Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(2); 2023 > Article
-
Original Article
COVID-19 outbreak in a religious village community in Republic of Korea and risk factors for transmission -
Jiae Shim1
 , Eunju Lee1
, Eunju Lee1 , Eunyoung Kim1
, Eunyoung Kim1 , Yeonhwa Choi1
, Yeonhwa Choi1 , Giseok Kang2
, Giseok Kang2 , Bryan Inho Kim3
, Bryan Inho Kim3
-
Osong Public Health and Research Perspectives 2023;14(2):110-118.
DOI: https://doi.org/10.24171/j.phrp.2023.0002
Published online: April 5, 2023
1Division of Infectious Disease Response, Chungnam Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency, Daejeon, Republic of Korea
2Chungnam Center for Infectious Diseases Control and Prevention, Hongseong, Republic of Korea
3Division of Infectious Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- Corresponding author: Bryan Inho Kim Division of Infectious Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Republic of Korea E-mail: globalepi@korea.kr
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 1,528 Views
- 73 Download
Abstract
-
Objectives
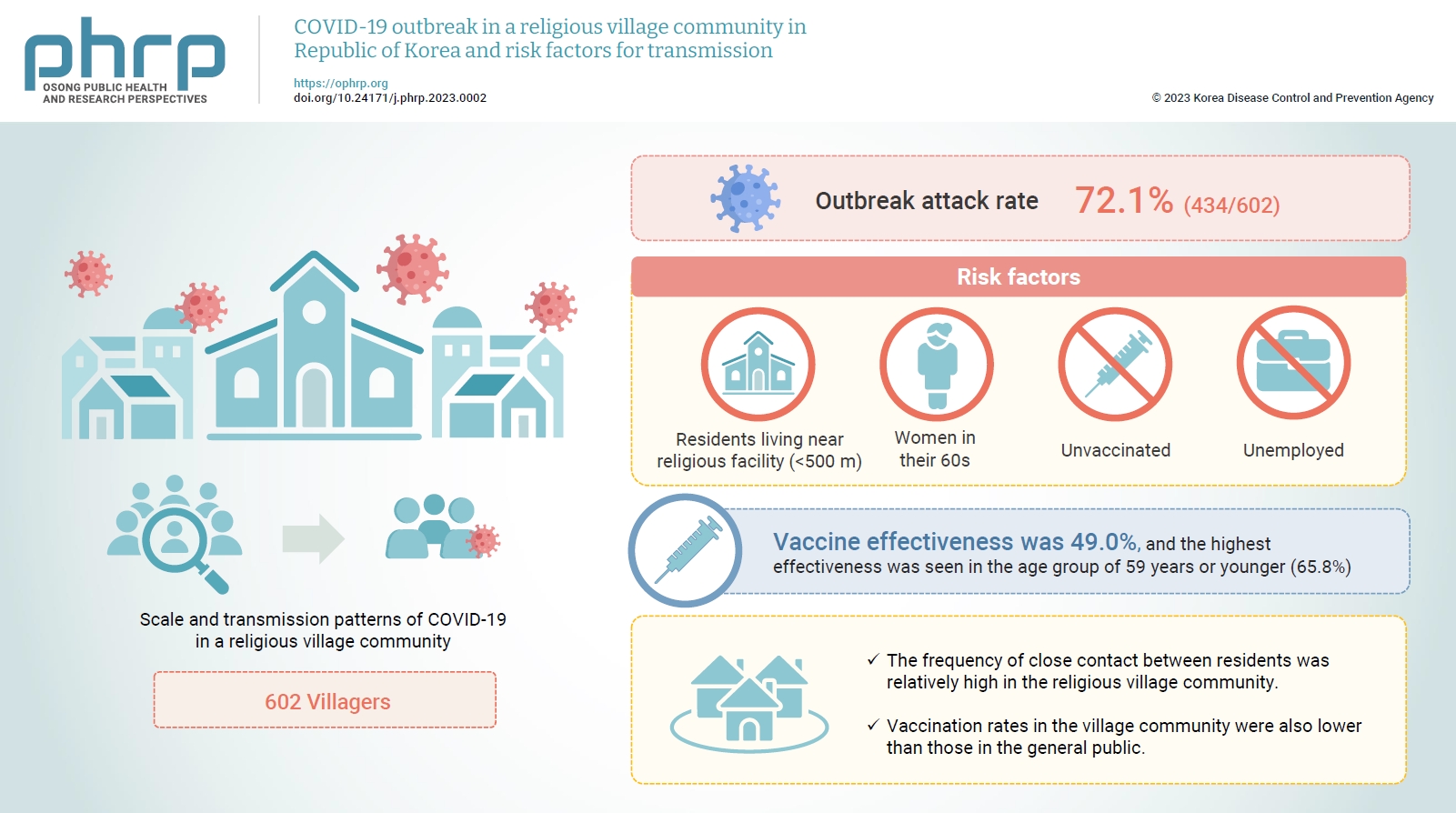
- This study aimed to assess the scale and transmission patterns of coronavirus disease 2019 (COVID-19) in a religious village community in South Korea, to determine the risk factors of transmission, and to evaluate vaccine effectiveness.
-
Methods
- An epidemiological survey was conducted, and data were collected and analyzed from 602 villagers in the religious village community. Multivariate logistic regression analysis was used to identify the risk factors for COVID-19 transmission and to evaluate vaccine effectiveness.
-
Results
- The outbreak attack rate was 72.1% (434/602). The attack rate was high among women in their 60s, the unemployed, residents living near religious facility (<500 m), and the unvaccinated. Age, the distance between religious facility and residences, and the absence of vaccination were identified as risk factors for infection. Vaccine effectiveness was 49.0%, and the highest effectiveness was seen in the age group of 59 years or younger (65.8%).
-
Conclusion
- This village community was isolated, with little communication with the outside world. However, the frequency of close contact between residents was relatively high, contributing to the spread of COVID-19 in the village even with relatively short exposure. Vaccination rates in the village community were also lower than those in the general public. Public health authorities should consider the potential impact of cultural factors, including religion, that could lead to the exponential spread of COVID-19 in closed village communities.
- Since the start of the coronavirus disease 2019 (COVID-19) pandemic in late December 2019, more than 24 million cumulative confirmed cases have been reported in South Korea between January 20, 2020, and September 25, 2022 [1]. South Korea has maintained the crisis alert level at “serious” and has made various efforts to prevent the spread of COVID-19 [2]. For instance, social distancing measures were implemented, such as working from home, school closures, and meeting restrictions, as well as other policies such as wearing masks, hand hygiene, and vaccination [3,4].
