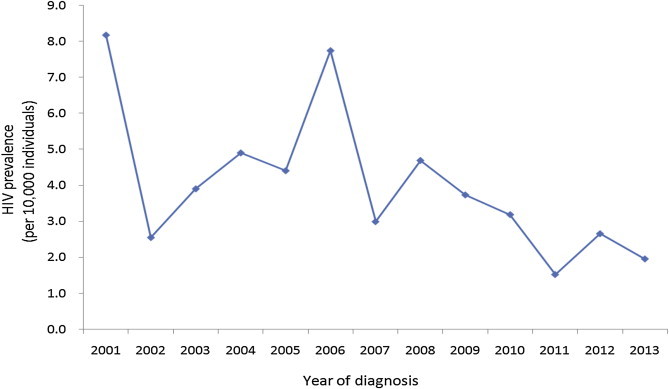
Figure 1The trend in human immunodeficiency virus seroprevalence in suspected tuberculosis cases at public health centers during 2001–2013 in Korea. HIV seroprevalence is presented as the number of confirmed HIV-infected individuals per 10,000 HIV-tested individuals among suspected tuberculosis cases at public health centers every year. HIV = human immunodeficiency virus.
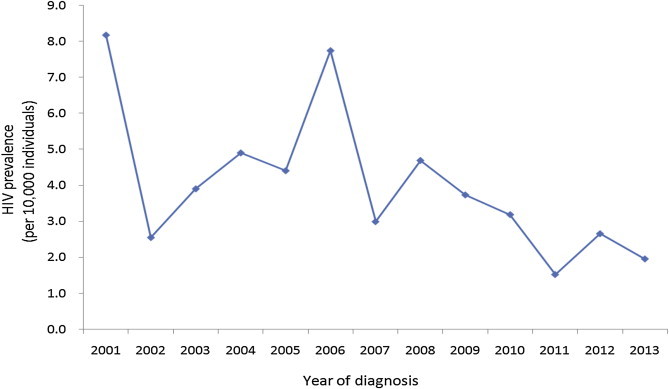
Table 1Human immunodeficiency virus testing of suspected tuberculosis patients in public health centers during 2001–2013 in Korea.
|
Year |
Total
|
HCIS
|
Frequency of testc
|
|
No. of HIV testsa
|
No. of PHCs |
No. of HIV tests |
No. of HCISb
|
|
2001 |
7,617 |
215 |
4,039 (53) |
114 |
1.10 |
|
2002 |
6,385 |
222 |
4,314 (68) |
150 |
1.10 |
|
2003 |
6,905 |
222 |
5,785 (84) |
186 |
1.13 |
|
2004 |
6,902 |
225 |
6,442 (93) |
210 |
1.05 |
|
2005 |
7,411 |
246 |
7,411 (100) |
246 |
1.09 |
|
2006 |
8,280 |
251 |
8,280 (100) |
251 |
1.07 |
|
2007 |
7,181 |
251 |
7,181 (100) |
251 |
1.07 |
|
2008 |
6,749 |
253 |
6,749 (100) |
253 |
1.05 |
|
2009 |
8,580 |
253 |
8,580 (100) |
253 |
1.07 |
|
2010 |
6,758 |
253 |
6,758 (100) |
253 |
1.07 |
|
2011 |
7,053 |
253 |
7,053 (100) |
253 |
1.07 |
|
2012 |
7,982 |
254 |
7,982 (100) |
254 |
1.06 |
|
2013 |
5,526 |
253 |
5,526 (100) |
253 |
1.08 |
Table 2Characteristics of the trends of human immunodeficiency virus test takers among suspected tuberculosis cases in public health centers during 2001–2013 in Korea.
