Previous issues
- Page Path
- HOME > Articles and issues > Previous issues
Editorial
- To become a more stronger and safer country
- Jong-Koo Lee
- Osong Public Health Res Perspect. 2023;14(2):67-69. Published online April 28, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0105
- 996 View
- 45 Download
Review Article
- Points to consider when developing drugs for dry eye syndrome
- Suyoung Bae, Hosun Seung, Ho Jung Oh
- Osong Public Health Res Perspect. 2023;14(2):70-75. Published online April 26, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0031
- 1,555 View
- 113 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 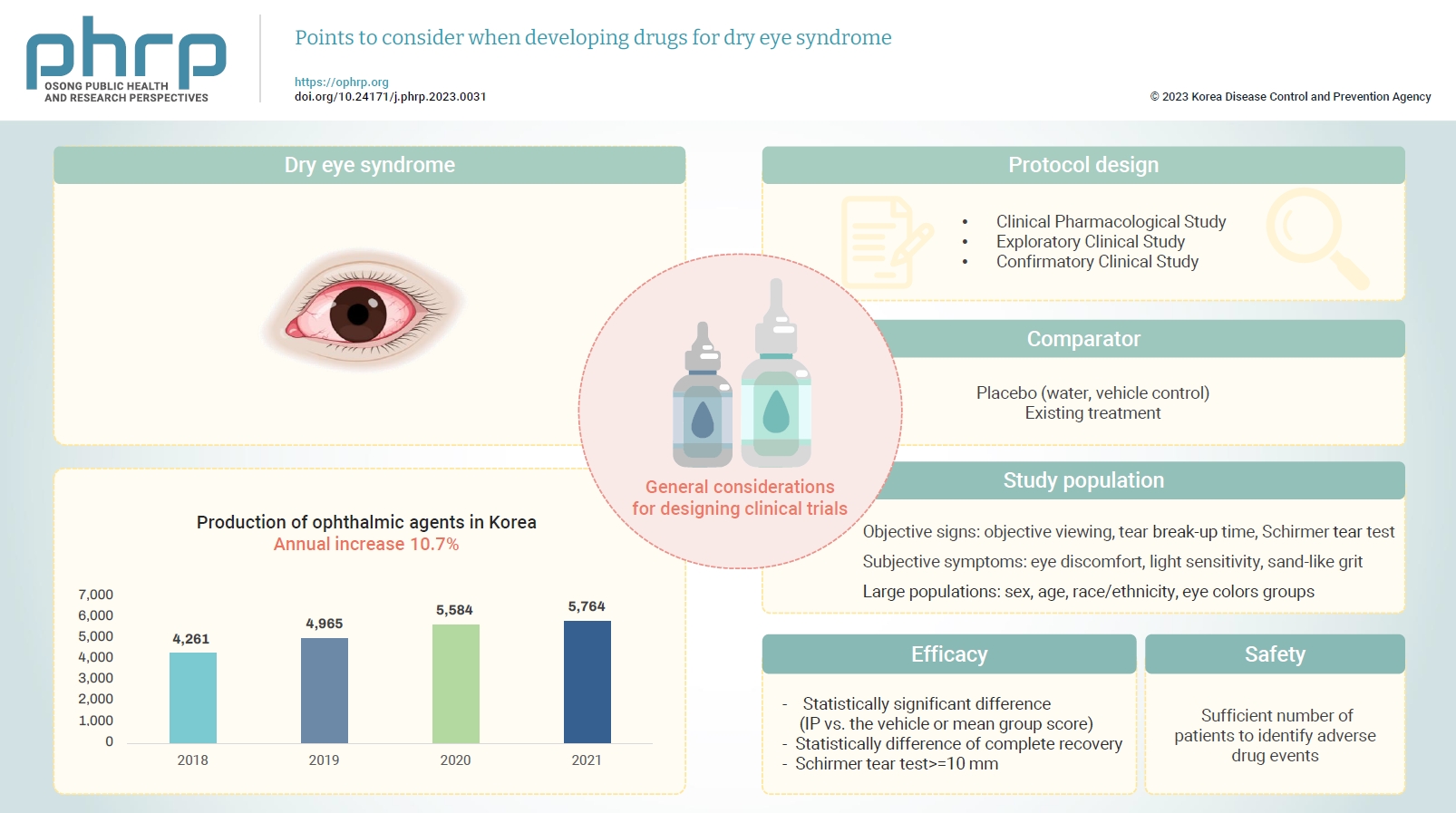
- Changes in both the social environment (e.g., the increased use of electronic media) and the atmospheric environment (e.g., air pollution and dust) have contributed to an increasing incidence of eye disease and an increased need for eye care. Notably, the signs and symptoms of dry eye syndrome can impact the daily quality of life for various age groups, including the elderly, and usually requires active treatment. The symptoms of dry eye syndrome include tear film instability, hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities. As treatments for dry eye are being developed, a standardized guideline is needed to increase the efficiency of drug development and improve the quality of clinical trial data. In this paper, we present general considerations for the pharmaceutical industry and clinical trial investigators designing clinical trials focused on the development of drugs to treat dry eye syndrome.
