Noncommunicable Disease Risk Factors Among Adolescent Boys and Girls in Bangladesh: Evidence From a National Survey
Article information
Abstract
Objectives
To assess the prevalence of noncommunicable disease (NCD) risk factors and the factors associated with the coexistence of multiple risk factors (≥ 2 risk factors) among adolescent boys and girls in Bangladesh.
Methods
Data on selected NCD risk factors collected from face to face interviews of 4,907 boys and 4,865 girls in the national Nutrition Surveillance round 2018–2019, was used. Descriptive analysis and multivariable logistic regression were performed.
Results
The prevalence of insufficient fruit and vegetable intake, inadequate physical activity, tobacco use, and being overweight/obese was 90.72%, 29.03%, 4.57%, and 6.04%, respectively among boys; and 94.32%, 50.33%, 0.43%, and 8.03%, respectively among girls. Multiple risk factors were present among 34.87% of boys and 51.74% of girls. Younger age (p < 0.001), non-slum urban (p < 0.001) and slum residence (p < 0.001), higher paternal education (p = 0.001), and depression (p < 0.001) were associated with the coexistence of multiple risk factors in both boys and girls. Additionally, higher maternal education (p < 0.001) and richest wealth quintile (p = 0.023) were associated with the coexistence of multiple risk factors in girls.
Conclusion
The government should integrate specific services into the existing health and non-health programs which are aimed at reducing the burden of NCD risk factors.
Introduction
Globally, the incidence of noncommunicable diseases (NCDs) has been rising [1] and increase is perceived as a threat to the Sustainable Development Goals (SDGs) [2]. Major NCDs such as cardiovascular disease, respiratory diseases, cancer, and diabetes are rising globally, and disproportionately affecting developing countries [3]. Every year, 15 million NCDs are related to premature deaths, and 85% of those deaths occur in low, and middle-income countries [4].
An unhealthy diet, inadequate physical activity, tobacco use, being overweight and obesity are the major risk factors for NCDs [5]. Adolescence (10 to 19 years of life) is a crucial period of transition to adulthood [6], and during this period, adolescents are exposed to various unhealthy behaviors [7,8], which often continue into adulthood [9]. In a study of 65 low, and middle-income countries from 2003–2011, it has been reported that the prevalence of adolescents consuming an insufficient amount of fruit and vegetable, having an inadequate level of physical activity, using tobacco, consuming alcohol, and being obese was 74.3%, 71.4%, 12.1%, 15.7%, and 7.1%, respectively [10].
Furthermore, several studies have identified the coexistence of multiple risk factors for NCDs, such as low fruit and vegetable consumption, physical inactivity, smoking, alcohol use, sedentary behavior, being overweight or obesity during adolescence [11–14]. All of these risk factors are modifiable, and studies have demonstrated that practicing a healthy lifestyle such as consuming healthy food, engaging in regular physical activity, and avoiding tobacco could prevent 80% of cardiovascular disease and type 2 diabetes, and 40% of cancers [15]. So, in order to reduce the burden of NCDs, prevention strategies should begin during adolescence [16,17].
The government of Bangladesh is committed to improving adolescents’ health and developing the National Adolescent Health Strategy 2017–2030 [18] to ensure the highest level of health and wellbeing for adolescents [19]. The government of Bangladesh has achieved the health-related Millennium Development Goals and is now committed to attaining the Sustainable Development Goal by 2030. Adolescent health is aligned with the third goal of the SDGs i.e. good health, and wellbeing [20]. Additionally, the Global Strategy for Women’s, Children’s, and Adolescent health has stated “adolescents are the core of all to achieve the SDGs by 2030 [21].” Thus, the health and wellbeing of adolescents could accelerate the process of achieving the SDG commitment.
Various NCD risk factors persist among Bangladeshi adolescents but national prevalence and data on the coexistence of NCD risk factors among adolescents are mostly unknown [22–24]. The prevalence and distribution data of NCD risk factors among adolescents can help to identify the future burden of NCDs, as well as formulate evidence-based interventions to reduce the development of further NCDs [25]. Besides, the most crucial period of life to acquire healthy habits is in adolescence, and the maintenance of a healthy lifestyle during this period may prevent NCDs [26]. In addition, lifelong costs of healthcare can be minimized by developing a healthy lifestyle during adolescence [27]. Recognizing these aspects, a nationwide survey of 6 population groups, including adolescent boys and girls aged 10–19 years was conducted. In this study, the prevalence of NCD risk factors and factors associated with the coexistence of multiple risk factors was assessed among adolescent boys and girls in Bangladesh.
