A case-control study of acute hepatitis A in South Korea, 2019
Article information
Abstract
Objectives
We aimed to reconfirm the source of hepatitis A virus (HAV) infection through epidemiological and genotype investigations of individual cases in a 2019 outbreak in South Korea.
Methods
We investigated food intake histories, associations with hepatitis A, and genotypes of HAV in 31 patients with hepatitis aged 20 to 49 years registered in the integrated disease and health management system during December 1–7, 2019 (case group) and in 35 sex- and age-matched people without a history of HAV vaccination or infection among patients’ families and colleagues (control group).
Results
The consumption of salted clams was a significant factor (odds ratio, 4.33; 95% confidence interval, 1.32–14.18) in the risk factor analysis of food intake history. HAV genotypes were analyzed in 24 of 31 patients. Type IA and type IIIA were found in 23 and 1 cases, respectively.
Conclusion
Salted clams are considered to have been the source of HAV infection at 49 weeks of the HAV outbreak in 2019; this result was consistent with that of a previous epidemiological investigation conducted by the Korea Disease Control and Prevention Agency in September 2019. Therefore, monitoring of the production and distribution of salted clams needs to be continued.
Introduction
Hepatitis A is a waterborne and foodborne infectious disease caused by hepatitis A virus (HAV). HAV is an RNA virus classified into the genus Hepatovirus within the family Picornaviridae. HAV has only 1 serotype and 7 genotypes, of which types I, II, III, and IV are found in humans. Type I is distributed worldwide, with type IA mainly found in North America, Korea, China, Japan, and Taiwan and type IIIA observed in India, Sri Lanka, Nepal, Malaysia, and the United States [1,2].
HAV outbreaks occur due to the consumption of undercooked contaminated food or contaminated drinking water [3]. Raw foods such as frozen strawberries, scallops, pomegranate seeds, chives, and raw oysters, especially shellfish, are sources of HAV infection. As evidenced by the 290,000 infections caused by contaminated shellfish in Shanghai, China in 1988 [4] and 292 infections caused by the consumption of Philippine scallops in a sushi restaurant in Hawaii, USA in 2016, hepatitis A infections caused by the ingestion of shellfish have been occurring on an ongoing basis since the 1970s [5,6]. In addition, there was a recent case of occurrence owing to polluted groundwater in a park in South Korea (hereafter, Korea) in 2017 [7].
Hepatitis A was classified as a national notifiable infectious disease in Korea in 2010, and mandatory surveillance was initiated. After the occurrence of 5,521 cases in 2011, approximately 1,000 to 2,000 cases have occurred every year. In 2019, there was a large-scale outbreak of hepatitis A in 17,598 people, with an incidence rate of 33.95 per 100,000 people. Furthermore, 3,906 and 3,989 cases were reported in 2020 and 2021, respectively [8].
The 2019 hepatitis A epidemic epidemiological investigation conducted by the Korea Disease Control and Prevention Agency confirmed that salted clams were the source of infection in 21 of 26 cluster outbreaks as of August 2019. According to the results of 2 case-control studies, the intake rate of salted clams in the case group was 59 times and 115 times higher than that in the control group, respectively, suggesting that the main source of infection was salted clams [9,10]. In those investigations, the genotype analysis of HAV in patients and salted clams, which were suspected to be the source of infection during the 2019 hepatitis A outbreak epidemiological investigation, showed that the viruses were highly similar (i.e., type IA).
Based on the investigation results, on September 11, 2019, the Korea Disease Control and Prevention Agency confirmed that the main cause of the hepatitis A outbreak was contaminated salted clams. Therefore, it was recommended via the media to stop eating salted clams until safety was ensured. After that, the number of hepatitis A cases, which was 660 cases per week, steadily decreased. Therefore, when we conducted the investigation in the 49th week after the outbreak, only 63 cases (approximately 10%) were reported [8,9].
However, as individual infections continued to occur in the fourth quarter of 2019, it became necessary to determine whether the reason for the newly developed individual infections was salted clams or other infectious agents. Therefore, the source of infection due to food intake was evaluated in this case-control study of hepatitis A cases reported in the 49th week of 2019, approximately 2 months after it was recommended to stop eating clams (in the 37th week). This time point was chosen considering the incubation period of HAV.
This report was also intended to inform the public regarding the risk of HAV infection through the intake of salted seafood produced without heating.
