Dual Task Training Effects on Upper Extremity Functions and Performance of Daily Activities of Chronic Stroke Patients
Article information
Abstract
Objectives
The purpose of this research was to study the influences of dual task training on upper extremity function and performance of daily activities of chronic stroke patients.
Methods
Dual task training was performed on 21 patients who had suffered a chronic stroke with hemiplegia. The dual task training was performed for 30 minutes per session, for 5 days a week, for 3 weeks. There were 5 evaluations carried out over 3 weeks before and after the intervention. Changes in upper extremity function were measured by using the Box and block test. Changes in the performance of daily activities were measured using the Korea-Modified Barthel Index.
Results
The mean upper limb function score of the chronic stroke patients increased significantly from 21.88 ± 19.99 before the intervention, to 26.22 ± 15.65 after the intervention (p < 0.05), and the mean daily activities score increased significantly from 65.82 ± 12.04, to 67.29 ± 12.90 (p < 0.05).
Conclusion
Dual task training effectively improved upper extremity function, and the performance of daily activities in chronic stroke patients.
Introduction
A stroke is a serious condition that occurs when the blood supply to the brain is either blocked causing sudden ischemia, or when there has been a hemorrhage of blood vessels, causing partial loss of brain function that leads to functional disability [1]. Some of the common symptoms of a stroke include loss of function of the upper limbs due to weakened muscles and sensory changes, difficulty in trunk control, unstable balance and gait, and inability to perform basic daily activities [2]. Of these symptoms, the inability to perform daily activities deteriorates the patients’ level of independence in their daily routines and increases their dependence on others, which may lead to loss of self-esteem and depression, resulting in a comprehensive decline in quality of life.
Basic daily activities are highly likely to include activities that require the simultaneous performance of 2 or more actions or functional tasks [3]. However, if a person with impaired cognitive or physical function, such as a stroke patient, performs 2 or more tasks at once, he or she may experience dual-task interference, where it is difficult for the patient to concentrate. As a result, their ability to perform daily activities that require at least 2 tasks will generally deteriorate [4].
Dual-task training is a practical interventional method for actual daily activities of a patient beyond the clinic, that helps to reduce dual-task interference. Generally, dual-task training refers to performing 1 task whilst being engaged in another, or performing 2 or more tasks simultaneously [5].
Many studies of stroke patients use dual-task training programs combining activities that require walking, balancing, trunk control, and upper limb function [5–7] to demonstrate efficacy, however, there are limited analyses of improved performance in daily activities. In fact, this may be the most important area for patient upper limb function and rehabilitation. Therefore, this study applied dual task training to chronic stroke patients to examine the effects of the training on their upper limb functions and daily activities.
Materials and Methods
1. Participants
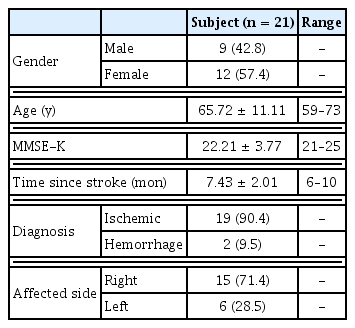
Prior to participation, all patients were instructed of the purpose of this study before requesting informed consent. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Of the stroke patients who had been admitted into Hospital A in South Korea under occupational therapy care, 21 patients understood and provided their consent to participate in the study. The selection criteria included patients with diagnosis of hemiplegia induced by a stroke which has occurred at least 6 months from the initial onset, and had a score of at least 20 on the Mini Mental State Examination-Korean [indicating the capability to follow the instructions of the researcher, capability of independent walking for 5 minutes at a comfortable pace, and the absence of neurological or orthopedic diseases other than stroke (Table 1)]. Patients who were undergoing medicinal treatment to reduce spasticity were not included in the study.