Materials and Methods
A nationwide cross-sectional survey was conducted from September 2018 to October 2019. Adolescent boys and girls aged 10–19 years were enrolled from 82 clusters (57 rural, 15 non-slums urban and 10 slums) in 8 administrative divisions of Bangladesh. A separate multistage cluster sampling technique was used for rural, non-slum urban, and slum areas to select the study participants. At first, 2 districts were randomly selected from each of the 8 administrative divisions, and then 2 sub-districts (upazilla) were randomly selected from each of the selected districts. In the third stage, one union was randomly selected from each selected sub-district. The villages with 250–400 households at the union were identified and further sub-division of a village to smaller segments occurred if it had 500 or more households. In the final stage, 2 segments or villages were randomly selected as the study clusters.
For the selection of the non-slum urban clusters, 2 wards were randomly selected from each of the 8 divisional headquarters, considering the proportion of the urban population in each division. From each ward, Mahallas were selected, and if any Mahalla contained more than 500 households, it was then segregated into smaller segments. Finally, 1–2 segments were randomly selected from each of the divisional headquarters as the study clusters. The “Census of Slum Areas and Floating Population 2014” was used for the selection of slum areas [28]. At the first stage, slums having ≥ 300 households were identified however, slums which had > 500 households were further divided into smaller segments. Later, 2 segments from the Dhaka and Chattogram, and 1 from the other 6 divisions (Rajshahi, Khulna, Sylhet, Barishal, Mymensingh, and Rangpur) were randomly selected as the study clusters.
All the households with eligible participants were listed and a total of 25,371 households with 10,529 boys and 10,211 girls (along with respondents in other age groups) were identified. From this group, nationally representative samples of 4,907 boys and 4,949 girls were interviewed. Data collection and all the anthropometric measurements of all the study participants were carried out at their residences. A locally made stadiometer was used to measure height, and weight was measured using a digital weighing scale (TANITA UM-070). Two measurements were taken for both height and weight. However, a third measurement was required if the difference between the first 2 consecutive measurements was > 0.5 cm and > 0.1 kg for height and weight, respectively.
There were 5 teams, each comprised of 1 project officer and 4–5 research assistants who collected data from all over Bangladesh. At the beginning of the study, all project officers and the research assistants received 5 days of training on interview technique and how to take anthropometric measurements (following WHO guidelines) [29]. A respective project officer was responsible for the supervision of his/her team as well as ensuring data quality. Data were directly entered onto tablet computers (Samsung Galaxy Tab A7) using a customized digital platform (Survey CTO) and were uploaded to the server at the end of the day. The data collection supervisors randomly visited the household from where data was already collected, and a statistician checked all the collected data regularly.
The outcome variables were insufficient fruits and vegetable intake, inadequate physical activity, tobacco use, and being overweight/obese. Fruits and vegetable intake was assessed with a questionnaire on how many days in a typical week an individual consumed fruits and vegetable and how many servings were consumed in 1 of those days. The WHO recommended show cards were used for making sure that the respondents understand the serving size [30]. Insufficient fruits and vegetable intake were defined as an intake of < 5 servings of fruits and vegetables in a typical day of the given week [30]. Physical activity was assessed using a questionnaire on how many days an individual was involved with various type of physical activities for at least for 10 minutes continuously in a typical day, how many days in a week, and the duration of those activities [30]. Inadequate physical activity was defined as moderate activities < 60-minutes/day and < 150 minutes/week for adolescents aged < 18 years and ≥ 18 years, respectively [31,32]. An adolescent was considered a tobacco user if she or he smoked or consumed smokeless tobacco daily in the last month before the interview day. Body mass index (BMI) was calculated using: BMI = Weight (kg) / Height (m)2 and classified adolescents as not overweight (< 85th percentile) or overweight/obese (≥ 85th percentile) using the age and gender specific WHO growth chart [33].
