences of COVID-19 conspiracy beliefs: a systematic review. Soc Sci Med 2022;301:114912. ArticlePubMedPMC
- 28. Marsoof A. The constitutionality of forced cremations of COVID-19 victims in Sri Lanka [Internet]. People’s Rights Group of Sri Lanka; 2020 [cited 2023 Oct 26]. Available from: https://www.prgsrilanka.org/the-constitutionality-of-forced-cremations-of-covid-19-victims-in-sri-lanka/.
- 29. College of Community Physicians of Sri Lanka. Debate about compulsory cremation of victims of COVID-19. J Coll Community Physicians Sri Lanka 2020;26:193−6.Article
- 30. Abdul Razak MI, Mohamed Saleem A. COVID-19: the crossroads for Sinhala-Muslim relations in Sri Lanka. J Asian Afr Stud 2021;57:529−42.ArticlePDF
- 31. Wijesinghe MS, Ariyaratne VS, Gunawardana BM, et al. Role of religious leaders in COVID-19 prevention: a community-level prevention model in Sri Lanka. J Relig Health 2022;61:687−702.ArticlePubMedPDF
- 32. Rossen LM, Branum AM, Ahmad FB, et al. Excess deaths associated with COVID-19, by age and race and ethnicity: United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1522−7.ArticlePubMedPMC
- 33. Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA 2021;325:1786−9.ArticlePubMedPMC
- 34. Wadhera RK, Shen C, Gondi S, et al. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol 2021;77:159−69.ArticlePubMedPMC
- 35. Islam N, Shkolnikov VM, Acosta RJ, et al. Excess deaths associated with COVID-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ 2021;373:n1137. ArticlePubMed
- 36. Khan MM, Khan MN, Mustagir MG, et al. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: a systematic review and meta-analysis. J Glob Health 2020;10:020503. ArticlePubMedPMC
- 37. Mannucci E, Nreu B, Monami M. Factors associated with increased all-cause mortality during the COVID-19 pandemic in Italy. Int J Infect Dis 2020;98:121−4.ArticlePubMedPMC
- 38. Stokes AC, Lundberg DJ, Elo IT, et al. COVID-19 and excess mortality in the United States: a county-level analysis. PLoS Med 2021;18:e1003571.ArticlePubMedPMC
- 39. Davies B, Parkes BL, Bennett J, et al. Community factors and excess mortality in first wave of the COVID-19 pandemic in England. Nat Commun 2021;12:3755. ArticlePubMedPMCPDF
- 40. Mazza M, Marano G, Lai C, et al. Danger in danger: interpersonal violence during COVID-19 quarantine. Psychiatry Res 2020;289:113046. ArticlePubMedPMC
- 41. Humphreys KL, Myint MT, Zeanah CH. Increased risk for family violence during the COVID-19 pandemic. Pediatrics 2020;146:e20200982.ArticlePubMedPDF
- 42. Uzobo E, Ayinmoro AD. Trapped between two pandemics: domestic violence cases under COVID-19 pandemic lockdown: a scoping review. Community Health Equity Res Policy 2023;43:319−28.ArticlePubMedPDF
- 43. Department of Census and Statistics, Ministry of Economic Policies and Plan Implementation. Grama Niladhari Divisions Statistics-2020: Colombo district [Internet]. Department of Census and Statistics; 2021 [cited 2023 Oct 26].Available from: http://www.statistics.gov.lk/Population/StaticalInformation/GND_Reports/2020/Colombo.
- 44. Simba H, Ngcobo S. Are pandemics gender neutral?: women’s health and COVID-19. Front Glob Womens Health 2020;1:570666. ArticlePubMedPMC
- 45. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the COVID-19 pandemic: a review. Soc Sci Med 2020;266:113364. ArticlePubMedPMC
- 46. McLaren HJ, Wong KR, Nguyen KN, et al. COVID-19 and women’s triple burden: vignettes from Sri Lanka, Malaysia, Vietnam and Australia. Soc Sci 2020;9:87. Article
- 47. Piquero AR, Jennings WG, Jemison E, et al. Domestic violence during the COVID-19 pandemic: evidence from a systematic review and meta-analysis. J Crim Justice 2021;74:101806. ArticlePubMedPMC
- 48. Kourti A, Stavridou A, Panagouli E, et al. Domestic violence during the COVID-19 pandemic: a systematic review. Trauma Violence Abuse 2023;24:719−45.ArticlePubMedPDF
- 49. World Vision Sri Lanka. COVID-19 global health emergency response in Sri Lanka: keeping our children and communities safe [Internet]. World Vision Sri Lanka; 2020 [cited 2023 Apr 28]. Available from: https://www.wvi.org/covid-19-response-srilanka.