- Since 2020, several variants of COVID-19 have been reported, raising concerns about the effectiveness of vaccination [5,6]. The Delta variant, first detected in India in 2020, accounted for 99% of cases in the United States and accelerated hospitalizations due to its high transmissibility [7]. In South Korea, the Delta variant was prevalent from July 2021 to the end of January 2022. Although there were some differences by age, the COVID-19 vaccination rate for the first dose by September 17, 2021 was approximately 70% [2]. The COVID-19 vaccine was found to be effective in reducing the risk of infection and mortality during the period when the Delta variant was prevalent [6,8].
- COVID-19 is known to be transmitted through respiratory droplets, and outbreaks are particularly common in “3-C” environments (close contact, closed spaces, and crowded places) [9]. In particular, religious practices such as group prayers, religious education attendance, and sharing a meal may increasingly influence the spread of COVID-19 [9–11]. Approximately 48% of confirmed cases of COVID-19 in Malaysia were related to religious events [12]. In addition, the possibility of widespread transmission within religious groups has been demonstrated in the United States [11]. In 2020, South Korea experienced a rapid, large-scale outbreak of COVID-19 in the local community, triggered by the Shincheonji Church’s religious activities and group outreach, mainly in Daegu [13]. Those who have experienced the COVID-19 outbreak are reported to experience mental health problems such as loneliness, anxiety, depression, as well as social problems such as stigma [14,15].
- This study aimed to determine the extent and transmission pattern of the outbreak of COVID-19 in a religious village community in South Korea when the Delta variant was prevalent, to evaluate vaccine effectiveness, and to identify risk factors for transmission at the village level.
Introduction
- Outbreak Detection
- On November 21, 2021, a religious member (a 77-year-old woman) living in a village of a religious community was confirmed positive for COVID-19. She was tested due to a chief complaint of muscle pain and chills that had lasted since November 19, 2021. After her contacts were traced and tested, 4 additional cases were confirmed, suggesting transmission.
- Case Definition and Epidemiological Investigations
- Regardless of clinical manifestations, positive cases were confirmed for COVID-19 using real-time polymerase chain reaction tests of specimens collected from the upper or lower respiratory tract. In accordance with the Infectious Disease Prevention and Control Act, basic epidemiological investigations were conducted on confirmed cases, including information on the individual, symptoms, and underlying diseases; the source of infection; religious group activities; and interpersonal contacts. Among the confirmed cases, the index case was determined to have the earliest confirmed date. Moreover, the suspected primary case was determined to have the earliest symptom onset by reviewing data, such as the date of symptom onset described in the basic epidemiological survey and details of medical institutions obtained through drug utilization review. The epidemiological investigation determined the management level by assessing the risk of exposure according to the COVID-19 response guidelines [16]. “Unvaccinated” referred to individuals that had not been vaccinated or were within 14 days of receiving the first dose. “Vaccinated” referred to individuals for whom 14 days had elapsed since the second dose.
- COVID-19 Control Measures for the Religious Community
- When the initial 5 cases were investigated, it was found that the village was populated by people from the same religious group, who formed a village revolving around religious facilities. The health authorities (the Korea Disease Control and Prevention Agency [KDCA] and the local health center) conducted a field epidemiological investigation and risk assessment of the village and discussed measures to manage contacts with confirmed cases to prevent further transmission of the infection.
- In the risk assessment, several religious activities were observed where droplets could spread in confined spaces. Additionally, there were frequent activities involving close physical contact between the religious leaders and members or between members themselves. As the exposure took place in November, the religious facilities were not adequately ventilated due to seasonally low temperatures, and no auxiliary ventilation systems were installed to compensate for this inadequate ventilation. Temperature controls and visitor lists, which were required by social distancing rules in religious facilities, were not properly implemented, and insufficient resources were provided, such as hand sanitizers for hand hygiene. Since an objective assessment of the circumstances of each religious activity was not possible due to the absence of surveillance cameras in the religious facilities, the overall situation was assessed through a field epidemiological investigation and in-depth interviews with confirmed cases and contacts in the village. Although the last in-person religious activity took place on November 14, 2021, a kimchi making event was conducted in the village for 2 days (November 15–16, 2021). Approximately 60 to 70 villagers who were also religious members participated in this event, and kimchi was delivered to many residents of the village community. After checking villagers’ COVID-19 vaccination status, it was found that 76.1% were not vaccinated, and residents aged 60 years or older accounted for 38.2% of the study population. Therefore, a substantial risk of severe COVID-19 cases was expected. Based on the results of the risk assessment, 2 portable testing clinics were set up in the village where all residents of the village community could undergo rapid testing. Additional door-to-door testing was performed for those who had difficulty visiting the testing clinics. All residents of the village were exposed by close contact; they were instructed to maintain quarantine. They were also closely monitored and tested every 3 days; this interval was chosen considering village residents’ cooperation, laboratory testing capacity, and local government resources. The local government implemented a strict quarantine with controlled access to the village. Further, the administration temporarily closed religious facilities and restricted gatherings. The local government organized and operated an extended care and monitoring team for treatment. In preparation for an emergency, hospital beds were secured and buses were prepared for rapid transfers.
- Study Design and Data Collection and Analysis
- This retrospective cohort study was conducted among residents of a religious village community during a COVID-19 outbreak.
- Data were collected from 602 residents of the village community from epidemiological information registered in the COVID-19 information management system of the KDCA and from the COVID-19 vaccination system. Thirty-one of the confirmed cases resided in other regions and had visited local religious facilities in the past, and 18 cases of secondary infection with contacts from villagers in the religious community were excluded from this study.
- The chi-square test was conducted after performing a descriptive statistical analysis of sex, age, occupation, place of residence (the distance from the location of religious facilities), and the COVID-19 vaccination status of infected and uninfected individuals. Multivariate logistic regression analysis was performed to identify risk factors for COVID-19. Vaccine effectiveness was assessed by analyzing the relevant effects in the unvaccinated and vaccinated subjects. All data were analyzed using IBM SPSS ver. 22.0 (IBM Corp.).
- Ethics Statement
- The study protocol was reviewed and approved by the KDCA Institutional Review Board (IRB No: 2022-11-08-PE-A). The requirement for informed consent was waived by the IRB.