The household questionnaire for adolescents was in 4 sections including 1) Sociodemographic information, 2) food security 3) water, sanitation, and hygiene practices, 4) behavioral risk factors of NCDs, and mental health. Hence, sociodemographic information, food security, water, sanitation, and hygiene practices were answered by household heads. The wealth index was assessed through some specific assets such as availability of amenities (electricity, solar electricity, radio, television, telephone, mobile, refrigerator, table/chair, watch/wall clock, almirah/wardrobe, electric fan, bicycle, motorcycle/motor scooter, car/truck, boat, or water pump), the household cooking fuel used (electricity, liquefied petroleum gas, piped natural gas, kerosene, coal, wood, straw/grass/leaves, animal dung, or bio-gas), the main source of drinking water, type of toilet used, household floor material, walls and roof. All of these household characteristics and assets were analyzed using principal component analysis. A composite wealth index was assessed using DHS (demographic and health survey) method consisting of area-specific indexes combined into a national model [34]. The wealth index was divided into 5 quintiles. Mental health status was assessed using a 9-item Patient Health Questionnaire (PHQ-9). The participants were asked how often they experienced the 9-item symptoms over the last 2 weeks. There were 4 options for each item including not at all (score = 0), sometimes (score = 1), most of the time (score = 2), all the time (score = 3). The scores were computed as all the scores of the 9-item symptoms for an individual and then scores were dichotomized into “no depression” (score 0–4) and “depression” (score 5–27) [35].
