Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(3); 2023 > Article
-
Original Article
The COVID-19 pandemic and healthcare utilization in Iran: evidence from an interrupted time series analysis -
Monireh Mahmoodpour-Azari1
 , Satar Rezaei1
, Satar Rezaei1 , Nasim Badiee2,3
, Nasim Badiee2,3 , Mohammad Hajizadeh4
, Mohammad Hajizadeh4 , Ali Mohammadi5
, Ali Mohammadi5 , Ali Kazemi-Karyani1
, Ali Kazemi-Karyani1 , Shahin Soltani1
, Shahin Soltani1 , Mehdi Khezeli6
, Mehdi Khezeli6
-
Osong Public Health and Research Perspectives 2023;14(3):180-187.
DOI: https://doi.org/10.24171/j.phrp.2023.0041
Published online: June 22, 2023
1Research Center for Environmental Determinants of Health, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran
2Institute for Studies in Medicine History, Persian and Complementary Medicine, Iran University of Medical Sciences, Tehran, Iran
3Department of Traditional Medicine, School of Persian Medicine, Iran University of Medical Sciences, Tehran, Iran
4School of Health Administration, Faculty of Health, Dalhousie University, Halifax, NS, Canada
5Department of Health Information Technology, Paramedical School, Kermanshah University of Medical Sciences, Kermanshah, Iran
6Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran
- Corresponding author: Satar Rezaei Research Center for Environmental Determinants of Health, Health Institute, Kermanshah University of Medical Sciences, Isar Sq., across from Farabi Hospital, Kermanshah 6719851351, Iran E-mail: satarrezaei@gmail.com
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,371 Views
- 66 Download
Abstract
-
Objectives
- This study aimed to examine the effect of the coronavirus disease 2019 (COVID-19) outbreak on the hospitalization rate, emergency department (ED) visits, and outpatient clinic visits in western Iran.
-
Methods
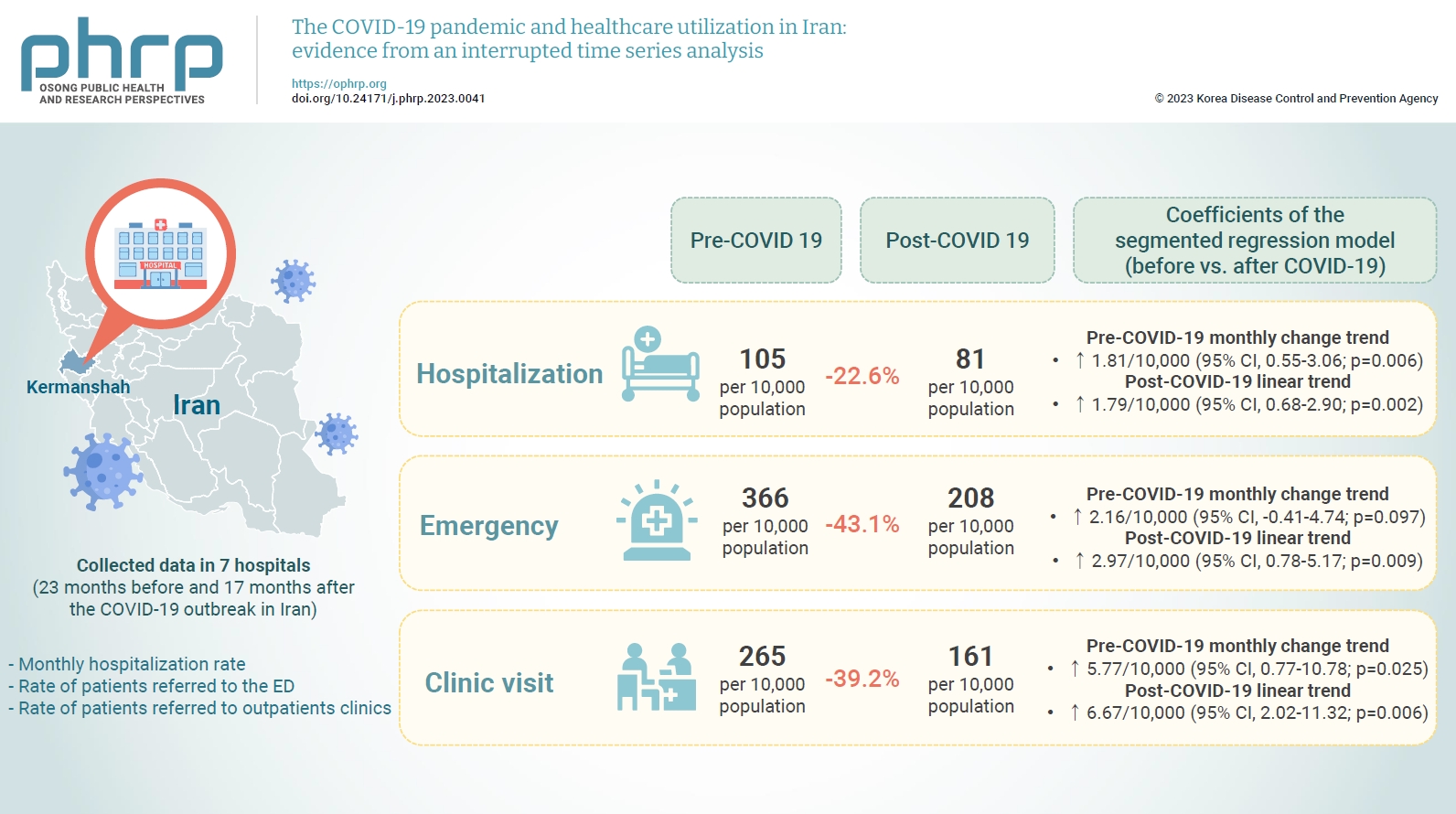
- We collected data on the monthly hospitalization rate, rate of patients referred to the ED, and rate of patients referred to outpatient clinics for a period of 40 months (23 months before and 17 months after the COVID-19 outbreak in Iran) from all 7 public hospitals in the city of Kermanshah. An interrupted time series analysis was conducted to examine the impact of COVID-19 on the outcome variables in this study.