- 50. Jayatissa R, Herath HP, Perera AG, et al. Impact of COVID-19 on child malnutrition, obesity in women and household food insecurity in underserved urban settlements in Sri Lanka: a prospective follow-up study. Public Health Nutr 2021;24:3233−41.ArticlePubMed
- 51. Sakelliadis EI, Katsos KD, Zouzia EI, et al. Impact of COVID-19 lockdown on characteristics of autopsy cases in Greece: comparison between 2019 and 2020. Forensic Sci Int 2020;313:110365. ArticlePubMedPMC
- 52. Calderon-Anyosa RJ, Kaufman JS. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med 2021;143:106331. ArticlePubMed
- 53. Yasin YJ, Grivna M, Abu-Zidan FM. Global impact of COVID-19 pandemic on road traffic collisions. World J Emerg Surg 2021;16:51. ArticlePubMedPMCPDF
- 54. Gupta M, Pawar NM, Velaga NR. Impact of lockdown and change in mobility patterns on road fatalities during COVID-19 pandemic. Transp Lett 2021;13:447−60.Article
- 55. Redelmeier DA, Zipursky JS. Pedestrian deaths during the COVID-19 pandemic. Am J Lifestyle Med 2021;17:276−9.ArticlePubMedPMCPDF
- 56. Jordans MJ, Kaufman A, Brenman NF, et al. Suicide in South Asia: a scoping review. BMC Psychiatry 2014;14:358. ArticlePubMedPMCPDF
- 57. Knipe DW, Padmanathan P, Muthuwatta L, et al. Regional variation in suicide rates in Sri Lanka between 1955 and 2011: a spatial and temporal analysis. BMC Public Health 2017;17:193. ArticlePubMedPMCPDF
- 58. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM 2020;113:707−12.ArticlePubMedPDF
- 59. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020;7:468−71.ArticlePubMedPMC
- 60. McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res 2020;290:113104. ArticlePubMedPMC
- 61. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav 2021;5:229−38.ArticlePubMedPDF
- 62. Appleby L. What has been the effect of COVID-19 on suicide rates? BMJ 2021;372:n834. ArticlePubMed
- 63. Rajapakse T, Silva T, Hettiarachchi NM, et al. The impact of the COVID-19 pandemic and lockdowns on self-poisoning and suicide in Sri Lanka: an interrupted time series analysis. Int J Environ Res Public Health 2023;20:1833. ArticlePubMedPMC
- 64. Edirisinghe PA, Kitulwatte ID. Extreme violence: homicide; an analysis of 265 cases from the offices of JMO Colombo and Ragama: a study from Sri Lanka. Leg Med (Tokyo) 2009;11 Suppl 1:S363−5.ArticlePubMed
- 65. Robinson J, Kengatharan N. Exploring the effect of COVId-19 on small and medium enterprises: early evidence from Sri Lanka. J Appl Econ Bus Res 2020;10:115−25.