Data was analyzed using Stata Version 13.0 (Stata Corp, College Station, TX, USA). Adolescent boys’ and girls’ data for NCD risk factors were separately analyzed. There were 84 adolescent girls excluded from the analysis since they were pregnant during the survey. Descriptive analyses were performed to assess sociodemographic characteristics of study participants. The weighted prevalence of selected NCD risk factors was reported among adolescent boys and girls. Later, the NCD risk factors were clustered and the coexistence of multiple risk factors was measured in a single participant. Simple logistic regression between the outcome variable with each independent variable was carried out, and variables with a p < 0.2 were considered for multivariable logistic regression. Multivariable logistic regression was performed to identify the factors associated with the coexistence of multiple risk factors. The associations between the outcome and the explanatory variables were considered significant if the p value was < 0.05.
Ethical clearance from the Institutional Review Board of the BRAC James P Grant School of Public Health, BRAC University, Dhaka, Bangladesh was obtained for this study (IRB: 2018-020-IR). Informed written consent was given after explaining the study objectives and procedures from those aged ≥ 18 years, and consent of their parents for those aged < 18 years.
Results
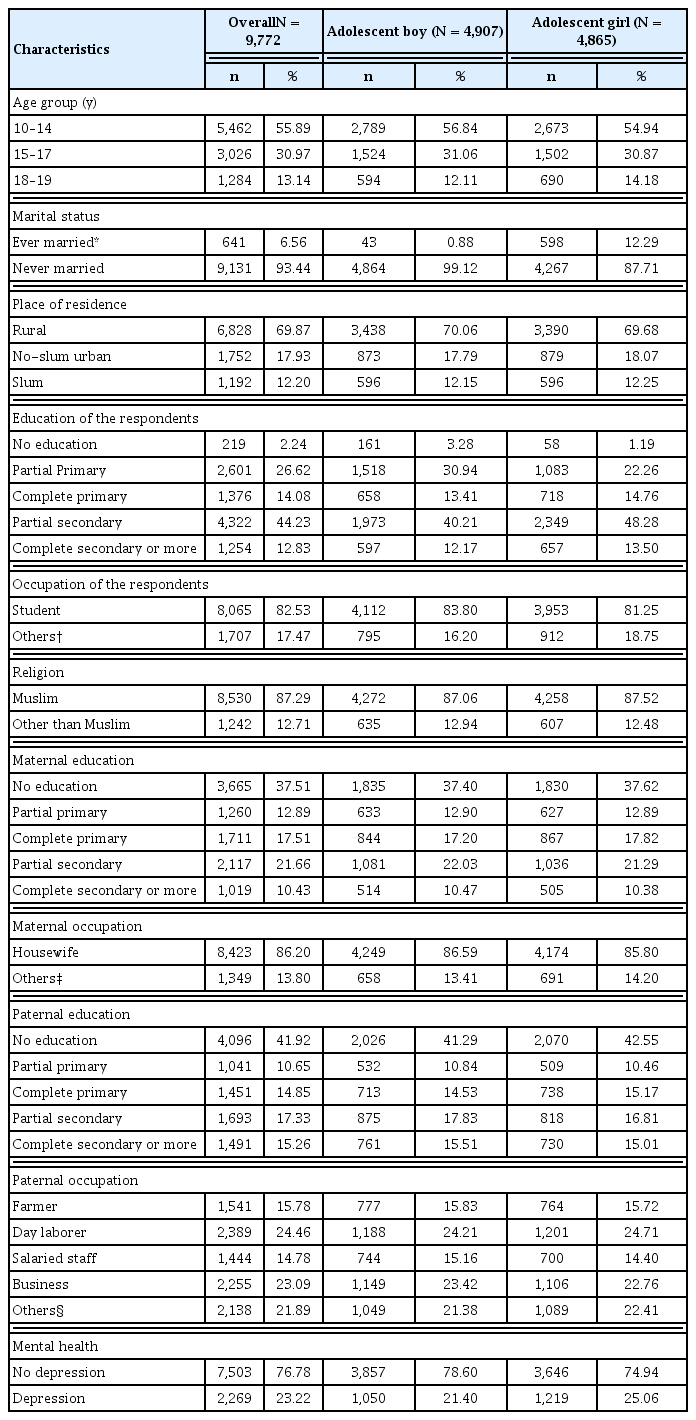
A total of 9,772 adolescent boys and girls participated in this study, and of them, 4,907 were boys, and 4,865 were girls (Table 1). More than 1/2 of the participants were aged between 10 and 14 years. While 12% of the adolescent girls were married, the percentage among boys was only 1%. Almost 2/3 of the adolescents were from rural areas. A higher proportion of girls completed secondary and higher secondary education compared with the boys. However, the fathers of both girls and boys were more educated than their mothers. About 1/4 of adolescents suffered from depression, and the proportion was higher among girls than boys.