Original Articles
- The incidence and clinical characteristics of myocarditis and pericarditis following mRNA-based COVID-19 vaccination in Republic of Korea adolescents from July 2021 to September 2022
- Ju-Young Sim, Seung-Yun Kim, Eun-Kyoung Kim
- Osong Public Health Res Perspect. 2023;14(2):76-88. Published online April 18, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0032
- 3,984 View
- 231 Download
- 2 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 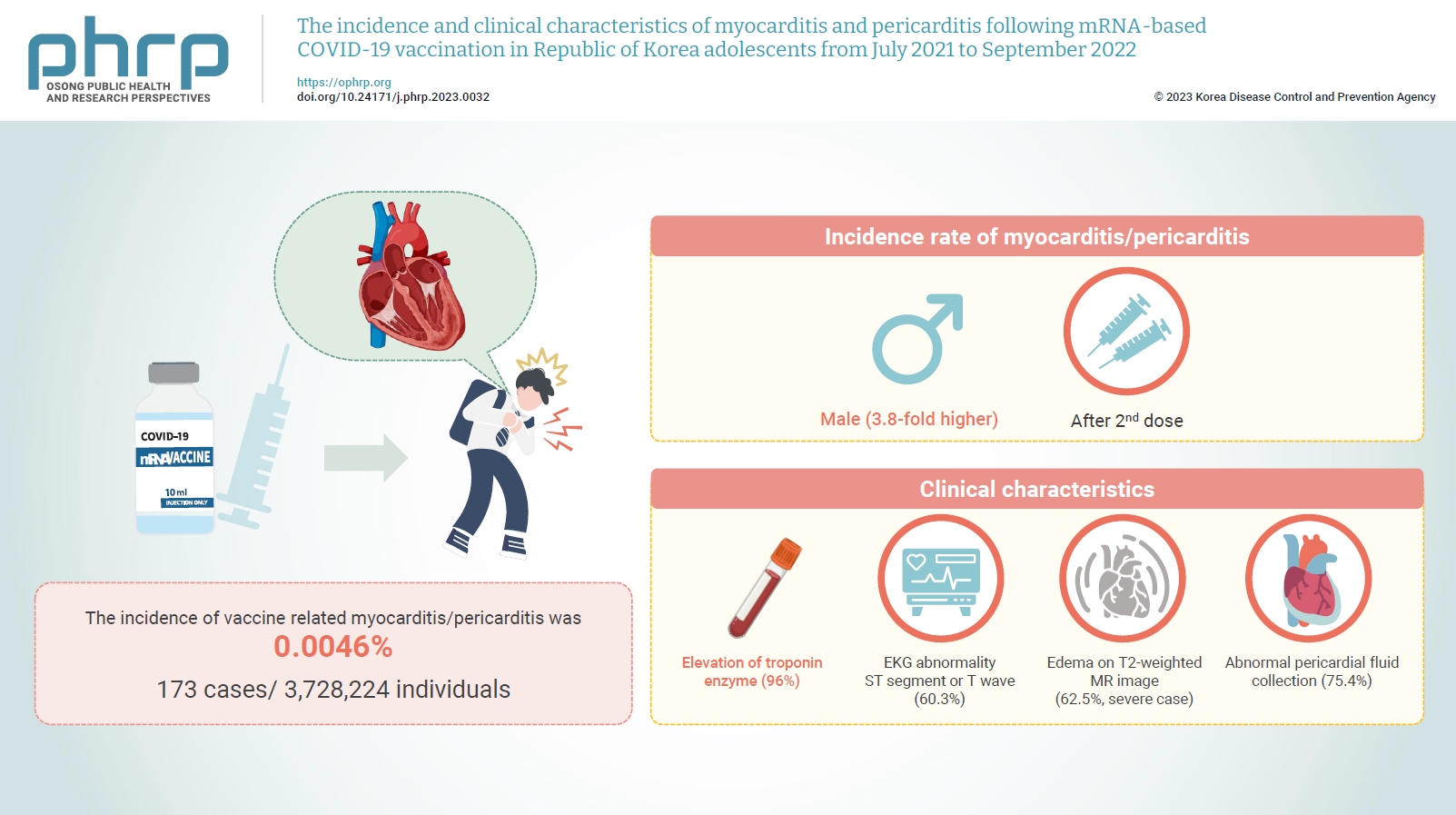
- Objectives
Age-specific information regarding myocarditis/pericarditis in adolescents following mRNA-based coronavirus disease 2019 (COVID-19) vaccination in Asia remains insufficient. This study investigated the incidence and clinical characteristics of myocarditis/pericarditis in Republic of Korea adolescents after mRNA-based COVID-19 vaccination.
Methods
This retrospective descriptive study utilized patient data from the Korea Immunization Management System. Incidence rates were calculated according to age and sex. Clinical characteristics (symptoms/signs, laboratory values, and imaging results) were compared between mild and severe cases.
Results
Between July 19, 2021 and September 30, 2022, 3,728,224 individuals aged 12 to 19 years received 6,484,165 mRNA-based COVID-19 vaccines, and 173 cases met the case definition for myocarditis/pericarditis: 151 mild (87.3%) and 22 severe (12.7%). The incidence was 3.8-fold higher in males than in females. Troponin I/ troponin T was elevated in 96% of myocarditis cases, demonstrating higher sensitivity than creatine kinase-myocardial band (67.6%) or C-reactive protein (75.2%). ST-segment or Twave on electrography abnormalities were found in 60.3% (85/141). Paroxysmal/sustained atrial/ventricular arrhythmias were more common in severe than in mild cases (45.5% vs. 16.8%, p=0.008). Edema on T2-weighted magnetic imaging occurred in 21.6% (8/37) and 62.5% (5/8) of mild and severe cases, respectively (p=0.03). Abnormal pericardial fluid collection or pericardial inflammation was found in 75.4% of pericarditis cases (49/65).
