Search
- Page Path
- HOME > Search
- Predictors of outcomes 3 to 12 months after traumatic brain injury: a systematic review and meta-analysis
- Younes Iderdar, Maryem Arraji, Nadia Al Wachami, Morad Guennouni, Karima Boumendil, Yassmine Mourajid, Noureddine Elkhoudri, Elmadani Saad, Mohamed Chahboune
- Osong Public Health Res Perspect. 2024;15(1):3-17. Published online February 5, 2024
- DOI: https://doi.org/10.24171/j.phrp.2023.0288
- 1,042 View
- 72 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 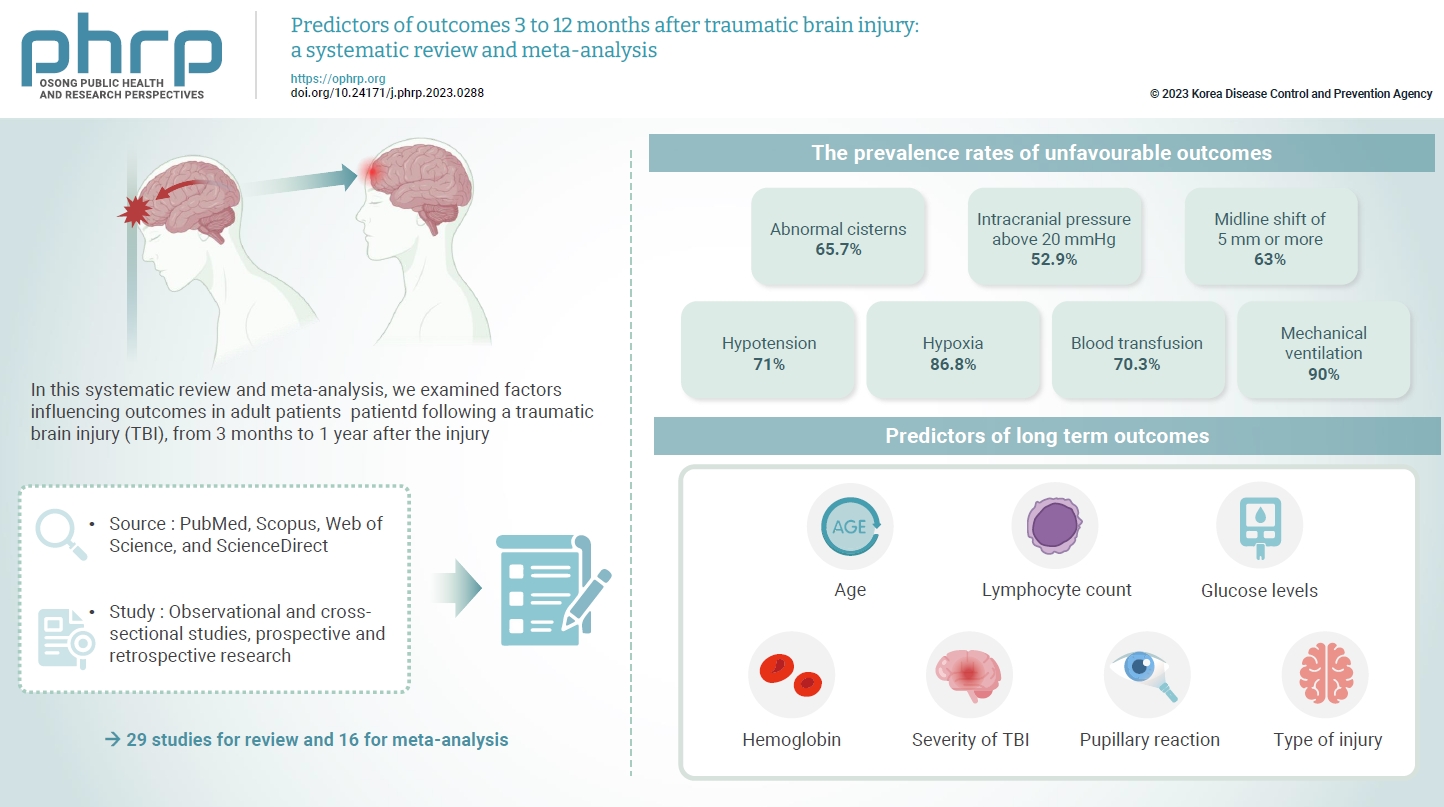
- The exact factors predicting outcomes following traumatic brain injury (TBI) remain elusive. In this systematic review and meta-analysis, we examined factors influencing outcomes in adult patients with TBI, from 3 months to 1 year after injury. A search of four electronic databases—PubMed, Scopus, Web of Science, and ScienceDirect—yielded 29 studies for review and 16 for meta-analysis, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. In patients with TBI of any severity, mean differences were observed in age (8.72 years; 95% confidence interval [CI], 4.77–12.66 years), lymphocyte count (−0.15 109/L; 95% CI, −0.18 to −0.11), glucose levels (1.20 mmol/L; 95% CI, 0.73–1.68), and haemoglobin levels (−0.91 g/dL; 95% CI, −1.49 to −0.33) between those with favourable and unfavourable outcomes. The prevalence rates of unfavourable outcomes were as follows: abnormal cisterns, 65.7%; intracranial pressure above 20 mmHg, 52.9%; midline shift of 5 mm or more, 63%; hypotension, 71%; hypoxia, 86.8%; blood transfusion, 70.3%; and mechanical ventilation, 90%. Several predictors were strongly associated with outcome. Specifically, age, lymphocyte count, glucose level, haemoglobin level, severity of TBI, pupillary reaction, and type of injury were identified as potential predictors of long-term outcomes.