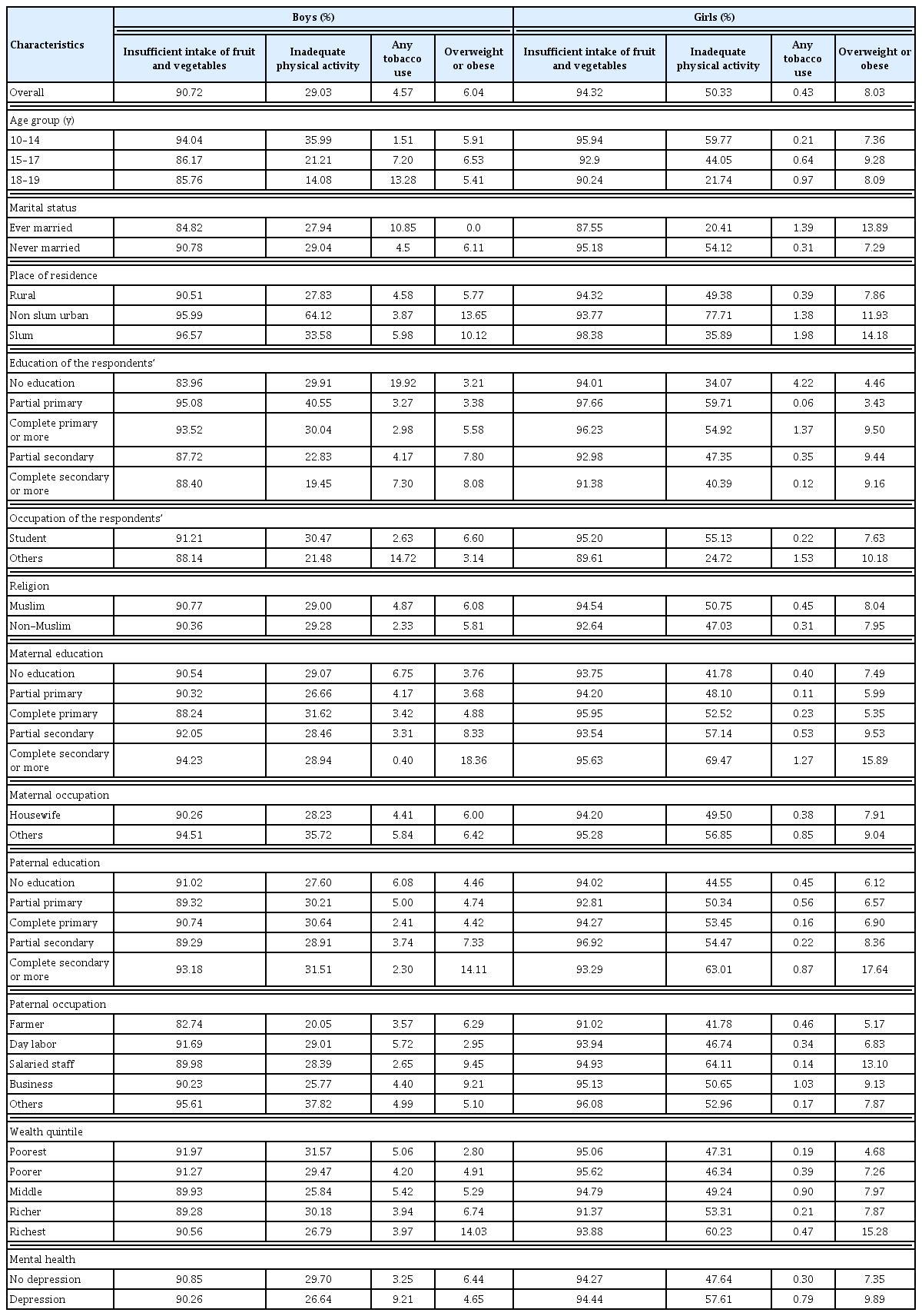
The weighted prevalence of NCD risk factors by sociodemo-graphic characteristics showed that among the adolescent boys, the prevalence of insufficient fruits and vegetable intake, inadequate physical activity, any tobacco use, and being overweight/obese were 90.72%, 29.03%, 4.57%, and 6.04%, respectively (Table 2). In contrast, among girls, the prevalence of insufficient fruits and vegetable intake, inadequate physical activity, any tobacco use, and being overweight/obese were 94.32%, 50.33%, 0.43%, and 8.03%, respectively. In older age groups, the prevalence of insufficient fruit and vegetable intake decreased in both sexes, and the prevalence was higher among adolescents living in slums. The prevalence of inadequate physical activity was lower in older adolescents. Non-slum urban adolescents (boys: 64.12%, girls: 77.71%) showed a higher prevalence of inadequate physical activity compared with their rural (boys: 27.83% girls: 49.38%), and slum (boys: 33.58%, girls: 35.89%) counterparts. In the case of girls, the prevalence of inadequate physical activity increased with both of their maternal and paternal higher education. However, this trend was not observed for boys. The prevalence of any form of tobacco use was higher among older adolescents living in slum areas and among those who were depressed, compared with younger adolescents living in areas other than slums and who were not depressed. All the NCD risk factors (insufficient fruits and vegetable intake, inadequate physical activity, use of tobacco, and being overweight or obese) were more common among depressed girls than those who were not depressed.