- 66. Imalka DD, Wijewardhana BV. A criminological study on crimes in the Western province of Sri Lanka, during the COVID 19 lockdown period. Vidyodaya J Humanit Soc Sci 2022;7:207−22.Article
- 67. Moreland B, Ortmann N, Clemens T. Increased unintentional drowning deaths in 2020 by age, race/ethnicity, sex, and location, United States. J Safety Res 2022;82:463−8.ArticlePubMedPMC
- 68. Bodilsen J, Nielsen PB, Sogaard M, et al. Hospital admission and mortality rates for non-covid diseases in Denmark during COVID-19 pandemic: nationwide population based cohort study. BMJ 2021;373:n1135. ArticlePubMed
- 69. Blecker S, Jones SA, Petrilli CM, et al. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern Med 2021;181:269−71.ArticlePubMed
- 70. Bhambhvani HP, Rodrigues AJ, Yu JS, et al. Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern Med 2021;181:272−4.ArticlePubMed
- 71. Gadsden T, Downey LE, Vilas VD, et al. The impact of COVID-19 on essential health service provision for noncommunicable diseases in the South-East Asia region: a systematic review. Lancet Reg Health Southeast Asia 2022;1:100010. ArticlePubMedPMC
- 72. Stohr E, Aksoy A, Campbell M, et al. Hospital admissions during COVID-19 lock-down in Germany: differences in discretionary and unavoidable cardiovascular events. PLoS One 2020;15:e0242653.ArticlePubMedPMC
- 73. World Health Organization (WHO), Alliance for Health Policy and Systems Research. Primary health care systems (primasys): case study from Sri Lanka [Internet]. WHO; 2017 [cited 2023 Oct 26]. Available from: https://iris.who.int/handle/10665/341087.
- 74. Wickramasinghe D, Fernando VK. Sri Lanka’s fight against COVID-19: a brief overview. Edited by Shaw R, Pal I: Pandemic risk, response, and resilience: COVID-19 responses in cities around the world. Elsevier; 2022. pp 129−42.
- 75. Samarathunga DR, Gamage RT, Wickramarachchi WA, et al. The response to COVID 19: a journal of the initial institutional experience of general surgical units at the National Hospital of Sri Lanka, Colombo. Sri Lanka J Surg 2020;38:46−53.Article
- 76. Hewamana S, Skandarajah T, Jayasinghe C, et al. Blood cancer care in a resource limited setting during the COVID-19 outbreak; a single center experience from Sri Lanka. PLoS One 2021;16:e0256941.ArticlePubMedPMC
- 77. Perera B, Wickramarachchi B, Samanmalie C, et al. Psychological experiences of healthcare professionals in Sri Lanka during COVID-19. BMC Psychol 2021;9:49. ArticlePubMedPMCPDF
- 78. Kumanan T, Rajasooriyar C, Guruparan M, et al. The impact of COVID-19 on the delivery of critical health care: experience from a non-high-income country. Asia Pac J Public Health 2020;32:473−5.ArticlePubMedPDF
- 79. Ya’qoub L, Elgendy IY, Pepine CJ. Sex and gender differences in COVID-19: more to be learned! Am Heart J Plus 2021;3:100011. ArticlePubMedPMC
- 80. Ramirez-Soto MC, Ortega-Caceres G, Arroyo-Hernandez H. Sex differences in COVID-19 fatality rate and risk of death: an analysis in 73 countries, 2020-2021. Infez Med 2021;29:402−7.ArticlePubMedPMC
- 81. Zintel S, Flock C, Arbogast AL, et al. Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis. Z Gesundh Wiss 2023;31:1303−27.ArticlePDF
- 82. Tenforde MW, Self WH, Adams K, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA 2021;326:2043−54.PubMed
- 83. Christie A, Henley SJ, Mattocks L, et al. Decreases in COVID-19 cases, emergency department visits, hospital admissions, and deaths among older adults following the introduction of COVID-19 vaccine: United States, September 6, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep 2021;70:858−64.ArticlePubMedPMC
- 84. He G, Zhu S, Fu D, et al. Association between COVID-19 vaccination coverage and case fatality ratio: a comparative study: Hong Kong SAR, China and Singapore, December 2021-March 2022. China CDC Wkly 2022;4:649−54.PubMedPMC
- 85. Lamptey E. Post-vaccination COVID-19 deaths: a review of available evidence and recommendations for the global population. Clin Exp Vaccine Res 2021;10:264−75.ArticlePubMedPMCPDF
- 86. Sessa F, Salerno M, Esposito M, et al. Autopsy findings and causality relationship between death and COVID-19 vaccination: a systematic review. J Clin Med 2021;10:5876. ArticlePubMedPMC
References
Figure & Data
References
Citations




 Cite
Cite