Search
- Page Path
- HOME > Search
Original Articles
- COVID-19 outbreak in a religious village community in Republic of Korea and risk factors for transmission
- Jiae Shim, Eunju Lee, Eunyoung Kim, Yeonhwa Choi, Giseok Kang, Bryan Inho Kim
- Osong Public Health Res Perspect. 2023;14(2):110-118. Published online April 5, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0002
- 1,499 View
- 72 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 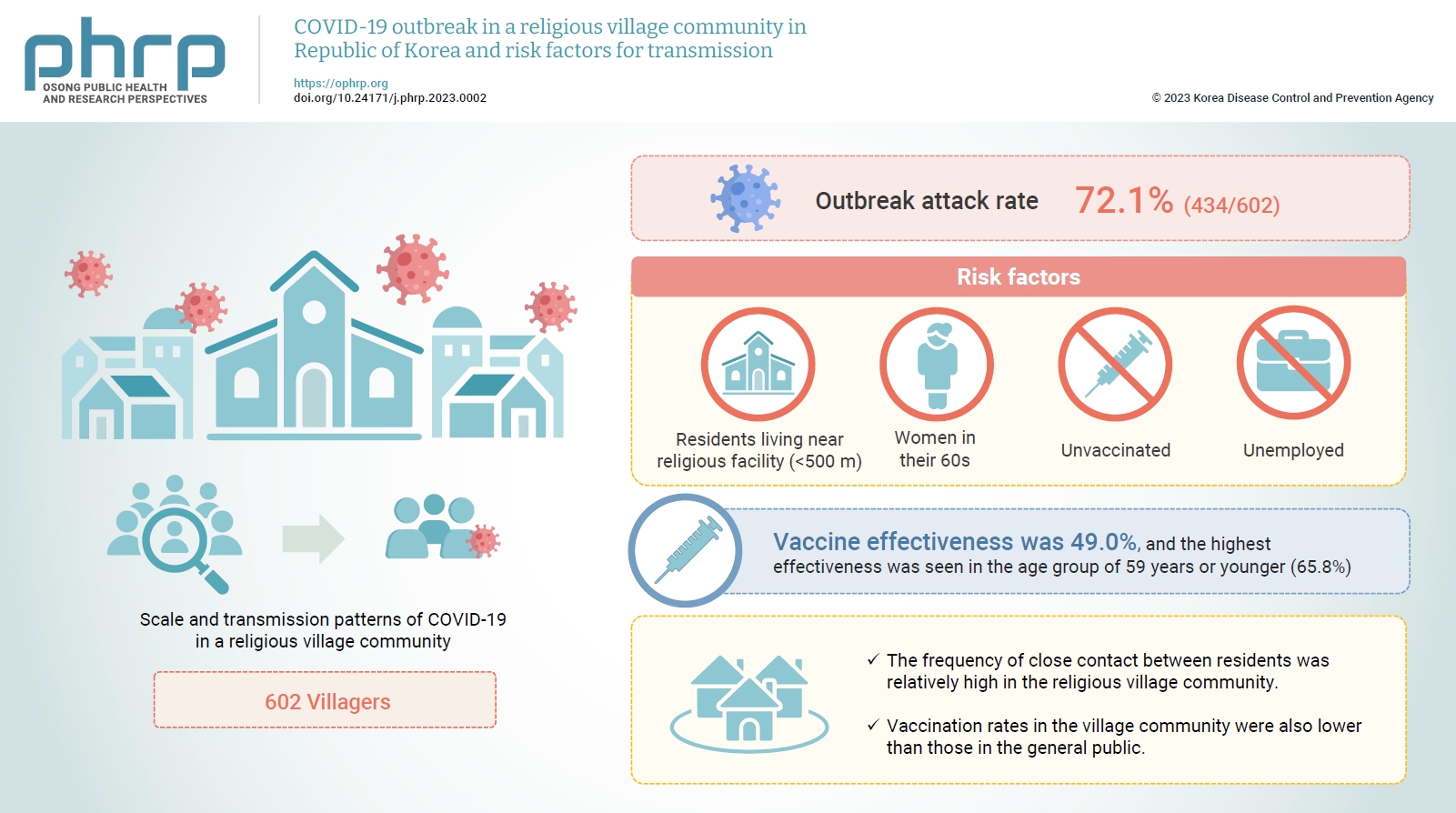
- Objectives
This study aimed to assess the scale and transmission patterns of coronavirus disease 2019 (COVID-19) in a religious village community in South Korea, to determine the risk factors of transmission, and to evaluate vaccine effectiveness.
Methods
An epidemiological survey was conducted, and data were collected and analyzed from 602 villagers in the religious village community. Multivariate logistic regression analysis was used to identify the risk factors for COVID-19 transmission and to evaluate vaccine effectiveness.