-
Results
- A statistically significant decrease of 38.11 hospitalizations per 10,000 population (95% confidence interval [CI], 24.93–51.29) was observed in the first month of the COVID-19 outbreak. The corresponding reductions in ED visits and outpatient visits per 10,000 population were 191.65 (95% CI, 166.63–216.66) and 168.57 (95% CI, 126.41–210.73), respectively. After the initial reduction, significant monthly increases in the hospitalization rate (an increase of 1.81 per 10,000 population), ED visits (an increase of 2.16 per 10,000 population), and outpatient clinic visits (an increase of 5.77 per 10,000 population) were observed during the COVID-19 pandemic.
-
Conclusion
- Our study showed that the utilization of outpatient and inpatient services in hospitals and clinics significantly declined after the COVID-19 outbreak, and use of these services did not return to pre-outbreak levels as of June 2021.
- The emergence and spread of coronavirus disease 2019 (COVID-19) has challenged and disrupted the functioning of healthcare systems worldwide. Countries have been forced to take swift action to counter the rapid spread of the virus while maintaining the integrity of their health systems [1]. Hospitals have been forced to re-evaluate care and treatment priorities due to the referral and management of new patients infected with COVID-19 in response to the community’s ongoing needs and medical care. During this period, major changes in the provision of non-emergency and elective care in hospitals, outpatient wards, clinics, and surgical centers have also occurred [2]. In particular, strict measures have been taken to control the pandemic worldwide, and healthcare systems have been reorganized to manage the sudden increase in the number of patients infected with the virus [3].
- The outbreak of COVID-19 in Iran began on February 19, 2020, following the official announcement of the first 2 cases of COVID-19 in the city of Qom. The virus quickly spread to all provinces of Iran [4]. The spread of COVID-19 and the presence of new coronavirus variants led to high utilization of hospital care, particularly among those with underlying diseases [5]. The most important measures taken by the Iranian government to prevent the spread of COVID-19 were an emphasis on physical distancing, quarantine policies, the control and restriction of travel, restrictions on gatherings, and an increase in the number of hospital beds to isolate COVID-19 patients [6]. As the pandemic continued, several studies reported reduced utilization of healthcare services for reasons that included fear of becoming infected at healthcare facilities, reduced access to healthcare centers due to quarantine or reductions in elective surgery, and the need to separate patients seeking urgent and necessary care from other patients [7]. For example, a study in France reported 68% and 45% reductions in pediatric emergency department (ED) referrals and hospital admissions, respectively [8]. A study in Italy showed a 48.8% reduction in referrals of patients with acute myocardial infarction [9]. A 42% reduction in ED visits was reported in the United States [10]. This unprecedented reduction in healthcare utilization resulting from the COVID-19 pandemic provided an opportunity to identify the most low-value services in healthcare systems and redistribute resources to more essential services to minimize mortality in a crisis [7,11].
- Data analysis using an interrupted time series model makes it possible to examine the effect of the COVID-19 pandemic on the pattern of hospitalizations and outpatient visits. The aim of this study was to investigate the effect of the COVID-19 pandemic on outpatient referrals and hospitalizations in hospitals affiliated with the Ministry of Health and Medical Education (MoHME) in the city of Kermanshah. Our study provides valuable insight into the impact of COVID-19 on healthcare utilization in Iran and can be helpful for other developing countries with similar healthcare situations to mitigate the long-term and short-term impacts of the pandemic.
Introduction
- Study Setting
- This study was conducted in the city of Kermanshah, the capital of Kermanshah Province in the western region of Iran. The total populations of the city of Kermanshah and Kermanshah Province in 2015 were estimated at 1 and 2 million, respectively. The city of Kermanshah contains 7 MoHME-affiliated hospitals that are responsible for providing most healthcare services in the city.
- Data Source
- The first 2 confirmed cases of COVID-19 in Iran were reported on February 19, 2020. We collected data on the monthly hospitalization rate, rate of patients referred to the ED, and rate of patients referred to outpatient clinics for a period of 40 months (23 months before and 17 months after the COVID-19 outbreak in Iran) from the health information systems of all 7 hospitals. Population data were also extracted from the Statistics Center of Iran.
- Statistical Analysis
- We conducted an interrupted time series analysis with segmented regression [12,13] to assess the impact of the COVID-19 outbreak on the monthly hospitalization rate per 10,000 population, number of patients referred to an ED per 10,000 population, and number of patients referred to an outpatient clinic per 10,000 population at 7 MoHME-affiliated hospitals in the city of Kermanshah. The interrupted time series method can be used to estimate the impact (not just association) of an intervention on outcomes when no comparison data are available [13]. This method is especially useful when “natural experiments” occur in the real world. The main advantage of this method is that it can fully exploit the longitudinal aspect of the data. However, this approach is unsuitable when trends are not linear (or cannot be transformed to be linear) or the intervention is implemented on a step-by-step basis or at several time points [14].
- The specific segmented regression model that follows was used to estimate the effect of the COVID-19 outbreak on the monthly hospitalization rate, rate of ED visits, and number of patients referred to an outpatient clinic [15].