Materials and Methods
Study Subjects
Hepatitis A epidemiological survey data registered at medical institutions using the Korea Disease Control and Prevention Agency’s integration system from December 1 to December 7, 2019 were analyzed.
Among 63 cases reported to the integrated disease and health management system during the abovementioned period, we identified 41 patients with hepatitis A among adults aged over 20 years who were diagnosed with hepatitis A based on clinical symptoms consistent with hepatitis A, HAV IgM detected in blood samples and specific genes detected in samples (such as blood, feces, or rectal swabs), while excluding cases of delayed reporting and cases for which epidemiological investigations were completed.
The control group included adults aged over 20 years who had established contact with patients during the same period. Among the patients’ families or colleagues, those who reported that they had no history of hepatitis A and had never been vaccinated against hepatitis A were selected with consideration of sex and age. However, there was a possibility that hepatitis A could be transmitted to them via contact with patients or exposure to the same infectious agents. Therefore, in this study, we monitored the occurrence of hepatitis A from the last exposure date to the maximum incubation period of 50 days to confirm that HAV infection did not take place.
In addition, people aged ≥50 years, who have HAV antibody positivity rates ≥90%, were excluded from the investigation on the basis of the results of a recent study on the prevalence of anti-HAV antibodies [10,11]. As a result, 31 and 35 people in the patient and control groups, respectively, were finally selected.
Study Methods
Epidemiological investigation (survey)
The responsible public health center and the Korea Disease Control and Prevention Agency reported patients’ clinical symptoms, isolation and management measures, food intake history, physical contact with infected persons, and contact tracing according to the management guidelines for waterborne and foodborne infectious diseases. In particular, the food intake history investigated the consumption of uncooked raw foods such as raw shellfish, various types of salted fish, and sashimi; frozen fruits such as strawberries, raspberries, and blackberries; and drinking water, including mineral water and groundwater. If there was an intake history of salted clams, the reason for intake was investigated [12].
Risk factor analysis
A case-control study was conducted by selecting hepatitis A patients aged 20 to 49 years who were reported from December 1 to 7, 2019 for the case group and family and work colleagues of patients for the control group. Our study considered HAV-contaminated food or drinking water intake as a risk factor.
HAV genotype analysis
The HAV genotypes of the case group were identified by the responsible Public Health and Environment Research Institute and were compared with the genotype distribution in the epidemiological investigation results obtained in September 2019.
Data analysis
IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for data analysis. The general characteristics of individuals in the patient and control groups are presented as frequencies and percentages, and the significance level was set to <0.05 using the chi-square test. In the case-control group study, odds ratios (ORs) and 95% confidence intervals (CIs) were obtained using the Excel 2013 program (Microsoft Corp., Redmond, WA, USA). In addition, this study was approved by the Institutional Review Board (IRB) of Seoul National University (IRB No: E2202/001-003).
Results
General Characteristics
The case group included 14 men (45.2%) and 17 women (54.8%), whereas the control group included 10 men (28.6%) and 25 women (71.4%). The average age of the individuals was 38.3 years, which was not significantly different from the average age of all hepatitis A patients reported through the Korea Disease Control and Prevention Agency’s integration system in 2019 [8]. Among the total participants, the percentage of those in their 40s was the highest (28 patients, 42.4%), followed by those in their 20s and 30s (19, 28.8%), respectively. No significant differences in the ratios were found with respect to sex and age in the patient and control groups (Table 1).
Hepatitis A in the case group occurred in 9 cities and provinces, most commonly in Gyeonggi Province (15 cases, 48.4%) and in Seoul metropolitan city (5 cases, 16.1%). In the control group, there were 18 people in Gyeonggi Province and 4 in Seoul metropolitan city. There was no significant difference in the distribution of residence areas between the patient and control groups (Table 1).