Conclusion
Myocarditis/pericarditis occurred in rare cases following mRNA-based COVID-19 vaccination. Most cases were mild, but the incidence was higher in adolescent males and after the second dose. As bivalent severe acute respiratory syndrome coronavirus 2 mRNA vaccination started in Republic of Korea in October 2022, the post-vaccination incidence of myocarditis/pericarditis should be closely monitored, considering clinical characteristics. -
Citations
Citations to this article as recorded by- Responses to Common Misconceptions Relating to COVID-19 Variant-Adapted mRNA Vaccines
George Kassianos, Pauline MacDonald, Ivan Aloysius, Shanti Pather
Vaccines.2024; 12(1): 57. CrossRef - To become a more stronger and safer country
Jong-Koo Lee
Osong Public Health and Research Perspectives.2023; 14(2): 67. CrossRef
- Responses to Common Misconceptions Relating to COVID-19 Variant-Adapted mRNA Vaccines
- Risk factors for deaths associated with COVID-19 according to the cause of death classification in Republic of Korea
- Na-Young Kim, Seong-Sun Kim, Hyun Ju Lee, Dong Hwi Kim, Boyeong Ryu, Eunjeong Shin, Donghyok Kwon
- Osong Public Health Res Perspect. 2023;14(2):89-99. Published online April 18, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0312
- 1,443 View
- 93 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
This study aimed to classify coronavirus disease 2019 (COVID-19)-related deaths according to whether COVID-19 was listed as the cause of death, and to investigate the differences in demographic characteristics and risk factors for COVID-19 death classifications.
Methods
A total of 5,625 deaths in South Korea among patients with confirmed COVID-19 from January 20, 2020 to December 31, 2021 were selected. Excluding false reports and unnatural deaths, 5,597 deaths were analyzed. Based on death report data, deaths were classified according to whether the cause of death was listed as COVID-19 (CD) or not (NCD). The epidemiological characteristics and causes of deaths were investigated using descriptive, univariate, and multivariate statistical analyses. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to analyze the risk factors.
Results