- where Yt denotes the number of admissions (hospitalizations, ED visits, and referrals to an outpatient clinic) in the month t, Tt is the time trend variable, which ranges in value from 1 (first observation) to 40 (last observation), Xt is a binary variable that represents before and after the outbreak (Xt =0 for before and Xt =1 for after), XtTt is coded as 0 for the period before the COVID-19 outbreak and assigned a value between 1 (first observation after the outbreak) and 17 (last observation after the outbreak) for the period after the COVID-19 outbreak, β0 indicates the starting level (intercept) of the outcome variable, β1 represents the slope of the outcome variable before the outbreak (the pre-existing trend), β2 represents the change in the value for the outcome variable immediately after the outbreak (compared to the counterfactual), and β3 represents the difference between the pre- and post-pandemic slopes of the outcome variable.
- An interrupted time series analysis was conducted using linear regression (ordinary least squares) with Newey-West errors. The Newey-West approach was used to handle autocorrelation and possible heteroscedasticity in the error term [13]. The Dickey–Fuller statistic test result suggested stationary residuals (i.e., the time series had no unit root). This indicated a normal residual distribution. The seasonality for each of the dependent variables in this study was checked using the 2-way line command. The output graphs indicated no seasonality patterns in our data (Figure S1). All data analysis was performed using Stata ver. 16.0 (StataCorp LLC).
- Ethical Approval
- This study was approved by the Deputy of Research, Kermanshah University of Medical Sciences (No. IR.KUMS.REC.1400.856), and performed in accordance with the principles of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
Materials and Methods
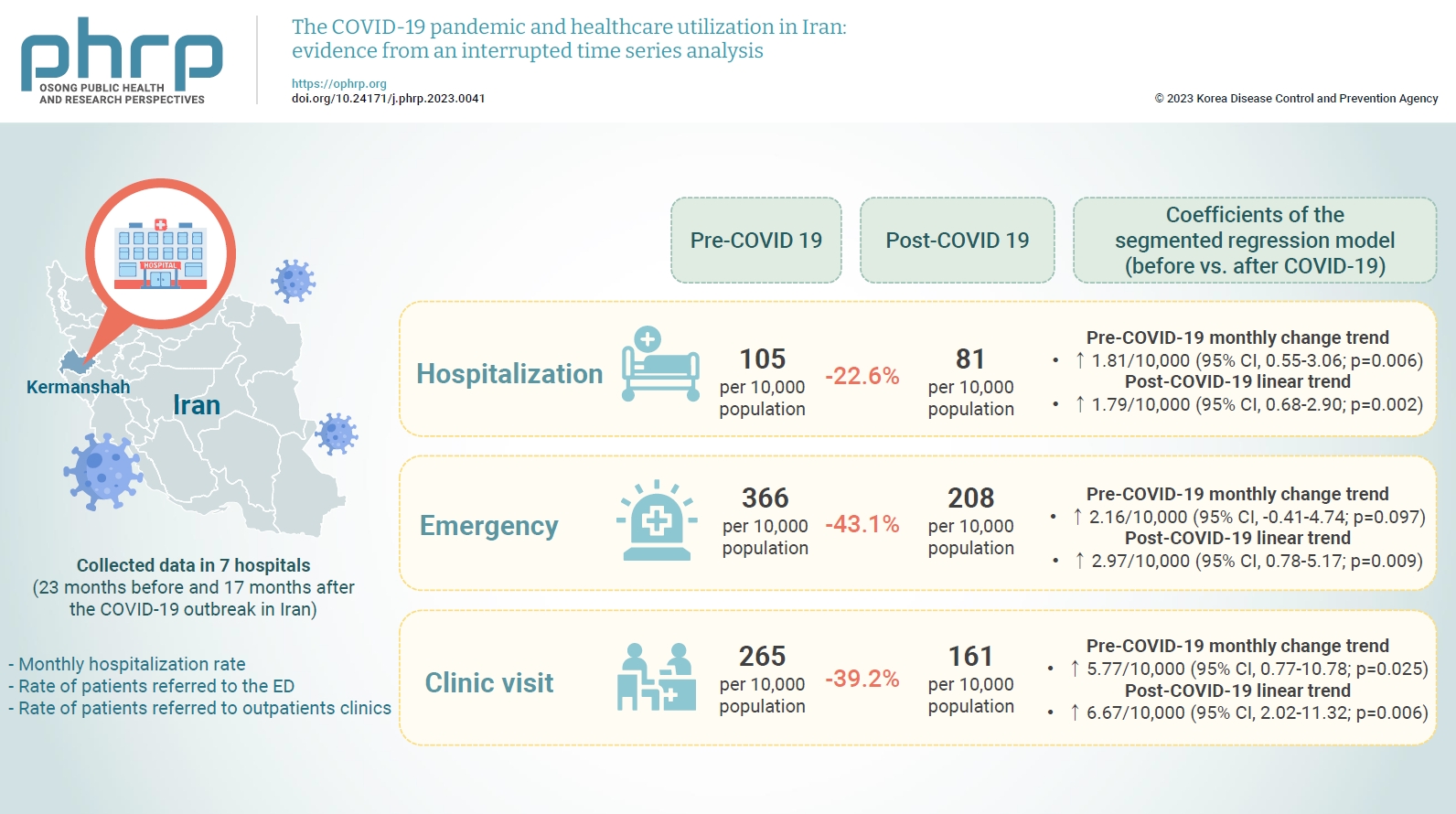
- The descriptive results suggested that, while the average hospitalization rate before the outbreak was 105 hospitalizations per 10,000 population, the corresponding figure for the period after the outbreak was 81 hospitalizations per 10,000 population. The results also indicated 22.6%, 43.1% and 39.2% reductions in hospitalization rate, ED visits, and outpatient clinic visits, respectively, following the COVID-19 outbreak. Table 1 reports pre- and post-COVID-19 averages without any time series modeling for all 3 of the variables used in the study.