Materials and Methods
- Epidemic Curve
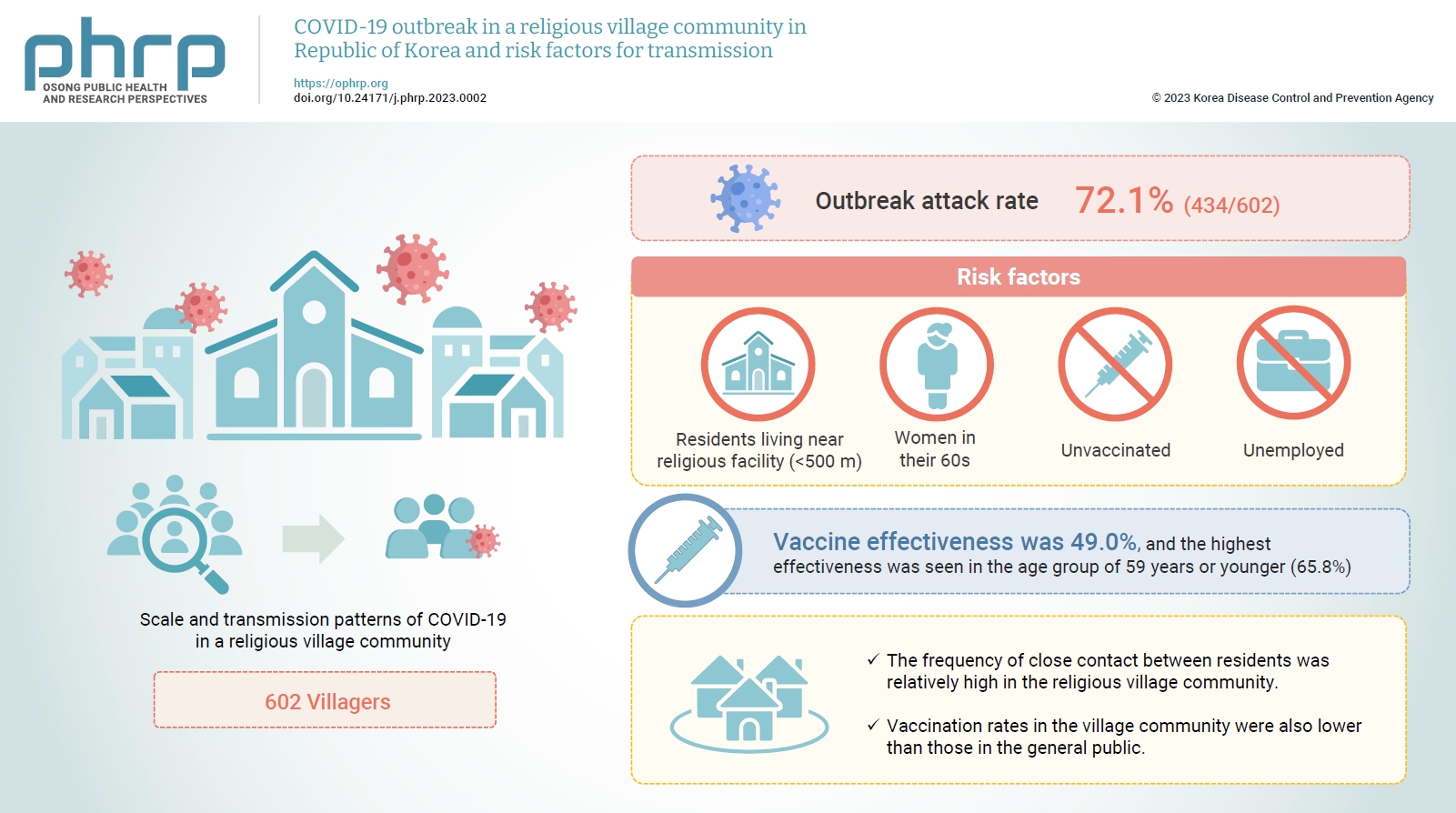
- The suspected primary case had experienced cough, phlegm, and headache since November 13, 2021, and the diagnosis date was November 23, 2021. The suspected primary case’s residence was the same as that of the index case, who was diagnosed on November 21, 2021, after complaining of muscle pain and chills on November 19, 2021. Although the source of infection could not be identified in the suspected primary case, the outbreak in the village community was assumed to have begun on November 11, 2021. The COVID-19 outbreak, triggered by religious activities on November 14, 2021, and village events such as kimchi preparation on November 15 and 16, 2021, resulted in rapid transmission of the virus in the community. The outbreak lasted for 30 days, until December 21, 2021, when the last patient was diagnosed (Figure 1).