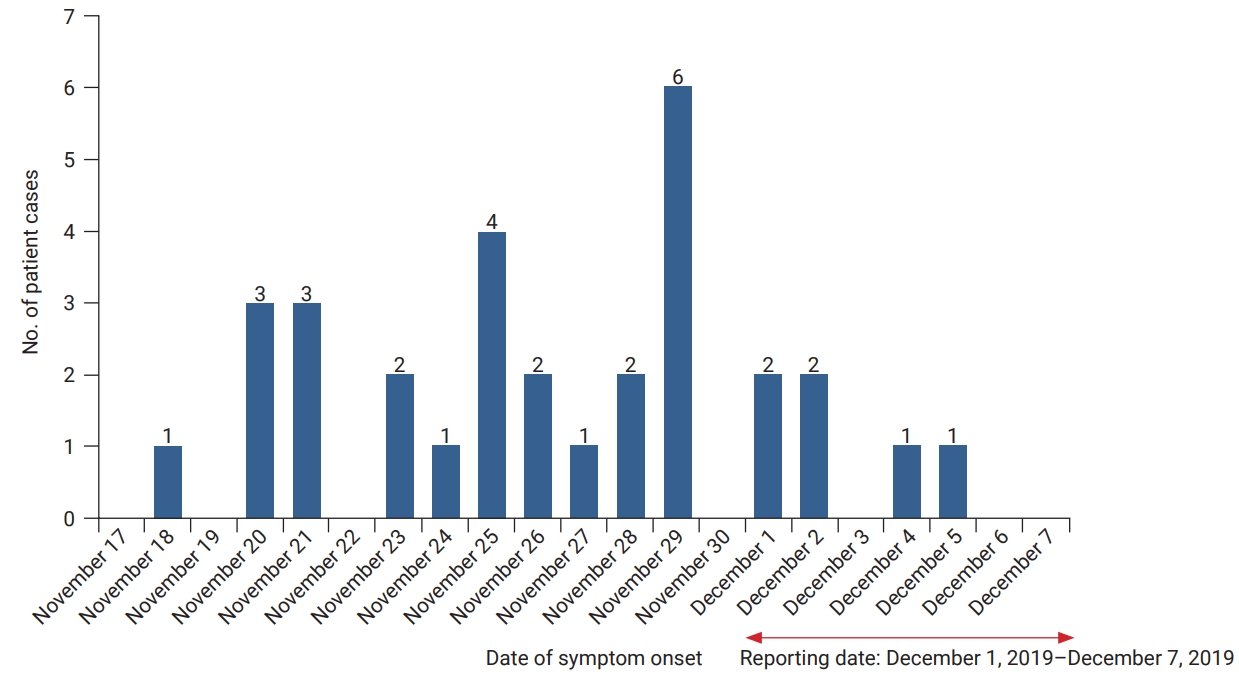
Epidemic Curve and Occurrence Characteristics
Thirty-one patients in the case group developed symptoms between November 18 and December 5, 2019. The average period from symptom onset to the report date was 7.8 days (minimum, 0 days; maximum, 15 days). The average period from symptom onset to the date of diagnosis was 6.0 days (minimum, 0 days; maximum, 15 days). The most frequent date of symptom onset was November 29, 2019 (6 patients, 19.4%), after which symptom onset continued to occur in 1 to 3 patients per day during the outbreak period (Figure 1).
The symptoms included fever of 38°C or higher (21 cases, 67.6%), nausea (19 cases, 61.3%), and a feeling of fatigue (18 cases, 58.1%), which were consistent with those reported before as the most common symptoms in the analysis of the 2017 epidemiological survey (i.e., fever, nausea, and severe fatigue/weakness). However, no cases of jaundice were reported in this study, unlike the previously reported jaundice incidence rate of approximately 40% [13].
Risk Factor Analysis
The intake of salted clams (OR, 4.33; 95% CI, 1.32–14.18) 15 to 50 days before the onset of symptoms was significant in the food intake analysis (Table 2).
In the case group, among patients with an intake history of salted clams, 13 (41.9%) purchased salted clams from a side-dish store near their residence, 8 (61.5%) purchased clams from a nearby market, and 5 (38.5%) consumed salted clams served as a side dish at a restaurant. Five patients (38.5%) reported being aware that salted clams were the probable source of HAV infection. Eight patients (61.5%) responded that they were unaware that salted clams were the probable source of HAV infection in 2019.
Five individuals with an intake history of salted clams in the control group purchased them from a nearby side-dish store and consumed them at home. Among them, 2 (40.0%) reported that they had heard about the recommendation to avoid eating salted clams through the news but ignored it because they judged that it would be safe to eat them from October to November, and 3 people (60.0%) responded that they were not aware of the recommendation.
Laboratory Test Results
The HAV genotype was identified in 24 of 31 patients. Type IA was detected in 23 patients, and type IIIA was detected in 1 patient.