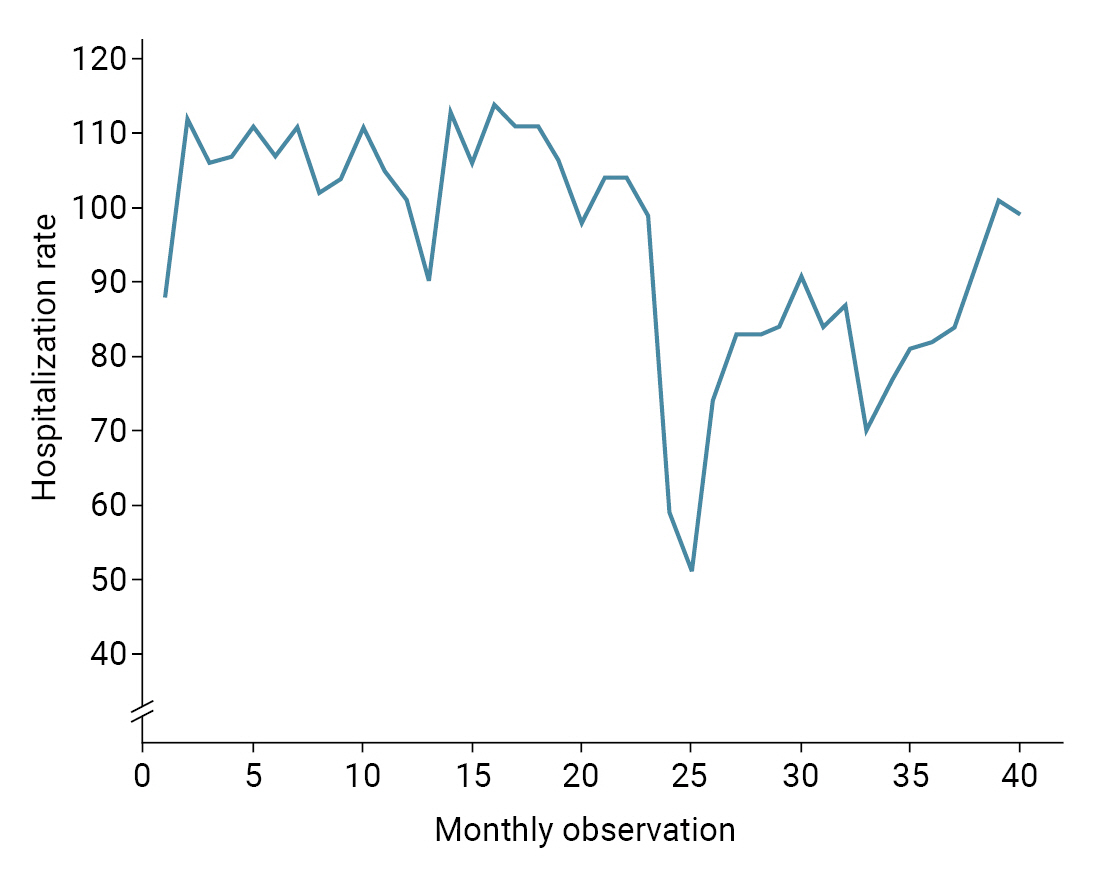
- Table 2 and Figure 1 depict the results of the segmented regression analysis for hospitalization rate. The results indicated an initial estimated hospitalization rate of 105.46 hospitalizations per 10,000 population during the study period. Although the hospitalization rate decreased every month before March 2020, this declining trend was not statistically significant (p=0.941). A statistically significant decrease of 38.11 hospitalizations per 10,000 population (95% confidence interval [CI], 24.93–51.29; p<0.001) was observed in the first month of the COVID-19 outbreak (March 2020). The monthly trend in the hospitalization rate after the COVID-19 outbreak (relative to the pre-COVID-19 trend) increased by 1.81 hospitalizations per 10,000 population (95% CI, 0.55–3.06; p=0.006). We also found that the monthly hospitalization rate after the COVID-19 outbreak increased by 1.79 hospitalizations per 10,000 population (95% CI, 0.68–2.90; p=0.002).