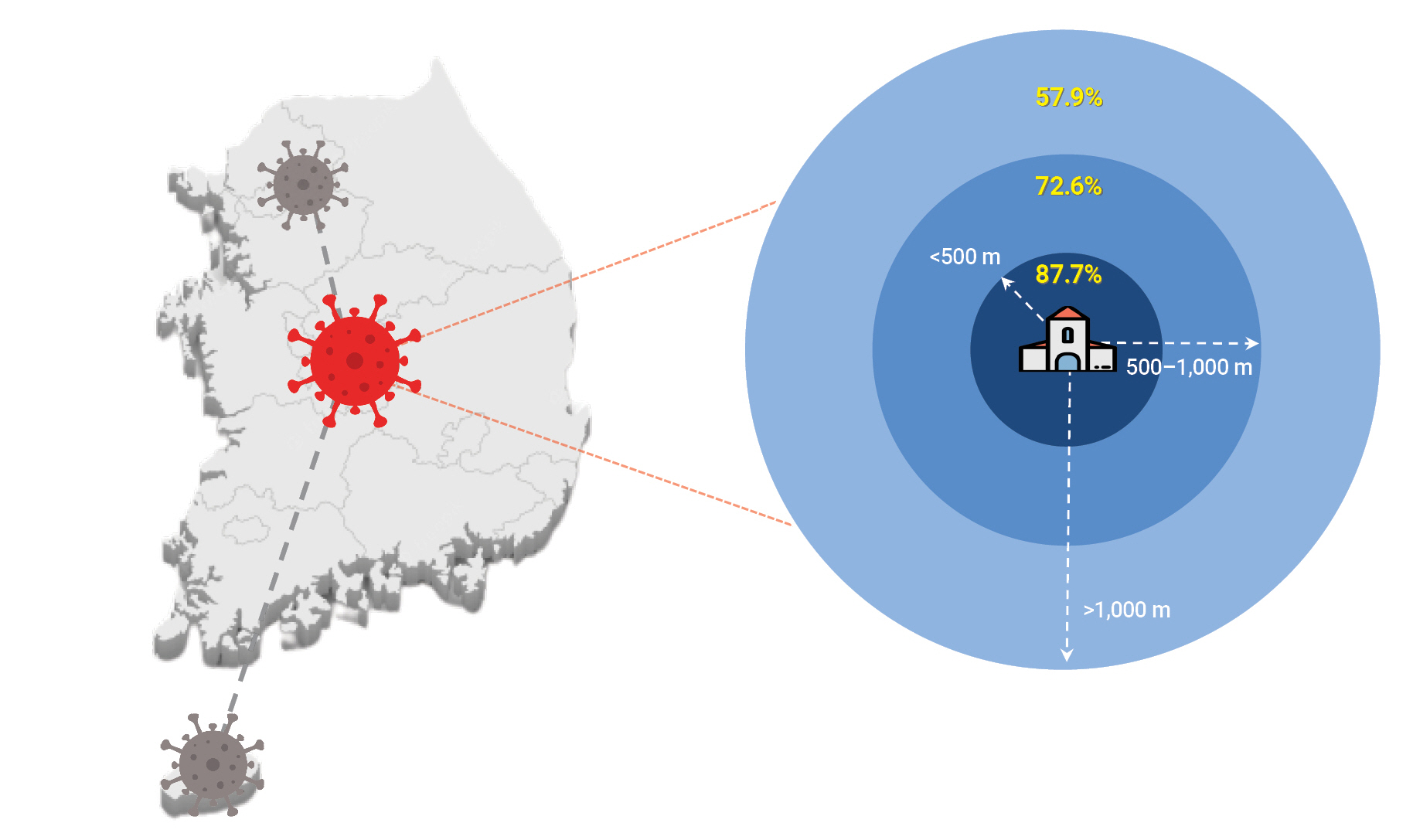
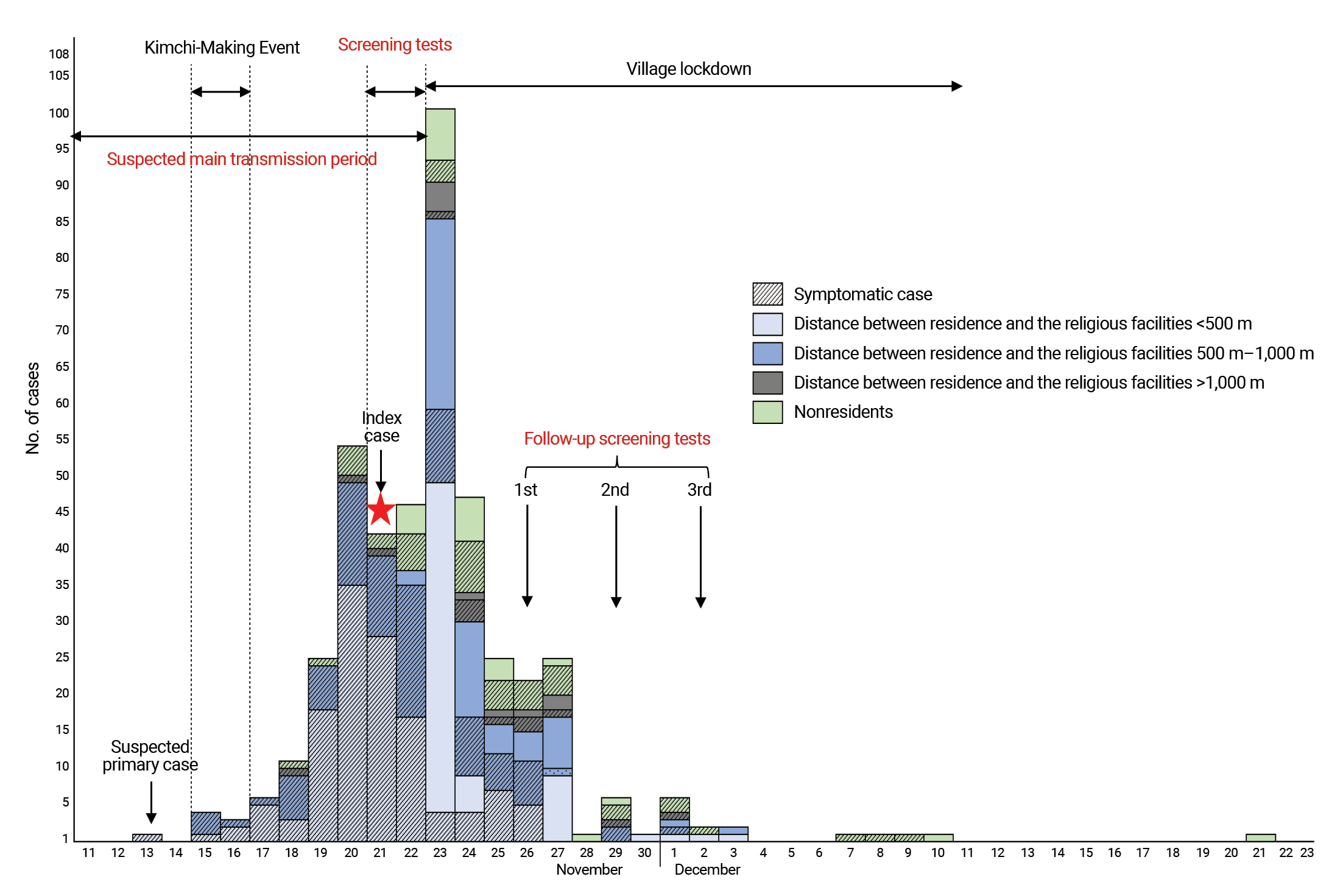
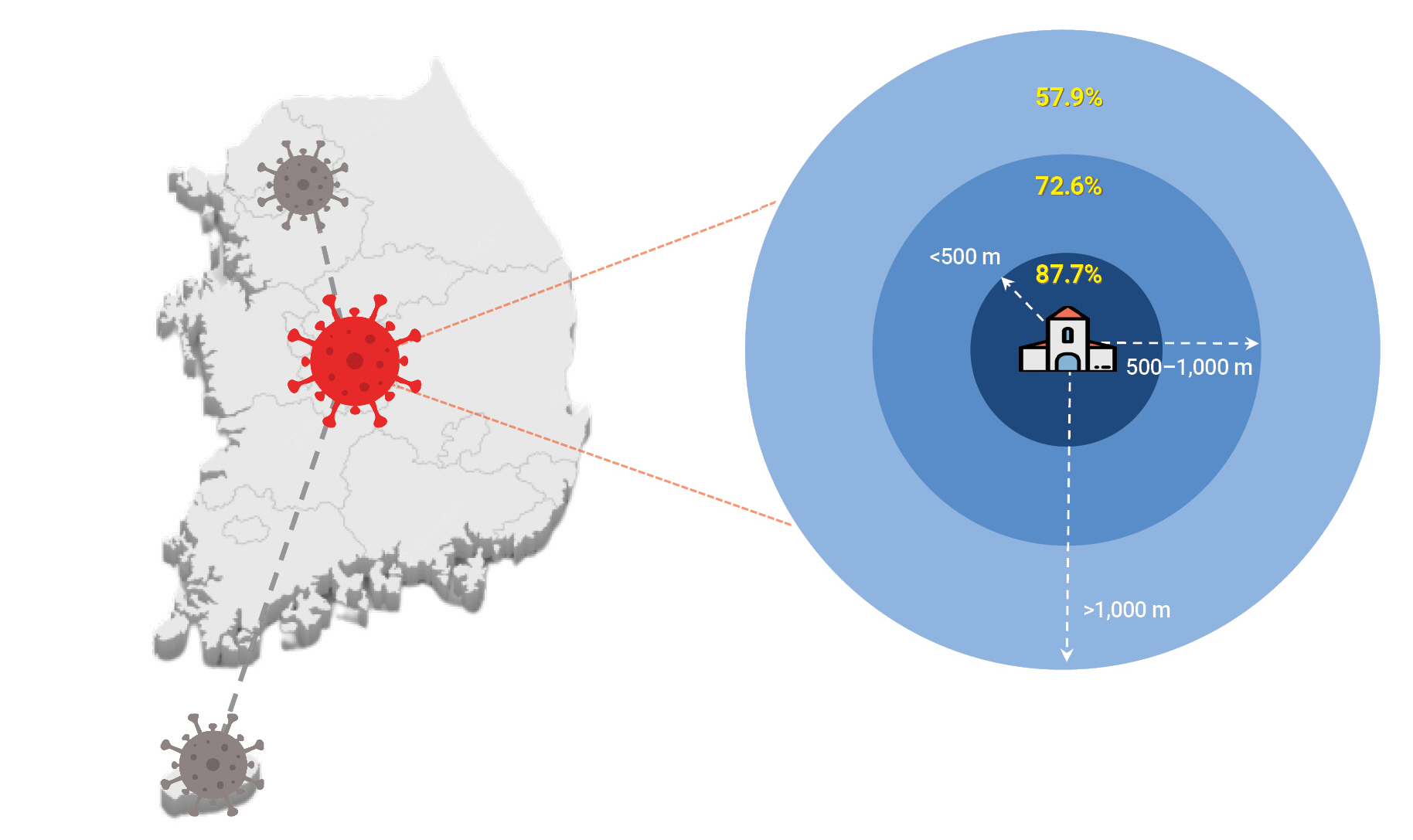
- General Characteristics of the COVID-19 Outbreak in a Religious Community
- Of the 602 residents in the village community, 434 were infected with COVID-19, with an attack rate of 72.1%. The attack rate was 64.6% in male (155/240) and 77.1% in female (279/362) (p<0.001). By age, 252 (67.7%) patients were aged 59 years or younger, 108 (83.7%) were aged 60 to 69 years, and 74 (73.3%) were aged 70 years or older (p=0.002). The COVID-19 patients included 266 (100.0%) unemployed people, 138 (84.7%) employed people, and 173 non-responders (p<0.001). A total of 193 individuals infected with COVID-19 (87.7%) resided within 500 m of the religious facilities, 151 (72.6%) resided within 500 to 1,000 m, and 22 (57.9%) resided more than 1,000 m from the facilities (p<0.001) (Figure 2). There were 374 confirmed cases (81.7%) that were unvaccinated for COVID-19, while 5 confirmed cases (55.6%) had completed the first dose of vaccination. Fifty-five confirmed cases (40.7%) had received the second vaccine dose (p<0.001) (Table 1).
- Risk Factors for COVID-19 Transmission in a Religious Community
- The risk factors for COVID-19 transmission in the village community were identified as age, the distance between religious facility and residences, and vaccination status. Compared with the group aged 59 years or younger, the odds ratio for infection was 6.23 (95% confidence interval [CI], 2.66–14.59) in the group aged 60 to 69 