Discussion
The number of patients with hepatitis A, which had reached 659 cases per week by the 34th week of the 2019 outbreak, decreased to 63 in the 49th week of 2019 after the recommendation to stop eating salted clams on September 11, 2019 (in the 37th week). In this study, we determined whether the source of infection in each case was still salted clams, even after recommending the public to stop consuming salted clams.
The incidence rate was high in Seoul and Gyeonggi Province, which accounted for 64.5% of the case group. This reflects the fact that patients with hepatitis A in Seoul and Gyeonggi Province accounted for 48.6% of all patients in 2019. The number of patients rapidly decreased after the recommendation to stop eating salted clams in the 39th week in Daejeon, Sejong, and Chungcheong Province, which had high crude incidence rates [8].
According to the results of the food intake history investigation to identify the source of infection, the intake rate of salted clams among the patients was 4.33 times (95% CI, 1.32–14.18) higher than that of the control group.; Therefore, after analyzing the data, this study revealed that salted clams were the source of infection. This finding is consistent with the study results reported by Seo et al. [14], who suggested that raw shellfish intake was a risk factor for hepatitis A, and the epidemiological investigation results published by the Korea Disease Control and Prevention Agency in September 2019 [15]. The genotypes of 87.5% of the 179 human samples and 80.4% of the 8 salted clam samples related to the cluster that occurred in 2019 were type IA. and the genotypes of HAV in the case group who ingested salted clams were all type IA, which was consistent with the results of a previous study [16].
Salted clams are bivalves that obtain nutrients by constantly filtering seawater. Therefore, when seawater is contaminated with viruses, the viruses may be concentrated inside the clam. In addition, because seawater along the coast, where sewage can flow in, can be continuously polluted, raw shellfish (including salted fish consumed raw) can be a source of HAV. It has been reported that HAV was detected in 8.9% of collected shellfish in Italy. HAV has also been detected in 3.8% of clams collected from fish farms or stores in Thailand. Therefore, this study considered salted clams as the source of infection in the 49th week of 2019 [17,18].
After the epidemiological investigation by the Korea Disease Control and Prevention Agency in September 2019, the Ministry of Food and Drug Safety inspected 136 salted clam products distributed in Korea in September 2019. The virus was detected, and the products were recovered and discarded in 44 cases, including 30 domestic and 14 Chinese salted clam products. In addition, domestic products were ordered to be inspected before sale to ensure that only products without viruses could be sold, and customs inspections were enforced for salted clams imported from China [19]. Regarding the distribution of salted clams, salted clams consumed in the patient and control groups were provided as side dishes at restaurants or were purchased from side-dish stores from the end of September to early November 2019 according to the epidemiological investigation results
Although mandatory surveillance and test orders were being implemented, the intake rate of salted clams in the case group was 4.33 times higher than that in the control group in this study. Moreover, a cluster infection of hepatitis A was reported in 6 people who consumed salted clams in April 2020. Therefore, cases of hepatitis A caused by salted clams continued to occur [20].
Compared with other products, there is a larger number of salted clams in products with the same serial number; therefore, clams that were omitted from sampling during the test may have been contaminated with HAV. Considering that HAV was detected in domestic products during product inspections in September 2019 and in raw clams collected at the Boryeong clam farm in Chungnam in December 2019, it is likely that contamination along Korea’s coast has occurred. Therefore, there is a possibility of HAV contamination of salted clams produced in Korea [21].
In addition, as salted clams are salted food products, the storage period is extended. Therefore, it is possible that consumers would continue to consume contaminated salted clam products without discarding the products they had individually purchased before the products were recalled. Moreover, in this study, more than 60% of people who ate salted clams were unaware that salted clams, an unheated food, could be contaminated. Therefore, it was assumed that individual cases of hepatitis A continued to occur because of the possibility of contamination of individual clams, as described above, and the continuous ingestion of contaminated salted clams without the awareness of relevant details owing to the lack of publicity.
In the food intake history investigation, sashimi intake, in addition to the consumption of salted clams, was higher in the case group than in the control group, although the difference was not statistically significant, and sashimi was identified as a probable source of infection. An investigation of the dietary history of patients with hepatitis A in Korea during the incubation period in 2017 found that these patients consumed a large proportion of raw vegetables/salads, followed by fresh fruit/fresh fruit juice, sashimi/sushi, steak tartare, raw oysters, and marinated raw crabs, with sashimi in the third place. The prevalence of norovirus infection, a waterborne and foodborne infectious disease caused by the ingestion of seafood caught in contaminated seawater, has also been reported.