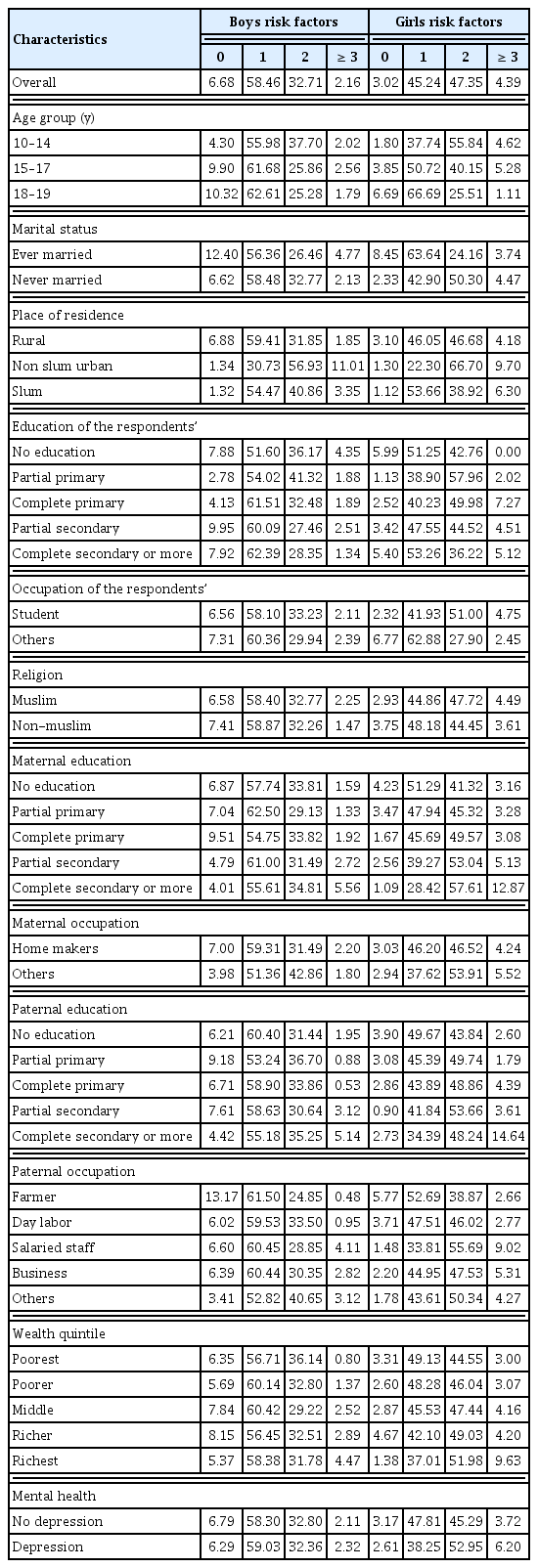
The prevalence of 1 or multiple risk factors of NCDs among study participants was assessed (Table 3). It was observed that only 6.68% of boys and 3.02% of girls had no NCD risk factors. The overall prevalence of 1 risk factor, 2 risk factors, and 3 or more risk factors among adolescent boys was 58.46%, 32.71%, and 2.16%, respectively, while among girls, the prevalence was 45.24%, 47.35%, and 4.39%, respectively. The prevalence of 1 risk factor increased with age, while the prevalence of 2 risk factors decreased. The coexistence of 2, and 3 or more risk factors among non-slum urban adolescents was higher than adolescents living in rural and slum areas. In the case of girls, though the prevalence of 1 risk factor was lower among adolescents of highly educated parents, the prevalence of 2 risk factors was higher among adolescents having highly educated mothers. The prevalence of 3 or more risk factors were higher among adolescents who belonged to the highest wealth quintile and those who were depressed compared with the adolescents who belonged to other wealth statuses and those who were not depressed.
The unadjusted and adjusted odds ratio with a 95% CI for the factors associated with the coexistence of 2 or more risk factors was assessed (Table 4). There was a significant association between age and the coexistence of multiple risk factors among adolescents. Both boys and girls living in the slum (boys: AOR: 1.68; 95% CI: 1.39–2.02 and girls: AOR: 1.37; 95% CI:1.13–1.65) and non-slum urban areas (boys: AOR: 2.91; 95% CI: 2.44–3.48 and girls: AOR: 2.16; 95% CI:1.79–2.61) had higher odds of having multiple risk factors than those living in rural areas. Among girls, the odds of having multiple risk factors was higher among those whose maternal education was partial primary (AOR: 1.22; 95% CI:1.00–1.48), complete primary (AOR: 1.27; 95% CI: 1.06–1.52), partial secondary (AOR: 1.58; 95% CI:1.32–1.89), and completed secondary or higher (AOR: 1.72; 95% CI:1.29–2.29). Paternal education was associated with having multiple risk factors for both adolescent boys and girls. In the case of boys, this association was statistically significant for those whose father received a partial primary education (p = 0.005) or a complete secondary education (p = 0.033). In the case of girls, this association was not significant only for those whose father completed primary education. However, there was no significant association between the respondents’ education and coexistence of multiple risk factors. It was also observed that the boys and girls with depression were more likely to have multiple risk factors than those who did not have depression (boys: AOR: 1.30; 95% CI:1.13–1.51, girls: AOR: 1.40; 95% CI:1.22–1.62).