- Case of
Rickettsia typhi -induced Brain Abscess Mimicking Brain Tumor - Yoonhyuk Jang, Jangsup Moon, Jin-Sun Jun, Tae-joon Kim, Kyung-Il Park, Soon-Tae Lee, Keun-Hwa Jung, Sang Kun Lee, Kon Chu
- Osong Public Health Res Perspect. 2018;9(3):122-125. Published online June 30, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.3.07
- 4,409 View
- 112 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Murine typhus is one of the most prevalent rickettsial infections in the world, caused by the bacterial genus
Rickettsia . Though the disease manifests a relatively benign clinical course with fever, rash, and headache being the 3 classic symptoms, neurological complications may arise in patients that could become permanent. In this case study, a patient with a brain abscess caused byR typhi infection is described. Based upon the recent reemergence of arthropod-borne disease, the findings in this case are significant;R typhi can cause a brain abscess that mimics a brain tumor, which delays the diagnosis and appropriate management of the disease. Murine typhus should always be considered when performing the differential diagnosis of brain abscesses in South Korea.-
Citations
Citations to this article as recorded by- Meningoencephalitis and retinal vasculitis due to rickettsial infection
Louisa Lehner, Stephan Thurau, Konstantin Pusl, Steffen Tiedt, Florian Schöberl, Robert Forbrig, Günter Höglinger, Michael Strupp
Journal of Neurology.2024; 271(3): 1469. CrossRef - Giant Actinomyces brain abscess in an immunocompetent child: A management strategy
Nicole H. Chicoine, Jackson Griffith-Linsley, Joling Goh, John J. Manaloor, Jeffrey S. Raskin
Surgical Neurology International.2021; 12: 325. CrossRef
- Meningoencephalitis and retinal vasculitis due to rickettsial infection
- Therapeutic Intervention for Visuo-Spatial Neglect after Stroke: A Meta-Analysis of Randomized Controlled Trials
- Jae-Sung Kwon
- Osong Public Health Res Perspect. 2018;9(2):59-65. Published online April 30, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.2.04
- 6,049 View
- 73 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The aims of this meta-analysis were to examine intervention methods of qualitatively, well-designed studies from the past 10 years for treating visuo-spatial neglect (VSN) in patients who had suffered a stroke, and to evaluate the combined effects of intervention.
Methods Studies published between 2008 and 2017 on the theme of VSN were collected from PubMed, CINAHL, and MEDLINE, representative academic databases and search engines. The PEDro scale was used for evaluating the quality of methodology. The sample size, mean, and standard deviation of identified studies were used for meta-analysis.
Results Eight studies were selected for analysis. The PEDro scores of the selected studies were ≥ 7, with 237 subjects analyzed. The results of intervention were classified into “mental function” and “activity and participation” based on the International Classification of Functioning, Disability and Health. The analyzed effect sizes for combined outcomes, mental function and, activity and participation, were 0.728 (medium effect size), 0.850 (large effect size), and 0.536 (medium effect size), respectively.
Conclusion Intervention methods for treating VSN had a short-term effect on cognitive function (visual perception). In particular, non-invasive brain stimulation therapy showed a large effect size for VSN treatment.
-
Citations
Citations to this article as recorded by- Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury
Verity Longley, Christine Hazelton, Calvin Heal, Alex Pollock, Kate Woodward-Nutt, Claire Mitchell, Gorana Pobric, Andy Vail, Audrey Bowen
Cochrane Database of Systematic Reviews.2021;[Epub] CrossRef - Neural Mechanisms of Spatial Attention Deficits in Trauma
Stefanie R. Russman Block, Daniel H. Weissman, Chandra Sripada, Mike Angstadt, Elizabeth R. Duval, Anthony P. King, Israel Liberzon
Biological Psychiatry: Cognitive Neuroscience and .2020; 5(10): 991. CrossRef - Updated Approach to Stroke Rehabilitation
Leroy R. Lindsay, Diane A. Thompson, Michael W. O’Dell
Medical Clinics of North America.2020; 104(2): 199. CrossRef - Implementing a Rehabilitation Protocol for Spatial Neglect Assessment and Treatment in an Acute Care Hospital
Kimberly Hreha, Peii Chen, Jennifer LaRosa, Christopher Santos, Cindy Gocon, A.M. Barrett
Journal of Acute Care Physical Therapy.2020; 11(2): 59. CrossRef - Alertness Training Improves Spatial Bias and Functional Ability in Spatial Neglect
Thomas Van Vleet, Paolo Bonato, Eric Fabara, Sawsan Dabit, Sarah‐Jane Kim, Christopher Chiu, Antonio Luigi Bisogno, Michael Merzenich, Maurizio Corbetta, Joseph DeGutis
Annals of Neurology.2020; 88(4): 747. CrossRef
- Non-pharmacological interventions for spatial neglect or inattention following stroke and other non-progressive brain injury



 First
First Prev
Prev