years and 2.89 (95% CI, 1.36–6.16) in those aged 70 years or older. The relative risk of infection was 3.42 times (95% CI, 1.42–8.21) higher in those who lived within 500 m of the religious facilities than in those who lived at more than 1,000 m away. The relative risk of infection was 9.23 times (95% CI, 5.03–16.93) higher in the unvaccinated group than in those who had been vaccinated (Table 2).
- Effectiveness of the COVID-19 Vaccine in the At-risk Population of a Religious Community
- The overall vaccine effectiveness of COVID-19 vaccine was 49.0% after the completion of the second dose (43.9% in males and 51.8% in females). By age, the vaccine effectiveness was 65.8% among those 59 years or younger, 39.8% among those 60 to 69 years old, and 42.0% among those 70 years or older. Furthermore, it was 11.0% in those who lived within 500 m from the religious facilities, 61.2% in those who lived at a distance of 500 to 1,000 m, and 69.6% in those who lived more than 1,000 m from the religious facilities (Table 3).
Results
- This is the first report of a COVID-19 outbreak in a closed religious village community in South Korea. The epidemic lasted for 30 days, from November 21, 2021, when the index case was confirmed, to December 21, 2021. Of the 602 residents in the village community, a total of 434 COVID-19 cases were confirmed. A genetic analysis revealed that this outbreak involved a Delta variant (B.1.167). A cause of extensive transmission within the village was interpersonal exchanges at religious and general village events.
