Severe acute respiratory syndrome coronavirus 2 and respiratory syncytial virus coinfection in children
Article information
Abstract
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has infected many people around the world. Children are considered an important target group for SARS-CoV-2, as well as other viral infections such as respiratory syncytial virus infection. Both SARS-CoV-2 and respiratory syncytial virus can affect the respiratory tract. Coinfection of SARS-CoV-2 and respiratory syncytial virus can pose significant challenges in terms of diagnosis and treatment in children. This review compares the symptoms, diagnostic methods, and treatment of COVID-19 and respiratory syncytial virus infection in children.
Introduction
Coronavirus disease 2019 (COVID-19), which causes viral pneumonia, has recently challenged the global healthcare system. COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which belongs to the Coronaviridae family [1]. As it spread rapidly to more than 100 countries all over the world, the World Health Organization declared COVID-19 as a pandemic on March 11, 2020 [2]. Meanwhile, acute lower respiratory tract infections are the cause of death for about 160,000 neonates and more than 760,000 infants annually [3]. Studies have shown that Streptococcus pneumoniae and Haemophilus influenzae type b are common causes of bacterial pneumonia in children [4,5]. Furthermore, postmortem studies of SARS-CoV-2-positive patients have also reported coinfections of SARS-CoV-2 with respiratory viruses such as respiratory syncytial virus (RSV), influenza virus, human bocavirus, parainfluenza virus, and human metapneumovirus [6].
It has been estimated that 22% of episodes of acute lower respiratory infections in children younger than 5 years are associated with RSV [7]. RSV can affect the bronchioles of the lungs. Coinfection of RSV with SARS-CoV-2 can be a key factor in the development, diagnosis, and treatment of COVID-19 in children.
Severe Acute Respiratory Syndrome Coronavirus-2
SARS-CoV-2 affects both the upper and lower respiratory tracts, as well as involving other organs such as the liver, heart, kidney, and brain [8]. Acute lung injury is observed in COVID-19 patients, as well as uncontrolled production of various cytokines and changes in the balance of immune cells, which eventually lead to acute respiratory distress syndrome (ARDS) [9]. Both sexes and all ages are affected by COVID-19, and older individuals and people with underlying diseases are classified as high-risk groups [10]. SARS-CoV-2 can also infect children and infants; although COVID-19 tends to be milder in children than in adults, children can carry and transmit SARS-CoV-2 [11]. Coinfection of SARS-CoV-2 with other respiratory agents can complicate the diagnosis, treatment, and prognosis of COVID-19, as well as increasing patients’ susceptibility (morbidity, symptom severity, and mortality) to COVID-19 [12]. Netea et al. [13] reported that COVID-19 is mild in most cases, although coinfections with other respiratory agents can increase the susceptibility of patients to severe disease.
Respiratory Syncytial Virus
RSV was first identified in chimpanzees in 1955; after a short time, it was confirmed that RSV could be pathogenic in humans. Human RSV is a single-stranded, negative-sense RNA virus that belongs to the genus Pneumovirus in the Pneumoviridae family [14,15]. RSV, which is recognized as one of the most common respiratory viruses that infect children worldwide [16], usually causes bronchiolitis in young children; however, it sometimes can develop into pneumonia. Studies have shown that RSV can infect 90% of children in the first 2 years of life [17]. It has been estimated that RSV annually causes 33 million lower respiratory tract infections, as well as 199,000 deaths in children under 5 years of age in the world [18]. Studies have reported that underlying lung or heart diseases may increase the severity of RSV infection. Premature infants, young children, adults, and older adults with weakened immune systems are at especially high risk for severe illness resulting from RSV [19]. Exposure to smoke is an important environmental risk factor for infant respiratory infections, such as RSV infection [20]. McConnochie and Roghmann [21] reported that exposure to passive smoke may be an important risk factor for bronchiolitis in infants. In RSV infection, host immune responses including cellular immunity and humoral immunity are involved. Cellular immunity plays a key role in the clearance of RSV infection, and the immunopathogenesis of RSV bronchiolitis is affected by cellular immunity. However, neutralizing antibodies against RSV are not stable, and their levels decrease over time [22].