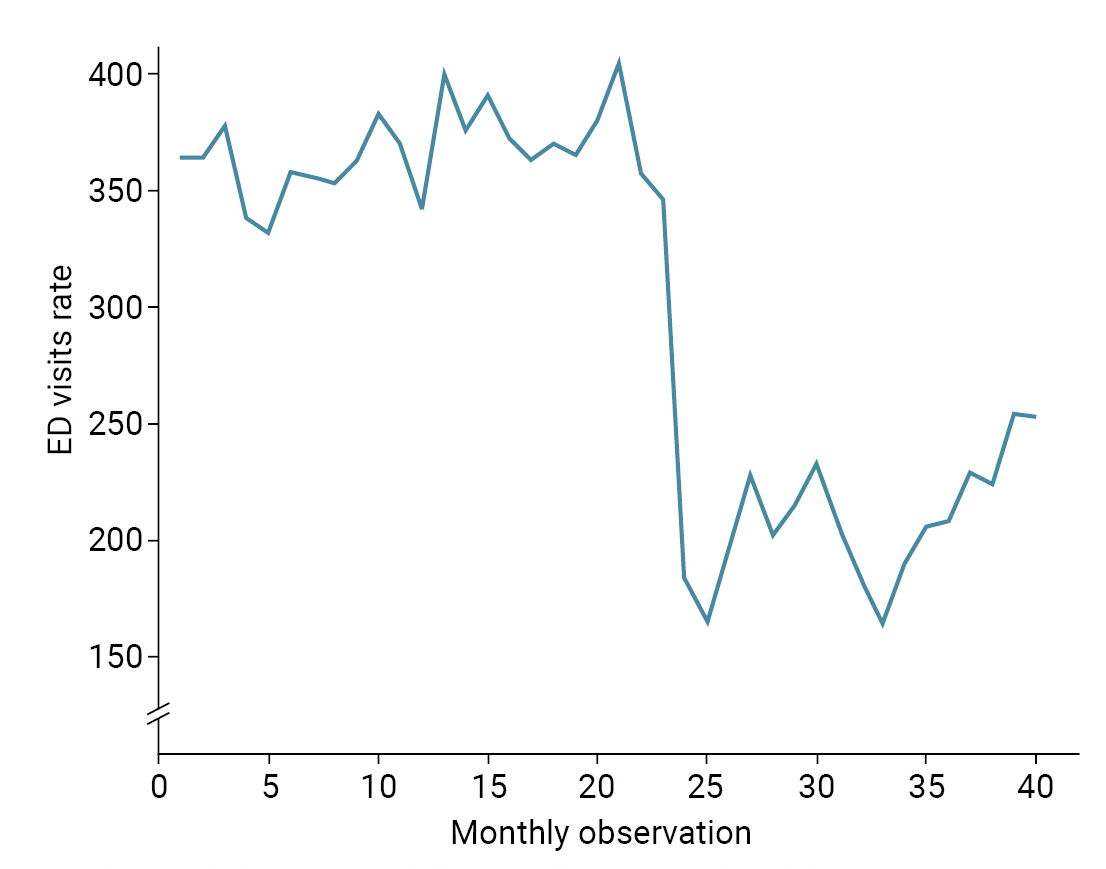
- The results of the segmented regression analysis for ED visits are reported in Table 3 and Figure 2. According to this analysis, the pre-pandemic rate of monthly ED visits was higher by 0.81 visits per 10,000 population. This trend, however, was not statistically significant. A statistically significant decrease of 191.65 ED visits per 10,000 population (95% CI, 166.63–216.66; p<0.001) was observed in the first month of the COVID-19 pandemic (March 2020). Compared to the pre-COVID-19 trend, the monthly trend in ED visits after the COVID-19 outbreak increased by 2.16 visits per 10,000 population, though the change was statistically insignificant (95% CI, –0.41 to 4.74; p=0.097). In addition, a statistically significant increase of 2.97 ED visits per 10,000 population (95% CI, 0.78–5.17; p=0.009) was observed following the COVID-19 outbreak.
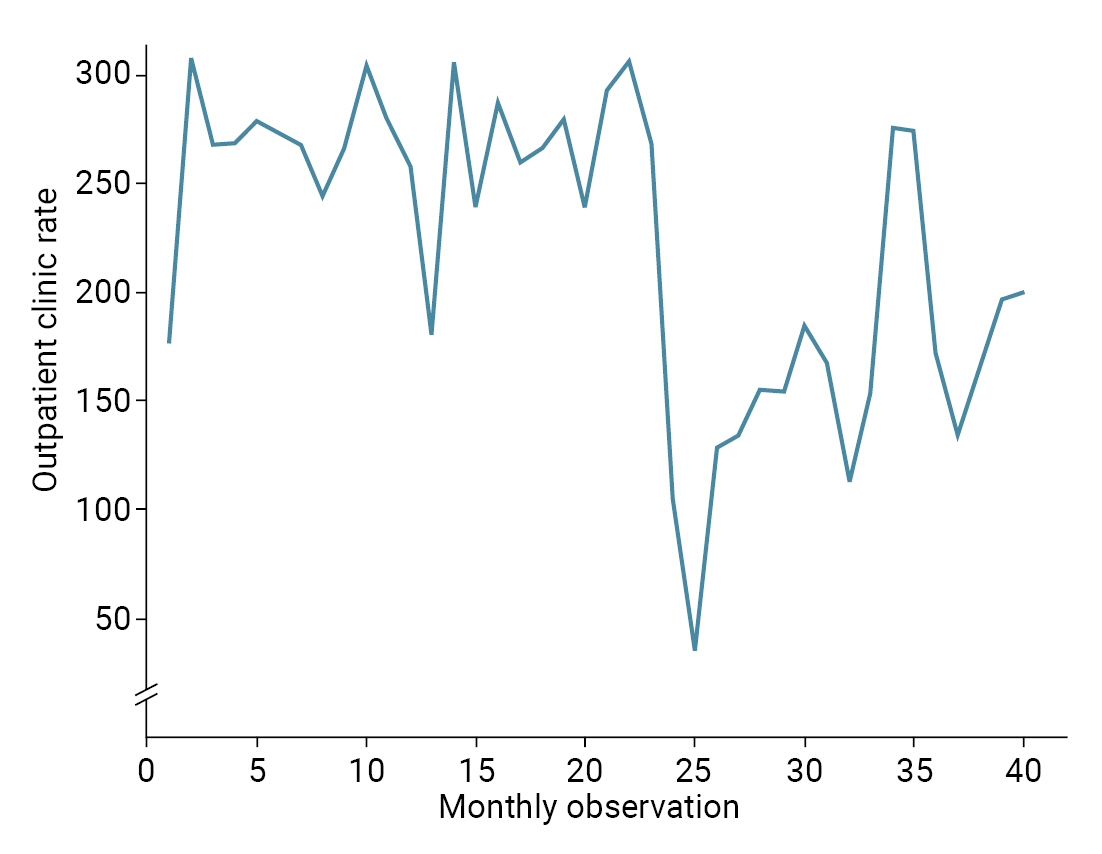
- Table 4 and Figure 3 present the results of the segmented regression analysis for outpatient clinic visits. The initial rate of outpatient clinic visits was estimated at 255.32 visits per 10,000 population. The rate of outpatient clinic visits increased by 0.89 visits per 10,000 population every month before the COVID-19 pandemic, although this trend was not statistically significant (p=0.313). A statistically significant decline of 168.57 outpatient clinic visits per 10,000 population (95% CI, 126.41–210.73; p<0.001) was observed in the first month of the COVID-19 outbreak. The monthly trend in outpatient clinic visits after the COVID-19 outbreak, compared to the pre-COVID-19 trend, increased by 5.77 visits per 10,000 population (95% CI, 0.77–10.78; p=0.025). After the COVID-19 outbreak, the rate of monthly outpatient clinic visits increased by 6.67 visits per 10,000 population (95% CI, 2.02–11.32; p=0.006).