The case fatality ratio was 0.89% and increased with age. Additionally, 96.4% of the subjects had an underlying disease, and 53.4% died in winter. The proportion of NCDs was 9.3%, of whom 19.1% died at home and 39.0% were confirmed to have COVID-19 after death. Malignant neoplasms (102/416 vs. 637/4,442; OR, 1.71; 95% CI, 1.36−2.16; p<0.001) were significantly associated with NCD.
Conclusion
This is the first study to analyze risk factors by cause of death using COVID-19 death report data in South Korea. These results are expected to be used as evidence for establishing a death monitoring system that can collect timely information in a new infectious disease pandemic.
- Vaccine hesitancy in patients with COVID-19 who have back pain
- Askeri Türken, Haşim Çapar
- Osong Public Health Res Perspect. 2023;14(2):100-109. Published online March 24, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0003
- 1,806 View
- 70 Download
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 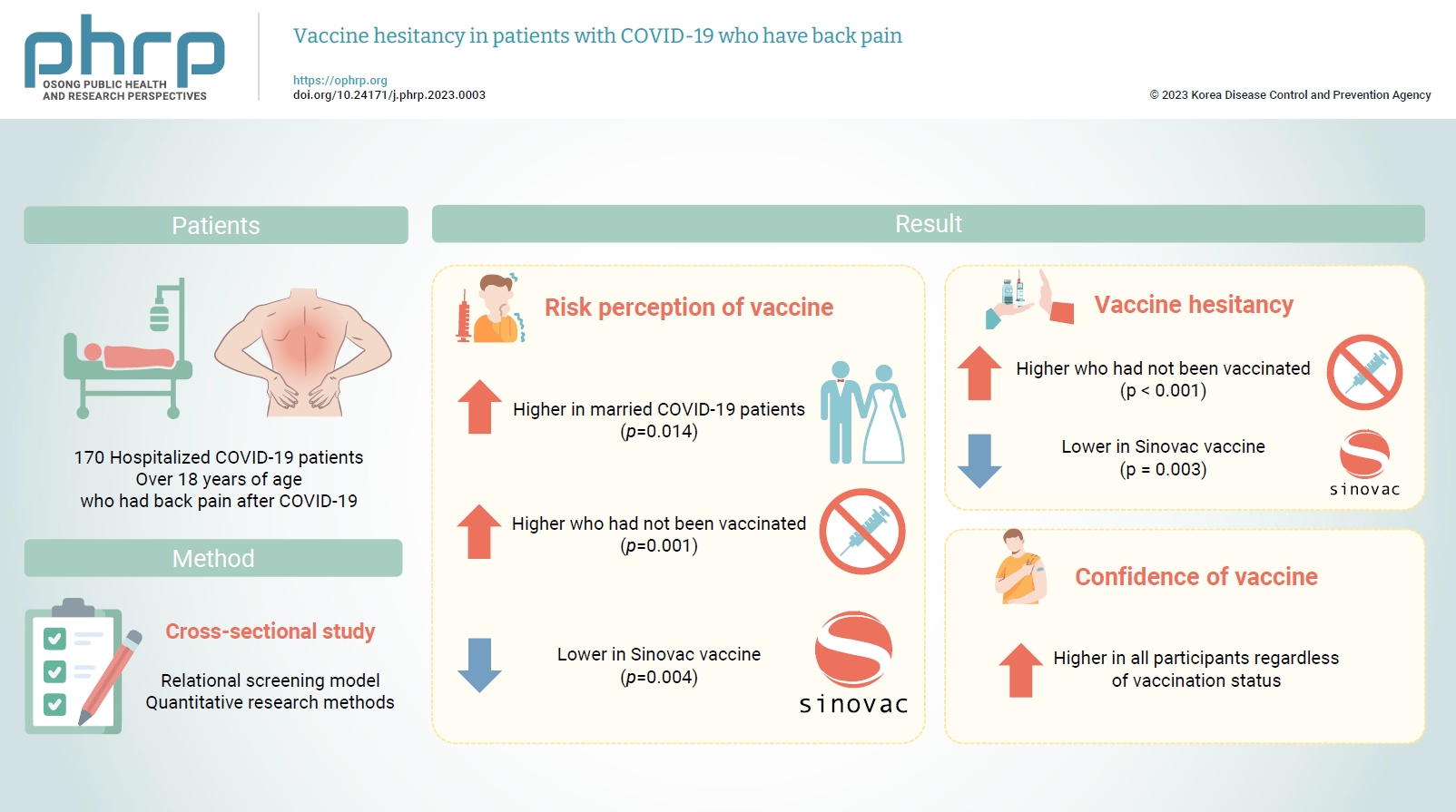
- Objectives
Musculoskeletal pain is among the most common symptoms in patients diagnosed with coronavirus disease 2019 (COVID-19), and it has placed a significant burden on health worldwide during the pandemic. This study explored vaccine hesitancy and associated factors in patients with positive COVID-19 polymerase chain reaction test results who were hospitalized and had back pain.
Methods
A cross-sectional study was conducted among 170 hospitalized COVID-19 patients over 18 years of age. Data were analyzed using descriptive statistics with IBM SPSS ver. 25.0.
Results
COVID-19 patients who were married considered COVID-19 vaccinations riskier than unmarried COVID-19 patients. Patients who had not been vaccinated expressed higher levels of distrust towards COVID-19 vaccines than patients who had been vaccinated. Participants had relatively little hesitation toward the Sinovac vaccine. High vaccine confidence was found in all participants regardless of vaccination status. Those who had not received the COVID-19 vaccine reported higher risk perceptions than those who had received at least 1 dose of any COVID-19 vaccine.
Conclusion
Measurements of the hesitancy of vaccinated and non-vaccinated patients or members of society towards vaccines can be an important parameter for health authorities to find solutions. -
Citations
