Contact Transmission of COVID-19 in South Korea: Novel Investigation Techniques for Tracing Contacts
Article information
Abstract
In the epidemiological investigation of an infectious disease, investigating, classifying, tracking, and managing contacts by identifying the patient’s route are important for preventing further transmission of the disease. However, omissions and errors in previous activities can occur when the investigation is performed through only a proxy interview with the patient. To overcome these limitations, methods that can objectively verify the patient’s claims (medical facility records, Global Positioning System, card transactions, and closed-circuit television) were used for the recent ongoing coronavirus disease 2019 contact investigations in South Korea.
Introduction
An epidemiological investigation aims to quickly determine the prevalence of an infectious disease whilst simultaneously revealing the cause, and source of the disease, and explore the transmission process to ultimately prevent the spread of the infectious disease [1]. As individuals become the source of the infectious disease, and if person-to-person transmission is suspected, it is important to immediately identify, and manage people that are in close contact with suspected patients [2,3]. In particular, if there are several unknown epidemiological and clinical characteristics, and an effective medical intervention is lacking (as in the case of new infectious diseases such as COVID-19), contact management becomes 1 of the core strategies to minimize additional transmission. For these strategies to be successful, it is necessary to evaluate between-person exposure risk in all locations where there have been confirmed cases (after the onset of symptoms), and to classify contact persons based on this risk. Furthermore, it is also important to eliminate the possibility of exposure to infection in the places visited by the confirmed patient, by performing the appropriate disinfection of areas that can harbor environmental contamination [2]. However, traditional investigative methods, depending on the patient or proxy interview, has the limitation of omissions and errors of previous activities.
The COVID-19 outbreak in China occurred on December 8th, 2019, and the first case in Korea was reported on January 20th, 2020. As of February 14th, the total number of confirmed cases of COVID-19 in Korea was 28. In the current epidemiological investigation contact investigation techniques that were used on a limited basis for the Middle East Respiratory Syndrome (MERS) outbreak in 2015, are being used in all confirmed cases of COVID-19.
This report will provide a general overview of the contact investigation from the COVID-19 National Emergency Response Center, Epidemiology and Case management team and describe the various methods used to evaluate exposure risk.
Results
COVID-19 contact investigation and management comprised of the following: 1) determination of the location of the contact (patient route), 2) exposure risk evaluation, 3) contact classification, and 4) contact management. The location of the contact was determined through the process of preliminary identification, by interviewing patients, and their acquaintances, and by objective verification of the investigated information. Exposure risk evaluation was performed depending on the route of disease transmission, patient characteristics, and environmental characteristics. Based on the results of the evaluation, the contacts were classified into close and casual contacts depending on the exposure [4]. The method of managing the classified contacts was largely distinguished between movement restriction and symptom monitoring. Movement restriction is a legal public health order, and quarantine (isolation), home isolation, or controlled travel is enacted. Symptom monitoring was performed as either active or passive monitoring, depending on the exposure risk (Figure 1).
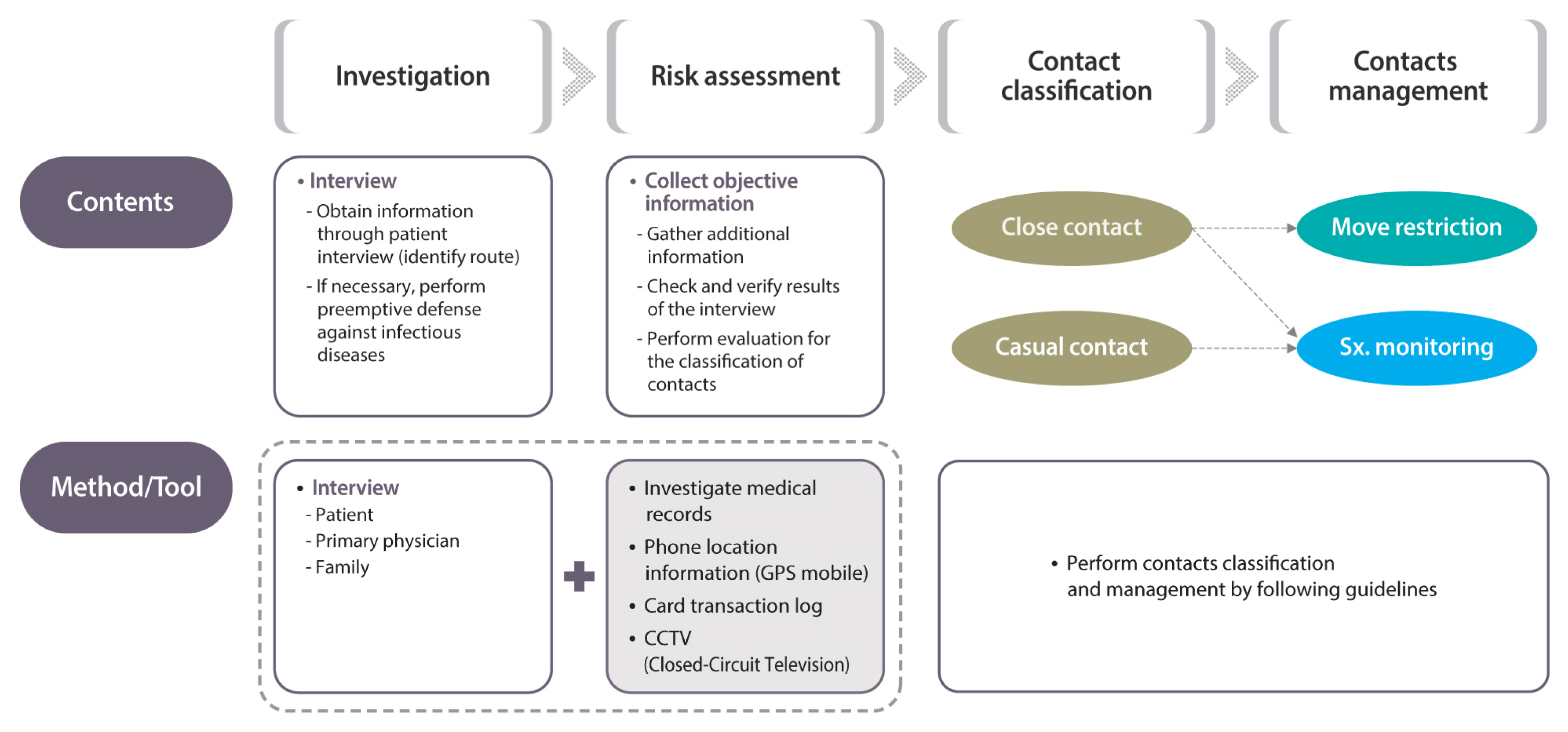
Stepwise approach in monitoring contacts when a patient with COVID-19 is detected.