Results
The outbreak attack rate was 72.1% (434/602). The attack rate was high among women in their 60s, the unemployed, residents living near religious facility (<500 m), and the unvaccinated. Age, the distance between religious facility and residences, and the absence of vaccination were identified as risk factors for transmission. Vaccine effectiveness was 49.0%, and the highest effectiveness was seen in the age group of 59 years or younger (65.8%).
Conclusion
This village community was isolated, with little communication with the outside world. However, the frequency of close contact between residents was relatively high, contributing to the spread of COVID-19 in the village even with relatively short exposure. Vaccination rates in the village community were also lower than those in the general public. Public health authorities should consider the potential impact of cultural factors, including religion, that could lead to the exponential spread of COVID-19 in closed village communities.
- mRNA vaccine effectiveness against SARS-CoV-2 B.1.617.2 (Delta) and B.1.1.529 (Omicron) variant transmission from home care cases to household contacts in South Korea
- Hanul Park, Young Joon Park, Sang Eun Lee, Min Jei Lee, Hyungtae Ahn
- Osong Public Health Res Perspect. 2022;13(6):435-442. Published online November 28, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0243
- 4,738 View
- 171 Download
- 1 Web of Science
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 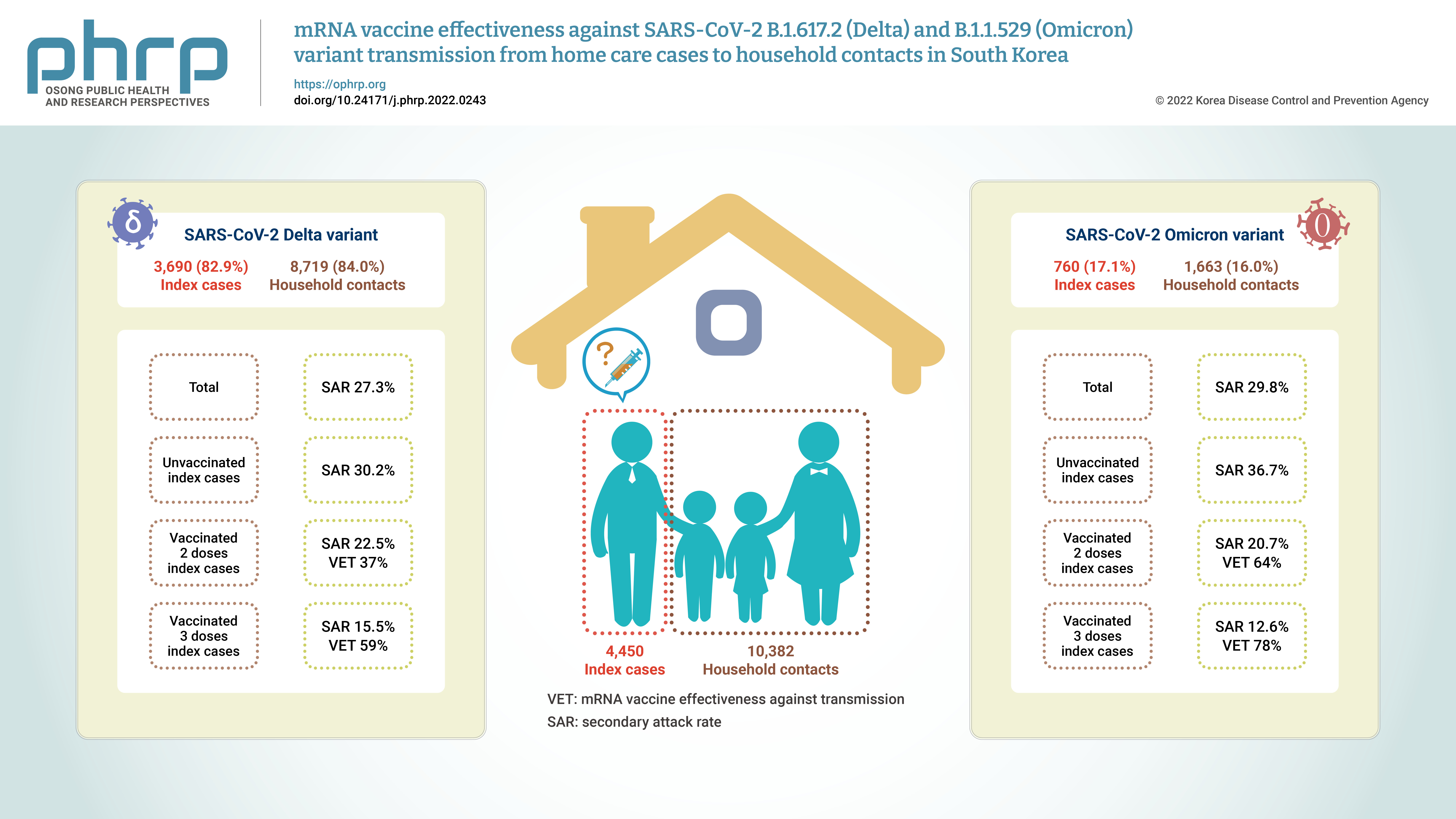
- Objectives
Household contacts of confirmed cases of coronavirus disease 2019 (COVID-19) areexposed to a high risk of viral transmission, and secondary incidence is an important indicatorof community transmission. This study analyzed the secondary attack rate and mRNA vaccineeffectiveness against transmission (VET) for index cases (patients treated at home) confirmedto be infected with the Delta and Omicron variants.Methods: The subjects of the study were 4,450 index cases and 10,382 household contacts.Logistic regression analysis was performed to compare the secondary attack rate byvaccination status, and adjusted relative risk and 95% confidence intervals were identified.Results: The secondary attack rate of the Delta variant was 27.3%, while the secondary attackrate of the Omicron variant was 29.8%. For the Delta variant, groups with less than 90 daysand more than 90 days after 2 doses of mRNA vaccination both showed a VET of 37%. For theOmicron variant, a 64% VET was found among those with less than 90 days after 2 doses ofmRNA vaccination.Conclusion: This study provides useful data on the secondary attack rate and VET of mRNAvaccines for household contacts of COVID-19 cases in South Korea. -
Citations
Citations to this article as recorded by- Household secondary attack rates and risk factors during periods of SARS-CoV-2 Delta and Omicron variant predominance in the Republic of Korea
Jin Lee, Mijeong Ko, Seontae Kim, Dosang Lim, Gemma Park, Sang-Eun Lee
Osong Public Health and Research Perspectives.2023; 14(4): 263. CrossRef