2. Procedure and measurement
This study used a single group pre-test post-test design. To select the patients, their general information was checked alongside medical records. The effects of dual-task training in patients in the pre-study were examined using the BBT (box and block test, as an assessment tool for the patients’ upper limb functions) and the K-MBI (Korea-modified Barthel index, to measure their capabilities of performing daily activities) assessment tools. Dual-task training was performed for 5 sessions per week for 4 weeks, 30 minutes per session was used as the intervention program for this study. After completing the 4-week intervention program, the BBT and K-MBI were conducted as a post-study in the same manner as the pre-study. As a standardized tool to assess the agility of the upper limbs, the BBT assessed the number of wooden blocks the patients could move within a minute. The test-retest reliability of this tool was 0.93 for the left hand and 0.97 for the right hand, and the inter-tester reliability was 0.99 for the left hand and 1.00 for the right hand [8]. The Barthel index was revised and supplemented by Granger et al [9] in 1979, leading to the assessment tool known as K-MBI which is sensitive to changes in the capabilities of performing daily activities. It had a test-retest inter-test reliability of 0.89 and 0.95, respectively [9]. The K-MBI test consists of 10 questions, and the score is out of 100 points. A score of between 0–24 indicates total dependence, 25–49 maximal dependence, 50–74 partial dependence, 75–90 slight dependence, 91–99 minimal dependence, and 100 total independence.
The applied individual program for upper limbs consisted of 3 tasks proposed by Schaefer et al [10]: moving beans with a spoon, classifying wooden blocks by color, and opening bottle caps. All activities were performed by the patient standing on a sissel sitfit (CH 8904 Aesch, Switzerland) air cushion with a diameter of 33 cm exposed to an unstable bearing surface. To assist the patients in their understanding, the therapists provided demonstrations and explanations prior to the patients’ performance of the study activities. When the patients expressed their full understanding in the training process, the dual-task training was started. The individual training tasks were randomly selected for implementation, and a break time was given to relieve patients’ fatigue during training.
3. Statistical analysis
PASW 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis of this study. Technical statistics were used to analyze the general properties of the patients, and paired samples t test was conducted after confirming a normal distribution through a test of normality (Shapiro-Wilk) on the patients to measure the changes in their capacity to perform daily activities and upper limb functions before and after the intervention.
Results
Table 2 shows the patients’ upper limb function and capability of performing daily activities before and after the intervention in this study. Firstly, patients’ upper limb function statistically significantly improved (p < 0.05), with the average BBT increasing from 21.88 points before the dual-task training intervention to 26.22 points after the intervention. In terms of the capability of performing daily activities, the mean K-MBI increased from 64.82 points before the intervention, to 67.29 points after the intervention (p < 0.05). These results showed statistically significant changes not only in the upper limb functions but also in the capability of performing daily activities (p < 0.05).
Discussion
An important thing to note is that improvement due to interventional training for stroke patients shown in the therapy room are retained in their daily lives. Filiatrault et al [11] reported that the sustained therapeutic effects from clinic to home depended on the similarities of the 2 tasks performed, or similarity of the 2 different environments. In other words, the more the training environment and practical environment were similar, the better the learning or therapeutic effects were transferred. Dual-task training differs from the simple task training conducted in clinical studies of stroke patients, to more closely resemble the patients’ daily routines, which require the simultaneous performance of various tasks. In this respect, this study applied dual task training, which resembles actual daily tasks to chronic stroke patients, to examine the therapeutic effects on upper limb function and performance of daily activities. As a result, statistically significant effects of the dual-task training were observed in chronic stroke patients’ upper limb function and capability of performing daily tasks (p < 0.05). These results signify the positive effects of dual-task training on upper limb function and performance of daily activities of chronic stroke patients, in addition to the positive effects on the walking ability, trunk control, and balancing of stroke patients that have been reported in many preceding studies [5–7]. Generally, the purpose of physical therapy following a stroke, is to maximally recover from the functional loss, reduce dependence upon others in daily activities, and assist in resuming their social roles. Of these outcomes, enhancing the ability to perform daily activities is arguably the most important objective to achieve the goal of helping stroke patients recover their normal lives [11–13].
In addition, a previous study noted that if there was no meaningful functional transition for the daily life activities, even if there was a quality improvement in the upper limb function, the upper limb function could not be regarded as having been improved, and an improvement of upper limb function in stroke patients would be closely related to their improvement in daily life performance [14]. It was confirmed that dual-task training could have a positive effect not only on the upper limb function of the patients, but also on the daily life performance ability, which is the end goal of rehabilitation, and this study has a significant meaning in this regard. The limitations of this study include the difficulty in applying its findings to all stroke patients, as it was conducted on a small number of patients, without a control group in the study design.
Notes
Conflicts of Interest
The author has no conflicts of interest to declare.