Incidence of COVID-19 and RSV Infection in Children
COVID-19 and RSV infection are both infectious respiratory diseases, but they are caused by different viruses. It has been reported that children have a lower COVID-19 incidence rate than adults [23]. However, the real incidence of COVID-19 in children is unclear because of the lack of widespread diagnostic testing and the prioritization of testing for those with severe disease and adults. Studies showed that hospitalization for COVID-19 is more common among adults than among children, reflecting the higher severe illness rate in adults [24]. The susceptibility rate of children and adolescents to SARS-CoV-2 is lower than that of adults [25].
RSV affects nearly all children in the first 2 years of life. It has been reported that about 0.5% to 2.0% of all children are hospitalized with lower respiratory tract illnesses, of whom 50% to 90% have lung infections and 5% to 40% show pneumonia [26]. RSV can infect people of all age groups, but infants, children under 2 years of age, and elderly people are at particularly high risk [27]. The mortality rate of RSV is higher than that of seasonal influenza infections [28]. In the general population, the frequency of RSV-positive hospitalizations is about 1% to 3%, although the proportion among premature infants is approximately 10% to 25% [29].
Coinfection of RSV and SARS-CoV-2 may have a substantial effect on the treatment and prognosis of the disease. Viral coinfection may be associated with the need for a higher level of care, increased length of stay, and progression to ARDS [30]; furthermore, coinfection can result in more serious damage to the immune system [31]. In other words, patients with COVID-19 and other viruses have a more serious problem, their treatment is more complicated, and their treatment cycle is longer [32]. The progress and outcome of SARS-CoV-2 coinfections with other viruses including RSV are related to the host immune response [33,34].
Several literature reviews have investigated coinfections of SARS-CoV-2 with other respiratory pathogens, such as RSV. Alvares [35] analysed 32 pediatric patients under 24 months of age hospitalized with COVID-19, and found that 18.7% of cases were coinfected with RSV. These patients had a significantly longer length of stay. However, no significant differences were observed in terms of the need for intensive care, mechanical ventilation, or mortality rate. In a study in Wuhan, among 250 patients diagnosed with COVID-19, RSV was detected in 12 patients (4.8%). That study showed that patients coinfected with viral pathogens had longer hospital stays than patients coinfected with atypical bacterial pathogens [36]. In the study of Hazra et al. [37] in 459 SARS-CoV-2-positive cases, there were no positive cases of RSV infection. In a study in Ontario, Canada that included 7,225 SARS-CoV-2-positive cases, 177 (2.4%) were coinfected with RSV. Their results showed that patients with viral coinfections were more likely to be younger than 65 years of age and male, and patients with SARS-CoV-2 coinfections mostly showed mild respiratory signs, including fever and cough [38].
Causes of Viral Coinfection
The mechanisms of viral coinfection may include virus-induced airway damage, reduced mucociliary clearance, and damage to the immune system [39]. Furthermore, several viruses can destroy the airway epithelium, which might lead to enhanced viral coinfection. Virus-associated immune system disorders can increase the risk of infection with other viruses [40,41].
Symptoms of COVID-19 and RSV in Children
The clinical manifestations of COVID-19 are milder in children than in adults [42]; however, fever, cough, diarrhea, nasal congestion, dyspnea, and abdominal pain are the most common symptoms of COVID-19 in children (Figure 1). The incubation period of SARS-CoV-2 is 2–5 days [43,44].