Citations to this article as recorded by- COVID-19 VE DAVRANIŞSAL İKTİSAT: KÜRESEL BİR PANDEMİ SIRASINDA İNSAN DAVRANIŞINI ANLAMAK
İlknur ARSLAN ARAS
Sağlık ve Sosyal Refah Araştırmaları Dergisi.2024; 6(1): 97. CrossRef
- COVID-19 VE DAVRANIŞSAL İKTİSAT: KÜRESEL BİR PANDEMİ SIRASINDA İNSAN DAVRANIŞINI ANLAMAK
- COVID-19 outbreak in a religious village community in Republic of Korea and risk factors for transmission
- Jiae Shim, Eunju Lee, Eunyoung Kim, Yeonhwa Choi, Giseok Kang, Bryan Inho Kim
- Osong Public Health Res Perspect. 2023;14(2):110-118. Published online April 5, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0002
- 1,497 View
- 72 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 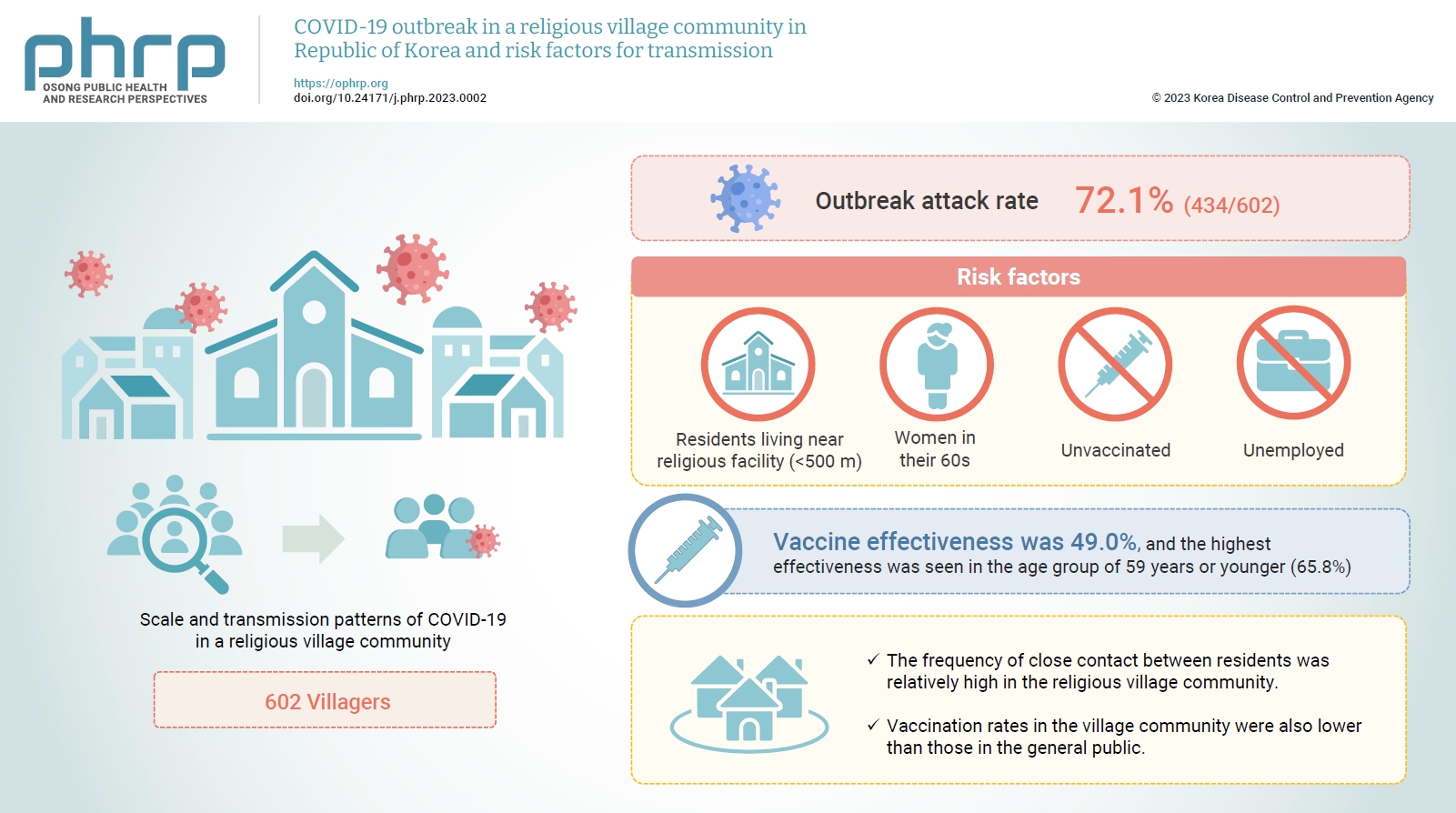
- Objectives
This study aimed to assess the scale and transmission patterns of coronavirus disease 2019 (COVID-19) in a religious village community in South Korea, to determine the risk factors of transmission, and to evaluate vaccine effectiveness.
Methods
An epidemiological survey was conducted, and data were collected and analyzed from 602 villagers in the religious village community. Multivariate logistic regression analysis was used to identify the risk factors for COVID-19 transmission and to evaluate vaccine effectiveness.
Results
The outbreak attack rate was 72.1% (434/602). The attack rate was high among women in their 60s, the unemployed, residents living near religious facility (<500 m), and the unvaccinated. Age, the distance between religious facility and residences, and the absence of vaccination were identified as risk factors for transmission. Vaccine effectiveness was 49.0%, and the highest effectiveness was seen in the age group of 59 years or younger (65.8%).
Conclusion
This village community was isolated, with little communication with the outside world. However, the frequency of close contact between residents was relatively high, contributing to the spread of COVID-19 in the village even with relatively short exposure. Vaccination rates in the village community were also lower than those in the general public. Public health authorities should consider the potential impact of cultural factors, including religion, that could lead to the exponential spread of COVID-19 in closed village communities.