Results
- Our study results show that the COVID-19 pandemic caused a significant decrease in the total number of hospitalizations, ED visits, and referrals to outpatient clinics in the city of Kermanshah. The results indicate a sharp and significant decrease in the use of health services included in the study in the first month after the outbreak of COVID-19. The results also identified 22.6%, 43.1%, and 39.2% reductions in the hospitalization rate, ED visits, and outpatient clinic visits, respectively, following the outbreak of COVID-19. Similar reductions in the utilization of hospital services have also been observed in studies conducted in other countries.
- A study in China by Xiao et al. [16] showed that health facility visits and the number of inpatients decreased by 28.9% and 21.6%, respectively, following the outbreak of COVID-19. Another study in China also showed that hospital visits decreased by 22.6% after the outbreak of the pandemic [17]. Decreasing trends of various degrees were also reported in other countries in terms of hospitalizations, ED visits, and outpatient clinic visits [3,18−20]. A systematic review of 81 studies from different countries showed that the number of hospitalizations and the rate of patient visits to healthcare service providers decreased by an average of 28.4% and 42.3%, respectively [21]. Although it is difficult to compare the rate at which the use of health services decreased between countries due to economic, social, and cultural factors as well as their different healthcare systems, these findings indicate a negative impact on the use of health services following the outbreak of COVID-19.
- This sharp decline in hospital care utilization can be attributed to people's fear of COVID-19 infection and insufficient knowledge about the nature of the disease [22−24]. In EDs, a decrease in daily visits and surgeries could also reflect the population’s fear of being in crowded places [20,25,26]. Changes in ED practices that lowered the admission of general patients may also have resulted in lower overall ED visits [22]. Other issues, such as travel restrictions and quarantine policies, might have played a role in reducing healthcare utilization [27]. Studies have also suggested that care providers might have delayed unnecessary healthcare services to reduce the risk of transmitting the virus to patients and healthcare workers [24,28,29]. Medical centers also suspended outpatient services for non-communicable diseases and non-emergency surgeries [24]. The Centers for Disease Control and Prevention (CDC) recommends the continued use of virtual visits and triage assistance lines and adherence to CDC infection control guidelines to minimize COVID-19 transmission and address public concerns about ED visits during the pandemic [10].
- The hospitalization rate, rate of ED visits, and rate of outpatient clinic visits maintained a downward trend compared to similar periods in 2019 after February 19, 2020, but each showed a slight increase following the outbreak. The subsequent increase in healthcare service utilization can be attributed to the different healthcare needs of the population. The increase in all healthcare services identified in this study remained lower than the rate of healthcare service utilization over the same period in the previous year. This shows that, despite the need for hospital, emergency, and outpatient services, people only sought healthcare when their health-related needs became urgent. This suggests that people continue to avoid in-person healthcare services despite the relaxation of restrictive policies to limit the spread of COVID-19 [24,28].
- Our study identified an increasing trend in healthcare use following a significant reduction after the initial outbreak of the COVID-19 pandemic. A study in Croatia also found that hospital admissions increased from September to December 2020 despite a 51% decrease in total hospital admissions after the outbreak of COVID-19 [30]. A study comparing private and public hospitals in China also identified an increase in the number of admissions to private hospitals in June 2020 [16]. Another study in China also reported that, although a decrease in hospital admissions related to respiratory disease was observed, some health conditions, including diseases of the nervous system, pregnancy and childbirth, congenital anomalies, and chromosomal abnormalities, corresponded to an increase in hospital admissions [17]. These increases in healthcare utilization can be due to previously unmet needs for healthcare services [31] or urgent needs for medical services and healthcare. They may also be due to increased public awareness about COVID-19 and expanded access to care and personal protective equipment.
- Strengths and Limitations
- By conducting an interrupted time series analysis, this study aimed to provide a comprehensive picture of changes in healthcare utilization before and after the outbreak of COVID-19. A significant advantage of this model is it could demonstrate the causal impact of the COVID-19 outbreak on healthcare utilization in the absence of a comparison group [12,13]. However, the study had some limitations. First, although an interrupted time series analysis can control for pre-existing time trends and provide a clear and simple mechanism to track the outcome variables of interest, this approach can be misleading when the impact of an intervention or event is not linear over time. Second, the data used in this study were from educational hospitals affiliated with the MoHME; thus, the study results cannot be generalized to other hospitals with different ownership, including private hospitals or social security organization-affiliated hospitals in Iran. Third, although disease peaks are very important and were among the major factors affecting hospital service utilization in our model, we could not include this variable in our analysis.