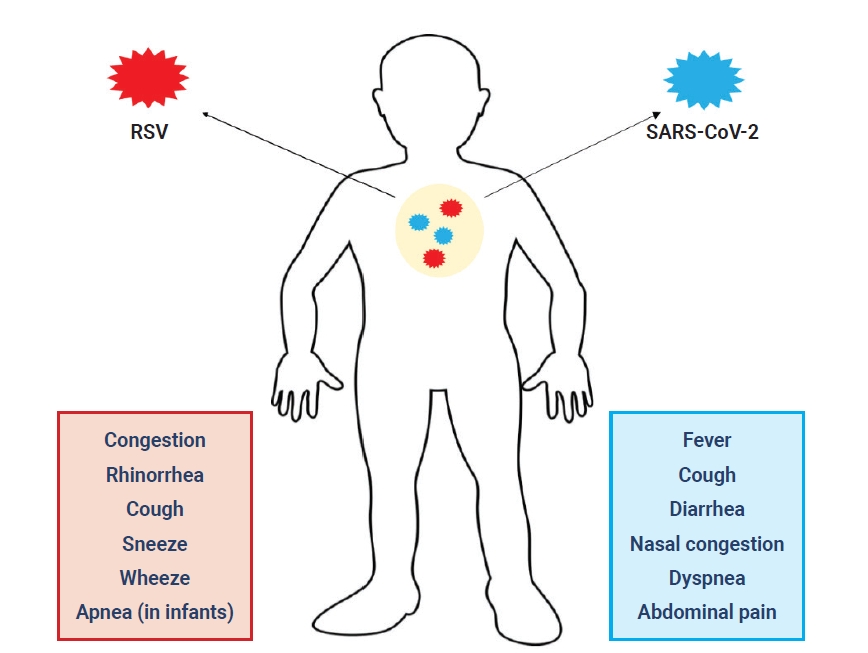
Common symptoms of coronavirus disease 2019 and respiratory syncytial virus (RSV) infection in children. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Multisystem inflammatory syndrome in children (MIS-C) is a hyperinflammatory condition wherein various body parts can become inflamed, such as the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs [25]. MIS-C develops about 2 to 6 weeks after COVID-19 infection. The disease usually affects children with a median age of 8 years [45]. The presenting clinical features in children with MIS-C included persistent fever, abdominal pain, vomiting, diarrhea, cardiac dysfunction, rash, conjunctivitis, headache, and meningismus [46]. Although the specific risk factors for MIS-C are not well understood, it has been hypothesized that lower pre-existing immunity to coronaviruses can elevate individuals’ risk [47]. MIS-C is a progressive disease, and patients who initially have mild symptoms can progress to severe disease with multi-organ dysfunction within a few days of symptom/sign onset. Serious symptoms and signs can include hemodynamic instability, tachycardia, left ventricular dysfunction, and respiratory distress, which might be primary or caused by cardiac dysfunction [48]. The laboratory findings of MIS-C include lymphopenia, anemia, and thrombocytopenia; increased levels of liver enzymes, creatinine, pro-brain natriuretic protein, and troponin; and coagulation [49].
RSV infection in young children is often mild in the early phase, but in children under 3 years of age, RSV may cause coughing, wheezing, congestion, rhinorrhea, sneezing, and apnea [49]. RSV is the most common cause of bronchiolitis and pneumonia in children under 1 year of age, and the incubation period of RSV is about 2 to 8 days [50]. In children, RSV can lead to severe respiratory disease requiring hospitalization, and causes death in some rare cases. Other RSV symptoms common among infants include listlessness, poor or diminished appetite, and fever [16–18]. RSV and COVID-19 coinfection may increase the severity of disease in children.
SARS-CoV-2 and RSV Diagnosis in Children
The early and accurate diagnosis of SARS-CoV-2 is an important tool for limiting and controlling COVID-19. Contact with infected individuals is a key way to transmit SARS-CoV-2 in both children and adults [51].
Molecular and serological tests are recommended by the Centers for Disease Control and Prevention to diagnose patients with SARS-CoV-2 infection. COVID-19 can result in significant alterations in the white blood cell count, elevated number of neutrophils and decreased number of lymphocytes have been reported in patients with severe COVID-19 [52]. Some laboratory predictors of COVID-19 have been identified in children, including increased or decreased levels of markers such as procalcitonin, D-dimer, and creatine kinase, as well as elevated liver enzymes [41].
The radiological imaging findings of COVID-19 pneumonia include lung changes (e.g., ground-glass opacities), bronchial changes, and pleural changes. However, the symptoms and radiological findings are similar to other respiratory viral infections [53]. Hence, determining the type and number of viruses present in a patient based on imaging findings and the medical history may be difficult, and misdiagnoses of COVID-19 and other respiratory viruses are possible. Radiographic images and clinical signs can only be used as diagnostic auxiliaries, and patients cannot be diagnosed solely on the basis of these 2 modalities [54].