Discussion
This study is the first of its kind to report the prevalence and clustering of NCD risk factors along with factors associated with the coexistence of multiple risk factors among adolescent boys and girls in Bangladesh. The study showed a high prevalence of NCD risk factors among adolescents in Bangladesh, and all identified risk factors (except for tobacco use) were more common among adolescent girls than boys. Age, place of residence, paternal education, and depression were associated with having multiple risk factors among both boys and girls. Additionally, maternal education and wealth status were significantly associated with the coexistence of multiple risk factors among girls.
This study observed that 9 out of 10 adolescents did not consume the recommended amount of fruit and vegetables, which is similar to the findings of a recently reported survey in Bangladesh [36]. The prevalence of insufficient fruit and vegetable intake identified among adolescents living in the slums was high compared with rural or non-slum urban adolescents, which is supported by the findings reported by Rawal et al [37]. Low socioeconomic conditions of the people who live in slums may prevent them from buying fruit and vegetables which may be too costly forcing them to consume readily available, inexpensive, unhealthy food [37]. It was observed in this current study that the number of adolescent girls with reportedly inadequate physical activity was almost twice the number observed among boys. This finding is consistent with the previous findings of studies conducted in Bangladesh and Iran [22,38]. Sociocultural factors may play an important role in this gender difference. In context of Southern Asia, boys have more access to sports and other outdoor physical activities compared with girls, and girls are more likely to be involved in household chores [38]. Moreover, parents are concerned about girls’ safety and prefer them to stay at home instead of performing outdoor physical activities [22]. In this situation, girls could increase physical activity by using school and college playgrounds which are accessible, and participate in indoor sports and physical exercise [39]. In addition,, community and parental support can play a crucial role in improving girls’ physical activity.
In this current study, 6.0% of boys and 8.0% of girls were either overweight or obese which was lower than the prevalence in Indian adolescent boys (6.6%) and girls (14.1%) [40]. However, the nutritional status of adolescent boys in Bangladesh has not previously reported. In a previously published report, Mridha et al [41] reported that 5% to 23% of Bangladeshi adolescent girls were either overweight or obese. The result of these 2 studies may vary due to the sampling strategy, selection area, and the methodology used for the survey. The finding in this current study showed a higher prevalence of being overweight/obese among girls compared with boys, which is consistent with the study by Laxmaiah et al [42]. Girls were less likely to be involved in physical activity, and spent their leisure time watching television, and relaxing [43]. It has been reported that overweight/obese adolescents are more likely to develop atherosclerosis, coronary heart disease during adulthood [44]. Government initiative is required to reduce this health problem. Adolescents should be educated about physical activity and be inspired to become involved in various outdoor sports and activities (brisk walking), particularly girls.
Tobacco use, was more prominent among boys than girls, and these findings were similar to previously reported studies [45,46]. Gender disparity in tobacco use is probably due to cultural constraints. In Bangladesh, though females use smokeless tobacco, smoking is regarded as unacceptable in society [37]. This study identified that only 6.68% of boys and 3.02% of girls were free from NCD risk factors amongst insufficient fruit and vegetable intake, inadequate physical activity, tobacco use, being overweight/obese. Sanchez et al [47] reported that only 1.2% of girls and 2.8% of boys did not have risk factors (physical activity, television viewing time, dietary recommendations for fat and fruit, and vegetable intake). In another study among Pakistani adolescents, investigators reported that only 3.1% of participants had no risk factors amongst physical inactivity, betel nut use, smoking, smokeless tobacco use, and unhealthy diet [48]. Though the generalization of these findings was difficult because different NCD risk factors were assessed in different studies, it is evident that NCD risk factors are widely present among adolescents.