- There were 434 confirmed cases (attack rate: 72.1%); 77.1% of the village’s female population and 64.6% of its male population were infected. The higher attack rate in female residents may have been due to their active participation in religious gatherings such as religious practices and social events such as kimchi making, as shown in previous studies [13]. The attack rate was 73.3% in those 70 years of age or older, 83.7% in those aged 60 to 69 years of age, and 67.7% in those were 59 years of age or younger. Although not shown in the table, the proportion of cases among unemployed individuals increased with age: 126 (49.0%) in those aged 59 years or younger, 75 (77.3%) in those aged 60 to 69 years, and 65 (86.7%) in those aged 70 years or older. Compared to employed individuals, it is reasonable to assume that unemployed residents engaged in village activities for considerably longer time periods and had more opportunities to participate in religious activities [17,18]. Among unemployed residents, the highest incidence was found in those aged 70 and older. However, healthy, unemployed individuals of 60 to 69 of age are presumed to have been most actively involved in religious and village activities, leading them to be exposed most frequently, because unhealthy and unemployed individuals have a limited ability to engage in outside activities [19,20]. Residents were divided into 3 groups according to the distance between their residence and the religious facilities, considering the household distribution and the walking distance. The attack rate was the highest (87.7%) among those who lived within 500 m from the religious facilities, while it was 72.6% in those who resided at a distance of 500 to 1,000 m, and 57.9% in those who lived more than 1,000 m from the facilities. Consistent with a previous study [21] reporting that those who lived closer to a religious facility attended religious services more frequently, the infection rate was higher among residents who lived closer to a religious facility due to frequent participation in religious activities. This was also reflected in the epidemic curve (Figure 1).
- Age, the distance between the religious facility and residences, and vaccination status were identified as risk factors for COVID-19 infection in the village community. In this village, social distancing and quarantine management were not strictly observed due to the nature of religious activities and the prioritization of religious activities over personal activities, frequent social gatherings among the members, and close-contact religious activities. In addition, although the COVID-19 vaccination rate of the general population was close to 70% at the time of the mass outbreak, the vaccination rate in the village was only 24%, which is thought to be the result of misinformation and villagers’ distrust of the vaccination, since they lived in a closed and isolated community.
- The vaccine effectiveness after the completion of the second dose in this study was 49%, which was similar to the effectiveness in a high-risk group in the United Kingdom [22]. However, this finding is significantly lower than the reported vaccine effectiveness of 85% in the general population [23]. In addition, as the distance between religious facility and villagers’ residences increased, vaccine effectiveness increased; this trend may have been influenced by not only the vaccination, but also the decreased likelihood of exposure to virus among those residing further from the facilities.
- COVID-19 vaccination is essential to control the pandemic by forming herd immunity [24]. According to studies on vaccine refusal behavior despite vaccine availability, major factors included fear of disease, concerns about vaccine safety, fear of side effects, distrust of vaccine effectiveness and the healthcare system, attitudes towards vaccination, and a history of influenza vaccination [24–27]. In addition, occupational status, income, health status, religion, and political orientation have been found to influence the decision to receive the vaccination [19,22]. Therefore, health authorities should provide accurate information on the safety and side effects of vaccines through various channels such as social media, and should actively manage fake news. It will also be necessary to foster positive attitudes toward vaccination and elicit vaccination intentions through planned communication to alleviate vaccine fears [9,17]. Because the attitudes of members of religious groups toward vaccines are shaped by their religious beliefs and responses to public health messages from religious leaders [20], religious leaders could positively or negatively influence the health behavior of their followers during an epidemic [9]. In contrast to general religious groups, where religious leaders generally play a positive role, in religious village communities that are closed and separated from the outside world may be more influenced by misbeliefs and misinformation, which could lead tovaccine refusal and uncooperative attitudes to epidemiological investigations [28]. Therefore, active countermeasures such as temporary lockdowns and periodic screening testing during the outbreak could be effective in preventing the transmission of COVID-19. Similar findings have been reported in Taiwan and China, where the spread of infection was prevented by lockdown and quarantine, rapid investigations, screening of villagers, and vaccination in villages with cluster outbreaks of COVID-19 caused by the Delta variant [29,30]. Although coercive and repressive containment measures could quickly stop the spread of infectious diseases, they could also cause humanitarian, psychological, and economic problems. Therefore, agreement and support for the need for containment measures among villagers, the public, and health authorities are needed [29].
- This study has several limitations. Temporary buildings and religious facilities were renovated, and group shelters existed in the community under investigation. However, because of the rejection of the religious community an epidemiological investigation of on-site housing facilities was not allowed, and information collection was limited. In a situation where the number of confirmed cases was rapidly increasing, it was difficult to determine the date of individual exposures and sources of infection because most confirmed cases had participated in religious services and religious activities on multiple occasions.
- Nonetheless, this study described the characteristics of an outbreak in a closed religious village community, identified risk factors for infection, and found evidence of vaccine effectiveness. The findings suggest that religious beliefs and cultures may influence individual and group behaviors related to the spread of COVID-19. The results of this study may have significant implications for containing outbreaks through public health measures. These measures include temporary implementation of lockdown measures, early detection of asymptomatic cases through active screening testing, and the establishment of a treatment system for severe cases the outbreak in a closed village community for religious reasons.
Discussion
- COVID-19 outbreak in a religious village community attack rate was 72.1%. The distance between the religious facility and residences, vaccination status, age were identified as risk factors for the COVID-19 outbreak in village communities.
- The risk of COVID-19 infection was relatively higher in residents who reside within 500m from the religious facility, than residents who reside outside 1,000m from the religious facility.
- This village community had a closed characteristic. The close contact between residents was frequent, contributing to the spread of COVID-19 in the village even with relatively short exposure.
HIGHLIGHTS
-
Ethics Approval
Obtaining informed consent was exempted by the IRB of Korea Disease Control and Prevention Agency (IRB No: 2021-11-08-PE-A) as there was no personal information in the study.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: BIK; Data curation: JS; Formal analysis: JS; Methodology: EL, YC; Project administration: BIK; Resources: JS, GK; Visualization: JS, EK; Writing–original draft: JS, Writing–review & editing: all authors.
-
Additional Information
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Korea Disease Control and Prevention Agency or the institutions with which the authors are affiliated.