GPS = global positioning system.
The methods used to overcome recall and confirmation biases that can occur while determining the location of the contact include checking medical facilities records, phone-based global positioning system (GPS), card transaction records, and closed-circuit television (CCTV; Table 1).

Information collection methods for the monitoring and management of patients with COVID-19 and their contacts.
1. History of using medical facilities and visiting pharmacies
History of using medical facilities, and visiting pharmacies was used to estimate the window of time of infection, through an accurate evaluation of the clinical symptoms of the infectious disease, and initial onset of the symptoms. If a medical facility was included in the patient’s route, quarantine of the medical facility was conducted.
2. GPS
Consistency in the recall of the route of the patients identified through interview was evaluated. Additionally, identification of the routes that the patient could not remember was also possible. However, another person’s information can be misunderstood as the patient’s information if the phone is not owned by or carried by the patient. GPS uses cellular phone networks, therefore there are limitations in identifying the exact locations of a patient’s route.
3. Credit card transaction log
Credit card transaction logs were used to assess the consistency in the route of the patient identified through interview, and the scope of contacts was assessed by specifying the locations visited. However, if the patient did not use a credit card under their name or if another person used the patient’s card, the information may be misinterpreted. Thus, rechecking the contents of the credit card log was necessary, and instances of not being able to use the information at the appropriate time may occur.
4. CCTV
By checking the video footage of the location of a patient’s path, CCTV provided help to identify the details of each situation. For example, CCTV was used to evaluate the level of exposure risk by identifying whether the patient wore masks, or had respiratory symptoms such as a cough. The limitations of using CCTV were the lengthy time required to check the CCTV, and the accuracy of patient identification if the CCTV was not inside the facility or the patient was in a blind spot of the camera.
Discussion
Based on the experience of the MERS outbreak in 2015, laws were revised to supplement the areas that were lacking at the time. Korea Centers for Disease Control and Prevention were able to use relevant information in epidemiological investigations to contain and prevent infection, thus enabling the establishment of a more comprehensive management of infectious diseases. Furthermore, making accurate information available to the general public helps to minimize fear and confusion with respect to the risk of transmissibility of the disease. The use of methods that have objectively verified the patient’s route claims (medical facility records, GPS, card transactions, and CCTV) for COVID-19 contact investigations in South Korea has provided accurate information on the location, and time of exposure, and details of the situation, thus reducing omissions in a patient’s route due to recall or confirmation bias that may have arisen from patient or proxy interviews.
However, the publicization of a patient’s route for the public’s benefit infringes upon the privacy of the patient. Thus, it is necessary to establish a protocol to protect privacy. Equally, more effort should be taken to provide accurate information to the public. Patient information that is unrelated to the communication of risk of infectious diseases must be protected by clearly defining the standards of publicization and reporting of patient information for the public’s benefit when an infectious disease is prevalent.
With regards to responding to the recent prevalence of COVID-19, Korea Centers for Disease Control and Prevention are performing defense activities to contain and prevent infection at the appropriate time, with more objective and accurate methods for monitoring patient contacts by using personal information. However, an evaluation of the effectiveness of these monitoring methods when multiple patients are involved, is necessary after the situation has been controlled. Epidemiological investigations require the collaboration of various related persons and must be conducted through a strict verification process. Furthermore, investigations must be performed using systematic processes with scientific methods and principles, and cycles of continuous evaluation and feedback to identify the etiology, extent, progression and therapy for the infectious disease and the development of public health policies.
Acknowledgments
We thank the relevant ministries, including the Ministry of Interior and Safety, Si/Do and Si/Gun/Gu, medical staff in health centers, and medical facilities for their efforts in responding to cases of COVID-19.
The COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, KCDC and Ministry of Health and Welfare (MOHW) who contributed to this article are as follows:
Ok Park, Young Joon Park, Shin Young Park, Young-Man Kim, Jieun Kim, Jin Lee, Eunmi Park, Dongwook Kim, Byoung-Hak Jeon, Boyeong Ryu, Daehyeon Ko, Eunyoung Kim, Hwami Kim, Hyeyoung Lee, Jin Gwack, Joongho Jo, Jung Hyun Lee, Junghee Hyun, Jungwoo Kim, Jae Kyung Park, Sangeun Lee, Seong Sun Kim, Seung Hwan Shin, Seung Woo Choi, Taeyoung Kim, Un-Na Kim (MOHW), Yeonhee Woo, Yeowon Jin, Yoon Suk Jang, Youngjoon Park, Minwoo Yum.
Notes
Conflicts of Interest
The authors declare no competing financial interests.