- Quality of life in patients treated for COVID-19–associated mucormycosis at a tertiary care hospital
- Pragya Kumar, Rajath Rao UR, Nilanjan Roy, Deepika Agrawal, Shamshad Ahmad, Kranti Bhavana
- Osong Public Health Res Perspect. 2023;14(2):119-128. Published online April 18, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0307
- 1,980 View
- 57 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 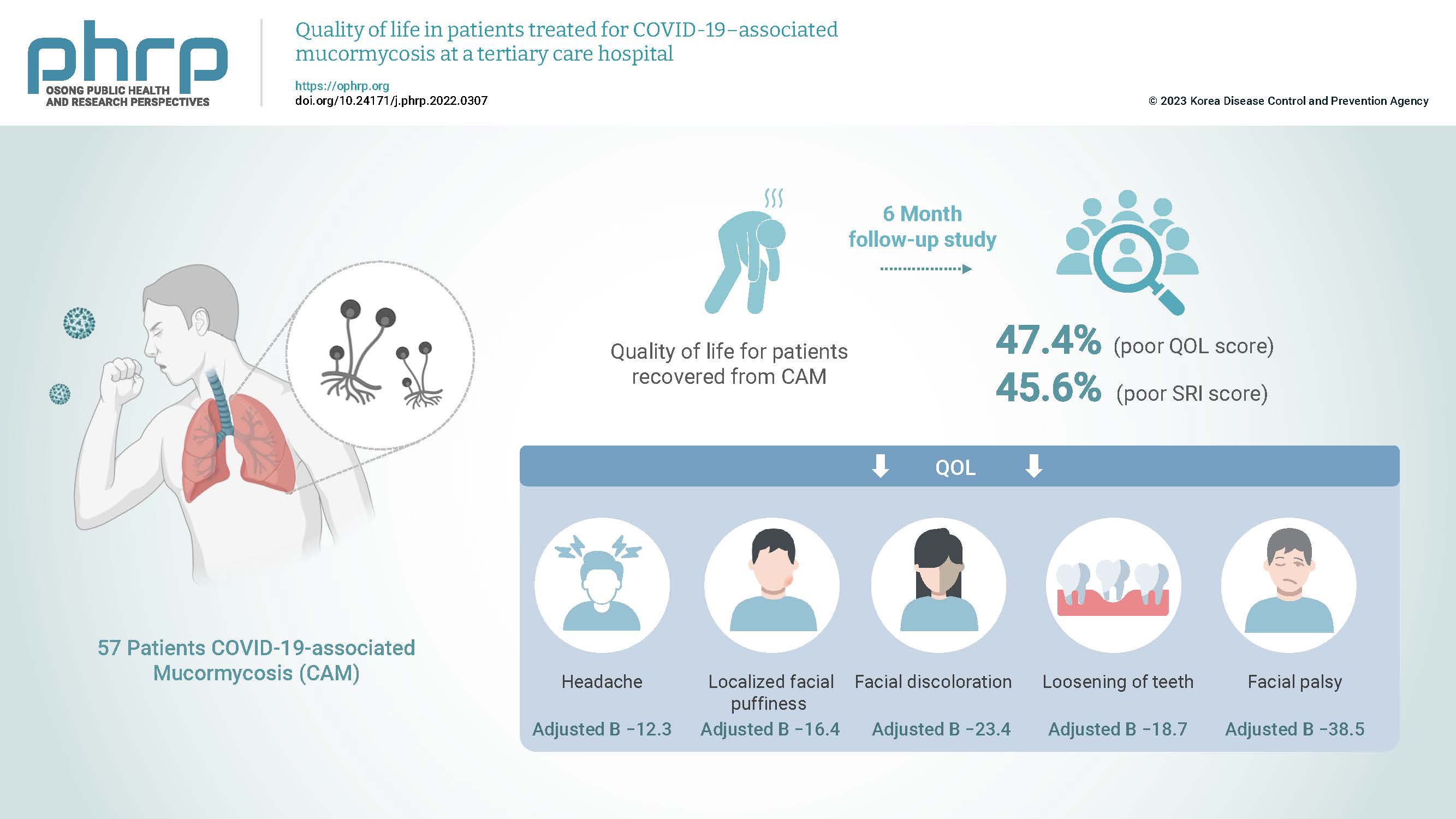
- Objectives
Coronavirus disease 2019 (COVID-19)–associated mucormycosis (CAM) has emerged as a formidable infection in patients with COVID-19. The aggressive management of CAM affects quality of life (QOL); thus, this study was designed to assess the QOL in patients with CAM at a tertiary healthcare institution.
Methods
This cross-sectional study of 57 patients with CAM was conducted over 6 months using a semi-structured standard questionnaire (the abbreviated World Health Organization Quality of Life questionnaire [WHO-BREF]) and a self-rated improvement (SRI) scale ranging from 0 to 9. Cut-off values of ≤52 and <7 were considered to indicate poor QOL and poor improvement, respectively. The correlations of QOL and SRI scores were evaluated using Spearman rho values.
Results
In total, 27 patients (47.4%; 95% confidence interval [CI], 34.9%–60.1%) and 26 patients (45.6%; 95% CI, 33.4%–58.4%) had poor QOL and poor SRI scores, respectively. The overall median (interquartile range) QOL score was 52 (41–63). Headache (adjusted B, −12.3), localized facial puffiness (adjusted B , −16.4), facial discoloration (adjusted B, −23.4), loosening of teeth (adjusted B, −18.7), and facial palsy (adjusted B, −38.5) wer e significantly associated with the QOL score in patients with CAM.
Conclusion
Approximately 1 in 2 patients with CAM had poor QOL and poor improvement. Various CAM symptoms were associated with QOL in these patients. Early recognition is the key to optimal treatment, improved outcomes, and improved QOL in patients with CAM.