Article information
| Characteristic | Total | Infected | Uninfected | Attack rate (%) | p-valuea) | ||
|---|---|---|---|---|---|---|---|
| Total | 602 (100.0) | 434 (100.0) | 168 (100.0) | 72.1 | |||
| Sex | <0.001 | ||||||
| Male | 240 (39.9) | 155 (35.7) | 85 (50.6) | 64.6 | |||
| Female | 362 (60.1) | 279 (64.3) | 83 (49.4) | 77.1 | |||
| Age (y) | 0.002 | ||||||
| ≤59 | 372 (61.8) | 252 (58.1) | 120 (71.4) | 67.7 | |||
| 60–69 | 129 (21.4) | 108 (24.9) | 21 (12.5) | 83.7 | |||
| ≥70 | 101 (16.8) | 74 (17.1) | 27 (16.1) | 73.3 | |||
| Employment (n=429)b) | <0.001 | ||||||
| No | 266 (62.0) | 266 (65.8) | 0 (0.0) | 100 | |||
| Yes | 163 (38.0) | 138 (34.2) | 25 (100.0) | 84.7 | |||
| Residence (n=466)c) | <0.001 | ||||||
| <500 m | 220 (47.2) | 193 (52.7) | 27 (27.0) | 87.7 | |||
| 500–1,000 m | 208 (44.6) | 151 (41.3) | 57 (57.0) | 72.6 | |||
| >1,000 m | 38 (8.2) | 22 (6.0) | 16 (16.0) | 57.9 | |||
| Vaccination status | <0.001 | ||||||
| Unvaccinated | 458 (76.1) | 374 (86.2) | 84 (50.0) | 81.7 | |||
| 1 dose | 9 (1.5) | 5 (1.2) | 4 (2.4) | 55.6 | |||
| 2 doses | 135 (22.4) | 55 (12.7) | 80 (47.6) | 40.7 | |||
Data are presented as n (%).
a) Determined using the chi-square test, unless otherwise specified.
b) People whose occupation was not confirmed were excluded (n=173).
c) Registered people in other regions were excluded based on their residence listed in the resident registration (n=136). Residence: distance from religious facilities.
| Characteristic | n (%) | aORb) | 95% CI | p-value |
|---|---|---|---|---|
| Sex | 434 (100.0) | |||
| Male | 155 (35.7) | Reference | 0.78–2.18 | 0.308 |
| Female | 279 (64.3) | 1.31 | ||
| Age (y) | 434 (100.0) | |||
| ≤59 | 252 (58.1) | Reference | ||
| 60-69 | 108 (24.9) | 6.23 | 2.66–14.59 | <0.001 |
| ≥70 | 74 (17.1) | 2.89 | 1.36–6.16 | 0.006 |
| Residence (n=366)a) | 366 (100.0) | |||
| <500 m | 193 (52.7) | 3.42 | 1.42–8.21 | 0.006 |
| 500–1,000 m | 151 (41.3) | 1.47 | 0.64–3.38 | 0.364 |
| >1,000 m | 22 (6.0) | Reference | ||
| Vaccination status | 434 (100.0) | |||
| Unvaccinated | 374 (86.2) | 9.23 | 5.03–16.93 | <0.001 |
| Vaccinated | 60 (13.8) | Reference |
aOR, adjusted odds ratio; CI, confidence interval.
a) Registered people in other regions were excluded based on their residence listed in the resident registration (n=68). Residence: distance from religious facilities.
b) Odds ratios were calculated by logistic regression after adjustment for sex, age, residence, and vaccination state.
| Vaccination status | Total (n=602) | Infected (n=434) | VE (95% CI) | |||
|---|---|---|---|---|---|---|
| Unvaccinated | Vaccinateda) | Unvaccinated | Vaccinated | |||
| Sex | 458 (76.1) | 144 (23.9) | 374 (86.2) | 60 (13.8) | 49.0 (37.8–58.1) | |
| Male | 164 (68.3) | 76 (31.7) | 123 (79.4) | 32 (20.6) | 43.9 (25.9–57.5) | |
| Female | 294 (81.2) | 68 (18.8) | 251 (90.0) | 28 (10.0) | 51.8 (35.7–63.8) | |
| Age (y) | 458 (76.1) | 144 (23.9) | 374 (86.2) | 60 (13.8) | 49.0 (37.8–58.1) | |
| ≤59 | 307 (82.5) | 65 (17.5) | 235 (93.3) | 17 (6.7) | 65.8 (48.3–77.4) | |
| 60–69 | 86 (66.7) | 43 (33.3) | 83 (76.9) | 25 (23.1) | 39.8 (22.1–53.4) | |
| ≥70 | 65 (64.4) | 36 (35.6) | 56 (75.7) | 18 (24.3) | 42.0 (18.4–58.7) | |
| Occupationb) | 361 (84.1) | 68 (15.9) | 349 (86.4) | 55 (13.6) | 16.3 (5.9–25.6) | |
| No | 228 (85.7) | 38 (14.3) | 228 (85.7) | 38 (14.3) | - | |
| Yes | 133 (81.6) | 30 (18.4) | 121 (87.7) | 17 (12.3) | 37.7 (14.4–54.7) | |
| Residencec) | 373 (80.0) | 93 (20.0) | 321 (87.7) | 45 (12.3) | 43.8 (30.4–46.0) | |
| <500 m | 186 (84.5) | 34 (15.5) | 166 (86.0) | 27 (14.0) | 11.0 (-63.0–25.5) | |
| 500–1,000 m | 162 (77.9) | 46 (22.1) | 136 (90.1) | 15 (9.9.) | 61.2 (42.8–74.4) | |
| >1,000 m | 25 (65.8) | 13 (34.2) | 19 (86.4) | 3 (13.6) | 69.6 (16.1–89.0) | |
aOR, adjusted odds ratio; CI, confidence interval.
a) Vaccinated: Those for whom 14 days had passed since receiving the second dose.
b) People whose occupation was not confirmed were excluded (n=173).
c) Registered people in other regions were excluded based on their residence listed in the resident registration (n=136). Residence: distance from the religious facilities.
- 1. World Health Organization (WHO). Novel coronavirus (2019-nCoV): situation report, 1 [Internet]. WHO; 2021 [cited 2022 Nov 16]. Available from: https://apps.who.int/iris/handle/10665/330760.
- 2. Ahn S, Jang J, Park SY, et al. Outbreak report of COVID-19 during designation of class 1 infectious disease in the Republic of Korea (January 20, 2020 and April 24, 2022). Public Health Wkly Rep 2022;15:1759−72. Korean.