Analyses of laboratory findings have shown that SARS-CoV-2 infection was associated with lymphopenia, prolonged prothrombin time, and elevated levels of lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, D-dimer, neutrophils, eosinopenia, C-reactive protein, and troponin [55]. The most common laboratory data include a decreased lymphocyte count and increased high-sensitivity C-reactive protein levels. When combined with other viral infections, these results might change. Laboratory finding results are often influenced by the degree of disease progression and the pathogens that infect the patient, so they can only be used as a reference for diagnosing the disease [56]. Multiplex reverse transcription-polymerase chain reaction can simultaneously detect respiratory viruses such as SARS-CoV-2 and RSV. Nevertheless, this technique may cause some false-negative results because of certain factors during sample recovery, processing, or transportation. Thus, repeat nasopharyngeal testing is important for confirming the diagnosis [57].
Computed tomography (CT) is used as another diagnostic tool for SARS-CoV-2, but it is less specific in children than in adults. The radiologic results in children with COVID-19 include unilateral or bilateral infiltrates and ground-glass opacities on CT [58].
Two main predictors are important for the diagnosis of RSV infection: the physical examination and patient history. Children typically present with cough, rhinitis, and wheezing. Laboratory testing and chest radiography are not required for a diagnosis. The white blood cell count is not abnormal, but it may be increased in some cases. The results of chest radiography in children with bronchiolitis sometimes are abnormal [59]. Thus, laboratory tests and chest radiography are not routinely recommended for RSV infection.
SARS-CoV-2 and RSV Treatment in Children
Combinations of antiviral agents and immunomodulators (oseltamivir + hydroxychloroquine + Kaletra [lopinavir + ritonavir]) are used to treat COVID-19 pneumonia in children [60], while RSV treatment is based on supportive care; however, palivizumab is recommended to prevent serious complications of RSV infection. Supportive care is the key treatment for RSV bronchiolitis [61]. Most infants can be managed at home, although hospitalization is necessary for children with RSV infection who are ill-appearing, have poor feeding, are dehydrated, have apnea, develop respiratory distress, or require supplemental oxygen [61].
Supportive care includes hydration, using saline nose drops to clear nasal obstruction, suction with a nasal bulb in the hospital, and adequate nutrition for the patient. Oxygen is recommended in some cases to keep oxygen saturation >90% [62]. Mechanical ventilation is needed in some otherwise healthy infants with RSV infection who are hospitalized and infants with underlying diseases such as chronic lung disease, congenital heart disease, or immunosuppression [63].
Conclusion
Both SARS-CoV-2 and RSV are infectious causes of respiratory disease in children. RSV and SARS-COV-2 coinfection in children can be considered a serious problem in the context of the COVID-19 pandemic. The pathogenicity of SARS-CoV-2 in children is unclear, but coinfection of RSV with SARS-CoV-2 may promote severe disease in children, as well as affecting the diagnosis and treatment of disease. Although several studies have investigated viral respiratory coinfections in COVID-19 patients, no study has evaluated the rate of RSV coinfection in SARS-CoV-2-positive samples from children. The clinical data of SARS-CoV-2 coinfection are of considerable value for the treatment of COVID-19. In patients with severe COVID-19, the rate of coinfections (e.g., RSV infection) is significantly higher than in those who have not been severely affected. Therefore, it is very important to prevent coinfection with SARS-CoV-2 and other viruses, including RSV, as a step towards preventing and controlling the spread of COVID-19. To prevent transmission, social distancing must be encouraged. In the process of diagnosing and treating patients with other viral infections, it is best to provide a separate room for specific individuals in the clinical setting so that they can be isolated and treated after evaluating the risk of transmission. These actions facilitate the accurate prevention and treatment of infectious complications and effective reduction of mortality in patients with COVID-19.
Notes
Ethics Approval
Not applicable.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding
The current study was financially supported by Abadan University of Medical Sciences (Ethics No: IR.ABADANUMS.REC.1399.218).
Availability of Data
All data generated or analyzed during this study are included in this published article. For other data, these may be requested through the corresponding author.
Additional Contributions
Conceptualization: MZ; Data curation: SS, MF, SE; Investigation: SS, MF, AR; Supervision: SA; Writing–original draft: SS, MF, AR; Writing–review & editing: MZ, SA.