- Analysis of pregnant women with critically severe COVID-19 in Republic of Korea from February 2020 and December 2021
- Ji Joo Lee, Sang-Eun Lee, Yeonjung Kim, Young-Joon Park
- Osong Public Health Res Perspect. 2023;14(2):129-137. Published online April 5, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0025
- 1,295 View
- 58 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 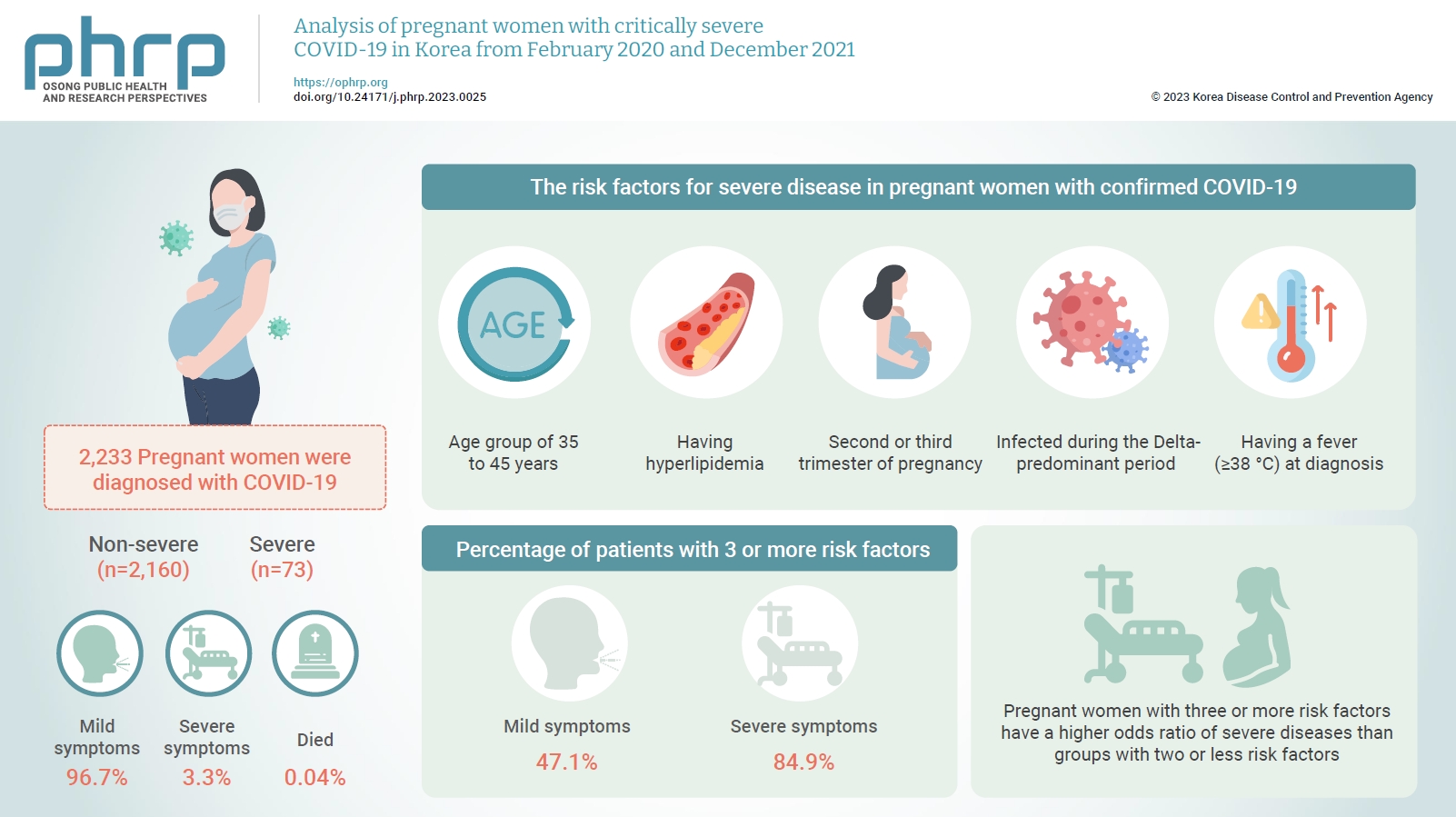
- Objectives
This study aimed to describe the characteristics and risk factors for severe disease in pregnant women infected with coronavirus disease 2019 (COVID-19) from the early days of the COVID-19 epidemic in Korea to the predominant period of the Delta variant.
Methods
A retrospective cohort study was conducted among pregnant women diagnosed with COVID-19 between February 2020 and December 2021. Logistic regression analysis was performed to compare severe and mild cases after adjusting for pregnant women’s age, nationality, infection route, outbreak area, infection period, symptoms, underlying disease, smoking status, trimester, and COVID-19 vaccination status.
Results
In total, 2,233 pregnant women were diagnosed with COVID-19 by December 2021. Among these, 96.7% had mild symptoms, 3.3% had severe symptoms, and 0.04% died. The risk factors for severe disease in pregnant women with confirmed COVID-19 were being in the age group of 35 to 45 years, having hyperlipidemia, being in the second or third trimester of pregnancy at the time of COVID-19 diagnosis, being infected during the Delta-predominant period, and having a fever (≥38 °C) at diagnosis. Furthermore, 47.1% of patients in the mild group and 84.9% of patients in the severe group had 3 or more risk factors.
Conclusion
Pregnant women with COVID-19 mainly experienced mild symptoms, but those with risk factors were at a higher risk of developing severe symptoms. Therefore, treatment and follow-up management should be thoroughly implemented.