The coexistence of multiple risk factors (i.e., insufficient intake of fruit and vegetables, inadequate physical activity, tobacco use, being overweight, and obesity) were less likely to be observed among older adolescents in this current study. However, other studies reported that specific risk factors were more prevalent among older adolescents [49,50]. A possible explanation may be that the variables associated with specific risk factors may not be the same as the variables associated with the coexistence of multiple risk factors [14]. Further studies are needed to understand how the coexistence of multiple risk factors among adolescents varies over time. Adolescents who lived in the slums and non-slum urban areas had higher odds of having multiple risk factors than those who lived in rural areas. A nationally representative study also reported that urban residents of Bangladesh were more likely to have multiple risk factors (inadequate fruit and vegetable intake, low physical activity, tobacco use, being overweight, hypertension, diabetes) than rural residents [51]. Bangladesh is undergoing rapid and unplanned urbanization [52]. As a result, multiple behavioral risk factors such as inadequate fruit and vegetable intake, insufficient physical activity, smoking, being overweight, and obesity are increasing among urban people [37]. The findings from this current study suggest that public health interventions should also target urban adolescents to prevent and control NCDs.
This current study revealed that among girls, the coexistence of multiple risk factors was associated with both parents having a higher education while in the case of boys, this was associated with paternal higher education only. In a study among Asians (including Bangladeshis), Ahmed et al [53] reported that raising the educational status raises the wealth status. As a result, there is an increase in sedentary lifestyle, tobacco use, and consumption of a high-fat diet [53]. It has also been reported that children and adolescents are closer to their parents, and parental health behaviors are significantly associated with adolescent’s health behaviors [47,54]. Therefore, health promotion interventions focused on parents are also required so that the parents can help their children adopt healthy practices. It was also observed that depression was positively associated with the coexistence of multiple risk factors among adolescents. Adolescence is a crucial period of life, and during this time, adolescents face many critical situations and obstacles pertinent to individual, familial, and social circumstances. Some adolescents are unable to cope with this and suffer from depression [55]. Adolescents with depressive symptoms may adopt an unhealthy lifestyle such as eating unhealthy diets, performing less physical activity, and leading a sedentary lifestyle [56,57]. Therefore, during this time, adolescents need the utmost parental care, support, and empathy to cope with adverse situations, and lead a healthy life [58]. Moreover, adolescents suffering from depression should be identified and treated.
This is the first study where nationally representative data for both adolescent boys and girls have been used. Moreover, NCD risk factors were analyzed separately for boys and girls, which provides more insight into the vulnerability of adolescents. However, this study had some limitations too. Firstly, it was a cross-sectional study that did not substantiate the causal claims on the coexistence of multiple risk factors due to a lack of temporality. Secondly, the behavioral risk factors were assessed based on self-reported information. Thirdly, “occasional” use of tobacco products was not assessed among adolescents. Fourthly, 2 WHO suggested risk factors i.e. blood pressure and blood glucose among the adolescents were not measured.
The findings of this study have important implications for public health policymakers. The NCD risk factors that are reported in this study are modifiable. The government should develop school-based strategies to educate adolescents on healthy lifestyles, including consumption of adequate fruit and vegetables, increasing physical activity, avoiding tobacco use, and not having an unhealthy diet. Besides, stakeholders and others should take the necessary steps to raise awareness about the consequence of these NCD risk factors not only among adolescents, but also their parents.
Conclusion
Adolescents in Bangladesh have a high prevalence of NCD risk factors, and all of the NCD risk factors studied including insufficient fruit and vegetable intake, inadequate physical activity, and being overweight/obese were more prevalent among girls than boys. More than a 1/3 of boys and more than 1/2 of the girls had more than 1 risk factor. The most-reported risk factors among adolescents were insufficient fruit and vegetable intake, followed by inadequate physical activity. It was observed that age, place of residence, paternal education, and depression were significantly associated with the coexistence of multiple risk factors in both boys and girls. Moreover, in the case of girls, maternal education, and wealth status were associated with the coexistence of multiple risk factors. It is crucial to identify susceptible adolescents for the prevention and control of NCDs, and special attention should be given to girls, younger adolescents, and those who live in slums, and non-slum urban areas.
Acknowledgments
The authors are grateful to all the study participants, data collectors, data collector supervisors, and administrators of the National Nutrition Surveillance round 2018–19.
Notes
Conflicts of Interest
The authors have no conflicts of interest to declare.