- 3. Prasiska DI, Muhlis ANA, Megatsari H. Effectiveness of the emergency public activity restrictions on COVID-19 epidemiological parameter in East Java Province, Indonesia: an ecological study. Asian J Soc Health Behav 2022;5:33−9.Article
- 4. Shirali GA, Rahimi Z, Araban M, et al. Social-distancing compliance among pedestrians in Ahvaz, South-West Iran during the Covid-19 pandemic. Asian J Soc Health Behav 2021;4:131−6.Article
- 5. European Centre for Disease Prevention and Control (ECDC). SARS-CoV-2 variants of concern as of 15 July 2021 [Internet]. ECDC; 2021 [cited 2022 Nov 16]. Available from: https://www.ecdc.europa.eu/en/covid-19/variants-concern.
- 6. Seppala E, Veneti L, Starrfelt J, et al. Vaccine effectiveness against infection with the Delta (B.1.617.2) variant, Norway, April to August 2021. Euro Surveill 2021;26:2100793. PubMedPMC
- 7. Katella K. 5 things to know about the Delta variant [Internet]. Yale Medicine; 2022 [cited 2021 Oct 13]. Available from: https://www.yalemedicine.org/news/5-things-to-know-delta-variant-covid.
- 8. Johnson AG, Amin AB, Ali AR, et al. COVID-19 Incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence-25 U.S. jurisdictions, April 4-December 25, 2021. MMWR Morb Mortal Wkly Rep 2022;71:132−8.ArticlePubMedPMC
- 9. Tan MM, Musa AF, Su TT. The role of religion in mitigating the COVID-19 pandemic: the Malaysian multi-faith perspectives. Health Promot Int 2022;37:daab041. ArticlePubMedPMCPDF
- 10. Algahtani FD, Alzain MA, Haouas N, et al. Coping during COVID-19 pandemic in Saudi community: religious attitudes, practices and associated factors. Int J Environ Res Public Health 2021;18:8651. ArticlePubMedPMC
- 11. James A, Eagle L, Phillips C, et al. High COVID-19 attack rate among attendees at events at a church-Arkansas, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:632−5.ArticlePubMed
- 12. Cho UJ, Wang S, Yi S, et al. Characteristics of COVID-19 outbreaks and risk factors for transmission at an army training center in South Korea from June to August 2021. Osong Public Health Res Perspect 2022;13:262−72.ArticlePubMedPMCPDF
- 13. Kim JY, Lee YM, Lee H, et al. Epidemiological characteristics of a COVID-19 outbreak caused by religious activities in Daegu, Korea. Epidemiol Health 2021;43:e2021024.ArticlePubMedPMC
- 14. Hasannia E, Mohammadzadeh F, Tavakolizadeh M, et al. Assessment of the anxiety level and trust in information resources among iranian health-care workers during the pandemic of coronavirus disease 2019. Asian J Soc Health Behav 2021;4:163−8.Article
- 15. Sangma RD, Kumar P, Nerli LM, et al. Social stigma and discrimination in coronavirus disease-2019 survivors and its changing trend: a longitudinal study at tertiary care center Gujarat, India. Asian J Soc Health Behav 2022;5:68−74.Article
- 16. Korea Disease Control and Prevention Agency (KDCA). COVID-19 response guidelines for local government (10th) [Internet]. KDCA; 2021 [cited 2022 Apr 1]. Available from: http://www.cncidc.or.kr/user/nd68273.do?View&dmlType=&keyword=&menuCode=krsite&page=3&pageSC=&pageSO=&dmlType=&boardNo=1594&pageSV= Korean..
- 17. Goncalves JPB, Lucchetti G, Menezes PR, et al. Complementary religious and spiritual interventions in physical health and quality of life: a systematic review of randomized controlled clinical trials. PLoS One 2017;12:e0186539.ArticlePubMedPMC
- 18. Koenig HG. Religion, spirituality, and health: a review and update. Adv Mind Body Med 2015;29:19−26.PubMed
- 19. Hwang SE, Kim WH, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccin Immunother 2022;18:1−8.ArticlePubMedPMC
- 20. Garcia LL, Yap JF. The role of religiosity in COVID-19 vaccine hesitancy. J Public Health (Oxf) 2021;43:e529−e530.ArticlePubMedPMCPDF
- 21. Froese P, Uecker J, Vaughan K, Park J, et al. American values, mental health, and using technology in the age of Trump: findings from the Baylor Religion Survey, wave 5. Baylor University;; 2017.
- 22. Whitaker HJ, Tsang RS, Byford R, et al. Pfizer-BioNTech and Oxford AstraZeneca COVID-19 vaccine effectiveness and immune response amongst individuals in clinical risk groups. J Infect 2022;84:675−83.ArticlePubMedPMC
- 23. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med 2021;385:585−94.ArticlePubMedPMC
- 24. Ahorsu DK, Lin CY, Yahaghai R, et al. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum Vaccin Immunother 2022;18:1−8.ArticlePubMedPMC
- 25. Kotecha IS, Vasavada DA, Kumar P, et al. Knowledge, attitude, and belief of health-care workers toward COVID-19 Vaccine at a tertiary care center in India. Asian J Soc Health Behav 2022;5:63−7.Article
- 26. Ahorsu DK, Lin CY, Alimoradi Z, et al. Cyberchondria, fear of COVID-19, and risk perception mediate the association between problematic social media use and intention to get a COVID-19 vaccine. Vaccines (Basel) 2022;10:122. ArticlePubMedPMC
- 27. Fan CW, Chen IH, Ko NY, et al. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother 2021;17:3413−20.ArticlePubMedPMC
- 28. Kim HJ, Hwang HS, Choi YH, et al. The delay in confirming COVID-19 cases linked to a religious group in Korea. J Prev Med Public Health 2020;53:164−7.ArticlePubMedPMCPDF
- 29. Tan X, Song Y, Liu T. Resilience, vulnerability and adaptability: a qualitative study of COVID-19 lockdown experiences in two Henan villages, China. PLoS One 2021;16:e0247383.ArticlePubMedPMC
- 30. Shy CG, Lu JH, Lin HC, et al. Rapid control of a SARS-CoV-2 B. 1.617.2 (Delta) variant COVID-19 community outbreak: the successful experience in Pingtung County of Taiwan. Int J Environ Res Public Health 2022;19:1421. ArticlePubMedPMC
References
Figure & Data
References
Citations



 Cite
Cite