- Estimated impact of the national hepatitis B immunization program on acute viral hepatitis B among adolescents in Republic of Korea
- Chungman Chae, Sangwoo Tak
- Osong Public Health Res Perspect. 2023;14(2):138-145. Published online March 24, 2023
- DOI: https://doi.org/10.24171/j.phrp.2022.0321
- 1,528 View
- 62 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 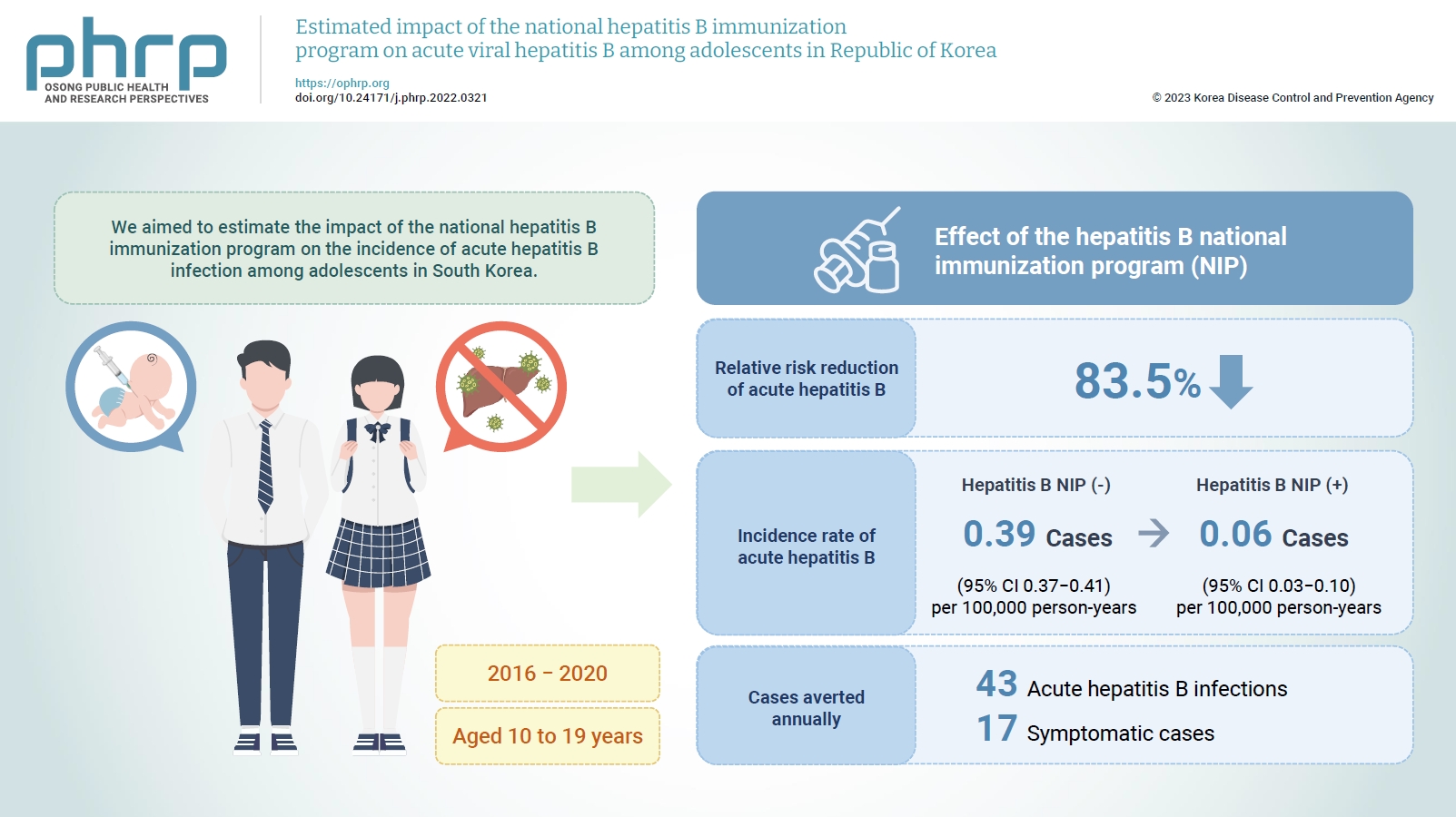
- Objectives
We aimed to estimate the impact of the national hepatitis B immunization program on the incidence of acute hepatitis B infection among adolescents in South Korea.
Methods
We estimated the counterfactual incidence rate of reported acute hepatitis B among adolescents from 2016 to 2020 compared to the assumption that the national hepatitis B immunization program for children had not been implemented since 1995. The impact of the national hepatitis B immunization program for adolescents was measured by estimating the absolute risk reduction and averted acute hepatitis B infections among adolescents from 2016 to 2020 attributed to the national immunization program.
Results
The relative risk reduction of acute hepatitis B among adolescents was estimated to be 83.5% after implementing the national hepatitis B immunization program. The incidence rate of reported acute hepatitis B infections among adolescents decreased from 0.39 to 0.06 per 100,000 person-years, and 43 acute hepatitis B infections, including 17 symptomatic cases, were averted annually from 2016 to 2020 by the national hepatitis B immunization program.
Conclusion
The national hepatitis B immunization program for children was effective in preventing acute hepatitis B infection among adolescents in South Korea.
Correspondences
- Comments on the article "Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates"
- Gaetano Perone
- Osong Public Health Res Perspect. 2023;14(2):146-146. Published online March 24, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0072L
- 830 View
- 32 Download
- Response to the comment of Perone by the corresponding author Kim
- Yongmoon Kim, Bryan Inho Kim, Sangwoo Tak
- Osong Public Health Res Perspect. 2023;14(2):147-147. Published online March 24, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0072R
- 735 View
- 31 Download





 First
First Prev
Prev