HAV has been reported in approximately 1% of fish and shrimp harvested from the Persian Gulf, confirming that sashimi can also be a source of infection [13,22,23]. Therefore, in addition to salted clams, which have already been identified as infectious agents, existing probable sources of infection such as raw shellfish, including sashimi and oysters, and the intake of other raw foods should continue to be investigated and managed.
This study had limitations. First, the age group was selected by reviewing the general antibody positivity rate. However, considering that the antibody positivity rate of individuals in their 40s was 68% to 69%, anti-HAV immunoglobulin G tests were not performed in the control group, since there could have been cases wherein people were not infected with HAV even if they consumed contaminated salted clams. Therefore, the risk may appear lower than the actual level. Nevertheless, this study identified salted clam consumption as a significant risk factor (OR, 4.33; 95% CI, 1.32–14.18), clearly indicating that salted clams were the source of infection. Second, we requested cooperation from local governments to inspect restaurants and vendors. However, it was impossible to inspect the food because the salted clams had already been discarded, were not recorded in account books, or could not be collected because they were sold out a long time ago. Similarly, sashimi was not considered a significant source of infection even though sashimi was consumed by many subjects in addition to salted clams. However, like clams, fish also live in polluted waters, and sashimi is raw food. Therefore, the risk of infection from sashimi cannot be excluded. Nevertheless, no further investigation regarding foods related to sashimi intake was conducted. Finally, because HAV has a long incubation period and the infection can develop 1 to 2 weeks before the onset of symptoms, individuals’ memory may not have been accurate during the survey. In addition, salted clams were already known as a source of infection through the media in September. Therefore, there may have been a recall bias toward reporting intake of salted clams or salted seafood.
Conclusion
In the study by Ki et al. [24], the reasons for the 2019 hepatitis A outbreak were identified as a decrease in the level of adult herd immunity, a change in Korean food culture, a weak public health system, and a lack of effective coordination of public health policies. The occurrence of infections caused by shellfish intake was likely because of the age of patients with a low antibody retention rate and changes in eating habits [12].
Recently, in Korea, people in their 20s, 30s, and 40s have been shown to have low HAV antibody positivity rates because they have not acquired immunity after birth naturally or through vaccination. However, their intake of salted seafood, raw clams, and raw fish is higher in the context of the social activities of this group. Therefore, it is thought that HAV infection from salted clams reflected this increased risk of infection. In addition, it was assumed that the hepatitis A outbreak continued in December 2019 because of the possibility of contamination of coastal beaches, the inherent limitation of the inspection process that all of the clams in imported and domestic salted clam products cannot be tested, and the continued intake of salted clams owing to the lack of publicity after the recommendation to discontinue consumption.
The 2019 hepatitis A epidemic epidemiological investigation in Korea confirmed once again that salted shellfish, which is an unheated product, can be a source of HAV infection, as well as raw shellfish consumption. Therefore, the monitoring of imports, production, and sale of salted clams should be continued. In addition, in order to effectively investigate and manage HAV, which has a long incubation period, education including salt foods is needed for raw food types that can be a source of infection. In addition, it is necessary to actively promote information on the probable sources of infection, personal hygiene management, and safe food intake to prevent HAV infection in the future.
Notes
Ethics Approval
This study was approved by the Institutional Review Board of Seoul National University (IRB No: E2202/001-003) and performed in accordance with the principles of the Declaration of Helsinki.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding
This research was supported by the Expert Group on Health Promotion for the Seoul Metropolitan Government 2021, and the BK21 four project (Center for Human-Caring Nurse Leaders for the Future) funded by the Ministry of Education (MOE, Korea) and National Research Foundation of Korea (NRF).
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
Authors’ Contributions
Conceptualization: JHH, SHL; Data curation: JHH; Formal analysis: JHH; Investigation: JHH, SHL; Methodology: JHH, SHL; Project administration: all authors; Resources: JHH; Software: JHH; Supervision: JYY; Validation: JYY; Visualization: JHH, SHL; Writing-original draft: all authors; Writing-review & editing: all authors.
Additional Contributions
We thank all the local government infectious disease managers.