- Household secondary attack rates and risk factors during periods of SARS-CoV-2 Delta and Omicron variant predominance in the Republic of Korea
- Evaluation of the Effectiveness of Pandemic Influenza A(H1N1) 2009 Vaccine Based on an Outbreak Investigation During the 2010–2011 Season in Korean Military Camps
- Kyo-Hyun Kim, Yoon Gu Choi, Hyun-Bae Yoon, Jung-Woo Lee, Hyun-Wook Kim, Chaeshin Chu, Young-Joon Park
- Osong Public Health Res Perspect. 2013;4(4):209-214. Published online August 31, 2013
- DOI: https://doi.org/10.1016/j.phrp.2013.07.002
- 3,007 View
- 18 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
In December 2010, there was an outbreak of acute febrile respiratory disease in many Korean military camps that were not geographically related. A laboratory analysis confirmed a number of these cases to be infected by the pandemic influenza A(H1N1) 2009 (H1N1pdm09) virus. Because mass vaccination against H1N1pdm09 was implemented at the infected military camps eleven months ago, the outbreak areas in which both vaccinated and nonvaccinated individuals were well mixed, gave us an opportunity to evaluate the effectiveness of H1N1pdm09 vaccine through a retrospective cohort study design.
Methods
A self-administered questionnaire was distributed to the three military camps in which the outbreak occurred for case detection, determination of vaccination status, and characterization of other risk factors. The overall response rate was 86.8% (395/455). Case was defined as fever (≥38 °C) with cough or sore throat, influenza-like illness (ILI), and vaccination status verified by vaccination registry. Crude vaccine effectiveness (VE) was calculated as “1 − attack rate in vaccinated individuals/attack rate in nonvaccinated individuals”, and adjusted VE was calculated as “1 – odds ratio” using logistic regression adjusted for potential confounding factor. A number of ILI definitions were used to test the robustness of the result.
Results
The attack rate of ILI was 12.8% in register-verified vaccinated individuals and 24.0% in nonvaccinated individuals. The crude VE was thus calculated to be 46.8% [95% confidence interval (CI): 14.5–66.9]. The adjusted VE rate was 46.8% (95% CI: –9.4 to 74.1). Various combinations of ILI symptoms also showed similar VE rates.
Conclusion
We evaluated the effectiveness of H1N1pdm09 vaccine in the 2010–2011 season in an outbreak setting. Although the result was not sensitive to any analytical method used and ILI case definition, the magnitude of effectiveness was lower than estimated in the 2009–2010 season. -
Citations
Citations to this article as recorded by- Assessment of Intensive Vaccination and Antiviral Treatment in 2009 Influenza Pandemic in Korea
Chaeshin Chu, Sunmi Lee
Osong Public Health and Research Perspectives.2015; 6(1): 47. CrossRef - Was the Mass Vaccination Effective During the Influenza Pandemic 2009–2010 in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2013; 4(4): 177. CrossRef
- Assessment of Intensive Vaccination and Antiviral Treatment in 2009 Influenza Pandemic in Korea



 First
First Prev
Prev