Discussion
- Our study findings provide useful insights for healthcare policymakers about the impact of the COVID-19 pandemic on healthcare utilization in Kermanshah Province and Iran as a whole. The results showed that the use of hospital services decreased significantly due to the COVID-19 pandemic, likely due to the changing behaviors of patients and providers, the suspension of health facilities and non-emergency services, and COVID-19-related restrictions. Since the use of healthcare services did not return to pre-outbreak levels 17 months after the outbreak, the government should consider devising and implementing interventions such as telemedicine so that all patients feel safe seeking the care that they need, even during a pandemic. Future research is needed to identify effective strategies and policies to mitigate the long-term and short-term impacts of the pandemic on healthcare utilization in Iran.
Conclusion
- • The study identified 22.6%, 43.1%, and 39.2% reductions in the hospitalization rate, emergency department (ED) visits, and outpatient clinic visits, respectively, following the start of the coronavirus disease 2019 (COVID-19) pandemic.
- • A statistically significant decrease of 38.11 hospitalizations per 10,000 population was observed in the first month of the COVID-19 outbreak.
- • A statistically significant decrease of 191.65 ED visits per 10,000 population was observed in the first month of the COVID-19 pandemic.
- • A statistically significant decrease of 168.57 outpatient visits per 10,000 population was observed in the first month of the COVID-19 outbreak.
HIGHLIGHTS
Supplementary Material
Figure S1.
-
Ethics Approval
This study was approved by the Deputy of Research, Kermanshah University of Medical Sciences (No. IR.KUMS.REC.1400.856), and conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of this study.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
This research received a grant from Kermanshah University of Medical Sciences (grant no. 4010052). The funder did not have any role in the study’s design; the collection, analysis, or interpretation of data, or the drafting of the manuscript.
-
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: SR, MMA, NB; Data curation: NB, SR, AM, MMA; Formal analysis: SR, AKK, SS, MMA; Funding acquisition: SR, MMA; Investigation: SR, SS, AKK, MK, AM; Methodology: SR, AKK, NB, MMA; Project administration: SR, NB, AM, SS; Resources: SR, MMA, MK, NB; Software: SR ; Supervision: SR, NB; Validation: SR, AKK, SS, AM, MH; Visualization: SR; Writing–original draft: SR, SS, NB, MMA, AM, MH; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Article information
| Variable | Coefficient | SEa) | 95% CI | p |
|---|---|---|---|---|
| Intercept, β0 | 105.46 | 3.10 | 99.17 to 111.75 | <0.001 |
| Pre-COVID-19 slope, β1 | –0.016 | 0.22 | –0.47 to 0.44 | 0.941 |
| Change in the level of the outcome variable immediately after the COVID-19 outbreak, β2 | –38.11 | 6.49 | –51.29 to –24.93 | <0.001 |
| Monthly change in trend, β3 | 1.81 | 0.62 | 0.55 to 3.06 | 0.006 |
| Post-COVID-19 linear trendb) | ||||
| Linear trend, βp1 | 1.79 | 0.54 | 0.68 to 2.90 | 0.002 |
SE, standard error; CI, confidence interval.
a) Newey-West standard errors.
b) This was obtained using the following time trend equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of the hospitalization rate at time t after the start of the COVID-19 pandemic, and timept is the time trend variable, which takes values between 1 (first observation after the start of the pandemic) and 17 (last observation after the start of the pandemic).
| Variable | Coefficient | SEa) | 95% CI | p |
|---|---|---|---|---|
| Intercept, β0 | 356.54 | 7.63 | 341.06 to 372.02 | <0.001 |
| Pre-COVID-19 slope, β1 | 0.81 | 0.58 | –0.37 to 1.99 | 0.171 |
| Change in the level of the outcome variable immediately after the COVID-19 outbreak, β2 | –191.65 | 12.33 | –216.66 to –166.63 | <0.001 |
| Monthly change in trend, β3 | 2.16 | 1.26 | –0.41 to 4.74 | 0.097 |
| Post-COVID-19 linear trendb) | ||||
| Linear trend, βp1 | 2.97 | 1.08 | 0.78 to 5.17 | 0.009 |
SE, standard error; CI, confidence interval.
a) Newey-West standard errors.
b) This was obtained from the following time trend equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of the rate of emergency department visits at time t after the start of the COVID-19 pandemic, and timept is the time trend variable, which takes values between 1 (first observation after the start of the pandemic) and 17 (last observation after the start of the pandemic).
| Variable | Coefficient | SEa) | 95% CI | p |
|---|---|---|---|---|
| Intercept, β0 | 255.32 | 13.82 | 227.10 to 283.17 | <0.001 |
| Pre-COVID-19 slope, β1 | 0.89 | 0.87 | –0.88 to 2.67 | 0.313 |
| Change in the level of the outcome variable immediately after the COVID-19 outbreak, β2 | –168.57 | 20.78 | –210.73 to –126.41 | <0.001 |
| Monthly change in trend, β3 | 5.77 | 2.47 | 0.77 to 10.78 | 0.025 |
| Post-COVID-19 linear trendb) | ||||
| Linear trend, βp1 | 6.67 | 2.29 | 2.02 to 11.32 | 0.006 |
SE, standard error; CI, confidence interval.
a) Newey-West standard errors.
b) This was obtained using the following time trend equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of the rate of outpatient clinic visits at time t after the start of the COVID-19 pandemic, and timept is the time trend variable, which takes values between 1 (first observation after the start of the pandemic) and 17 (last observation after the start of the pandemic).
- 1. Park AK, Kim IH, Kim J, et al. Genomic surveillance of SARS-CoV-2: distribution of clades in the Republic of Korea in 2020. Osong Public Health Res Perspect 2021;12:37−43.ArticlePubMedPMCPDF
- 2. Provenzano DA, Sitzman BT, Florentino SA, et al. Clinical and economic strategies in outpatient medical care during the COVID-19 pandemic. Reg Anesth Pain Med 2020;45:579−85.ArticlePubMedPMC
- 3. De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;383:88−9.ArticlePubMed
- 4. Salimi R, Gomar R, Heshmati B. The COVID-19 outbreak in Iran. J Glob Health 2020;10:010365. ArticlePubMedPMC
- 5. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020;323:1545−6.ArticlePubMed
- 6. Yazdani S, Bayazidi S, Cheraghi M, et al. Resilience during quarantine with the outbreak of COVID-19 in Iran. Int J Educ Appl Sci 2022;3:1−4.
- 7. Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 2021;11:e045343. Article
- 8. Angoulvant F, Ouldali N, Yang DD, et al. Coronavirus disease 2019 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections: a time series analysis. Clin Infect Dis 2021;72:319−22.ArticlePubMedPDF
- 9. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083−8.PubMed
- 10. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits: United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699−704.ArticlePubMedPMC
- 11. Scaramuzza A, Tagliaferri F, Bonetti L, et al. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child 2020;105:704−6.Article
- 12. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 2017;46:348−55.PubMed
- 13. Linden A. A matching framework to improve causal inference in interrupted time-series analysis. J Eval Clin Pract 2018;24:408−15.ArticlePubMedPDF
- 14. Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ 2015;350:h2750. ArticlePubMedPMC
- 15. Rashidian A, Joudaki H, Khodayari-Moez E, et al. The impact of rural health system reform on hospitalization rates in the Islamic Republic of Iran: an interrupted time series. Bull World Health Organ 2013;91:942−9.ArticlePubMedPMC
- 16. Xiao H, Dai X, Wagenaar BH, et al. The impact of the COVID-19 pandemic on health services utilization in China: time-series analyses for 2016-2020. Lancet Reg Health West Pac 2021;9:100122. ArticlePubMedPMC
- 17. Yang ZM, Wu MY, Lu JM, et al. Effect of COVID-19 on hospital visits in Ningbo, China: an interrupted time-series analysis. Int J Qual Health Care 2021;33:mzab078. ArticlePubMedPDF
- 18. Birkmeyer JD, Barnato A, Birkmeyer N, et al. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39:2010−7.ArticlePubMedPMC
- 19. O’Connell RM, Khan MA, Amir M, et al. The impact of COVID-19 on emergency general surgery admissions and operative volumes: a single centre experience. Surgeon 2021;19:e207−12.ArticlePubMed
- 20. Mitchell RD, O’Reilly GM, Mitra B, et al. Impact of COVID-19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emerg Med Australas 2020;32:1027−33.PubMedPMC
- 21. Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 2021;11:e045343.ArticlePubMed
- 22. Oseran AS, Nash D, Kim C, et al. Changes in hospital admissions for urgent conditions during COVID-19 pandemic. Am J Manag Care 2020;26:327−8.ArticlePubMed
- 23. Delamou A, Ayadi AM, Sidibe S, et al. Effect of Ebola virus disease on maternal and child health services in Guinea: a retrospective observational cohort study. Lancet Glob Health 2017;5:e448−57.ArticlePubMedPMC
- 24. Modesti PA, Wang J, Damasceno A, et al. Indirect implications of COVID-19 prevention strategies on non-communicable diseases: an opinion paper of the European Society of Hypertension Working Group on Hypertension and Cardiovascular Risk Assessment in Subjects Living in or Emigrating from Low Resource Settings. BMC Med 2020;18:256. PubMedPMC
- 25. Rennert-May E, Leal J, Thanh NX, et al. The impact of COVID-19 on hospital admissions and emergency department visits: a population-based study. PLoS One 2021;16:e0252441.ArticlePubMedPMC
- 26. Wongtanasarasin W, Srisawang T, Yothiya W, et al. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: a hospital-based study. Emerg Med Australas 2021;33:316−23.PubMed
- 27. McIntosh A, Bachmann M, Siedner MJ, et al. Effect of COVID-19 lockdown on hospital admissions and mortality in rural KwaZulu-Natal, South Africa: interrupted time series analysis. BMJ Open 2021;11:e047961.ArticlePubMed
- 28. Madhuripan N, Cheung HM, Alicia Cheong LH, et al. Variables influencing radiology volume recovery during the next phase of the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol 2020;17:855−64.ArticlePubMedPMC
- 29. D’Apolito R, Faraldi M, Ottaiano I, et al. Disruption of arthroplasty practice in an orthopedic center in Northern Italy during the coronavirus disease 2019 pandemic. J Arthroplasty 2020;35(7S). S6−9.ArticlePubMedPMC
- 30. Kalanj K, Marshall R, Karol K, et al. The impact of COVID-19 on hospital admissions in Croatia. Front Public Health 2021;9:720948. ArticlePubMedPMC
- 31. Karami Matin B, Hajizadeh M, Najafi F, et al. The impact of health sector evolution plan on hospitalization and cesarean section rates in Iran: an interrupted time series analysis. Int J Qual Health Care 2018;30:75−9.ArticlePubMed
References
Figure & Data
References
Citations



 Cite
Cite