|
2001
|
2002
|
2003
|
2004
|
2005
|
2006
|
2007
|
2008
|
2009
|
2010
|
2011
|
2012
|
2013
|
|
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
|
Total |
3,675 |
3,933 |
5,134 |
6,132 |
6,822 |
7,759 |
6,705 |
6,405 |
8,052 |
6,292 |
6,599 |
7,550 |
5,130 |
|
Sex |
|
Male |
2,514 (68.4) |
2,693 (68.5) |
3,586 (69.8) |
4,231 (69.0) |
4,676 (68.5) |
5,154 (66.4) |
4,565 (68.1) |
4,266 (66.6) |
5,314 (66.0) |
4,110 (65.3) |
4,130 (62.6) |
4,600 (60.9) |
3,290 (64.1) |
|
Female |
1,161 (31.6) |
1,240 (31.5) |
1,548 (30.2) |
1,901 (31.0) |
2,146 (31.5) |
2,605 (33.6) |
2,140 (31.9) |
2,139 (33.4) |
2,738 (34.0) |
2,182 (34.7) |
2,469 (37.4) |
2,950 (39.1) |
1,840 (35.9) |
|
Age (y) |
|
<20 |
387 (10.5) |
347 (8.8) |
430 (8.4) |
608 (9.9) |
677 (9.9) |
777 (10.0) |
848 (12.6) |
936 (14.6) |
1,123 (13.9) |
840 (13.4) |
988 (15.0) |
1,605 (21.3) |
903 (17.6) |
|
20–29 |
935 (25.4) |
1,062 (27.0) |
1,492 (29.1) |
1,435 (23.4) |
1,703 (25.0) |
1,891 (24.4) |
1,485 (22.1) |
1,248 (19.5) |
1,601 (19.9) |
1,121 (17.8) |
1,070 (16.2) |
1,015 (13.4) |
952 (18.6) |
|
30–39 |
624 (17.0) |
646 (16.4) |
1,004 (19.6) |
1,228 (20.0) |
1,167 (17.1) |
1,399 (18.0) |
1,134 (16.9) |
1,044 (16.3) |
1,313 (16.3) |
986 (15.7) |
1,003 (15.2) |
958 (12.7) |
624 (12.2) |
|
40–49 |
551 (15.0) |
588 (15.0) |
750 (14.6) |
956 (15.6) |
1,063 (15.6) |
1,208 (15.6) |
949 (14.2) |
971 (15.2) |
1,209 (15.0) |
1,005 (16.0) |
1,067 (16.2) |
1,097 (14.5) |
725 (14.1) |
|
50–59 |
409 (11.1) |
451 (11.5) |
523 (10.2) |
697 (11.4) |
739 (10.8) |
803 (10.3) |
790 (11.8) |
765 (11.9) |
970 (12.0) |
851 (13.5) |
1,027 (15.6) |
1,196 (15.8) |
753 (14.7) |
|
60 or older |
769 (20.9) |
839 (21.3) |
935 (18.2) |
1,208 (19.7) |
1,473 (21.6) |
1,681 (21.7) |
1,499 (22.4) |
1,441 (22.5) |
1,836 (22.8) |
1,489 (23.7) |
1,444 (21.9) |
1,679 (22.2) |
1,173 (22.9) |
|
Nationality |
|
Korean |
3,672 (99.9) |
3,922 (99.7) |
4,614 (89.9) |
5,775 (94.2) |
6,725 (98.6) |
7,376 (95.1) |
6,486 (96.7) |
6,261 (97.8) |
7,206 (89.5) |
5,877 (93.4) |
6,020 (91.2) |
7,112 (94.2) |
4,710 (91.8) |
|
Foreign |
3 (0.1) |
11 (0.3) |
520 (10.1) |
357 (5.8) |
97 (1.4) |
383 (4.9) |
219 (3.3) |
144 (2.2) |
846 (10.5) |
415 (6.6) |
579 (8.8) |
438 (5.8) |
420 (8.2) |
|
Region |
|
Metropolis |
2,011 (54.7) |
2,131 (54.2) |
2,651 (51.6) |
2,896 (47.2) |
3,289 (48.2) |
3,605 (46.5) |
3,791 (56.5) |
3,289 (51.4) |
3,617 (44.9) |
2,702 (42.9) |
2,480 (37.6) |
2,638 (34.9) |
2,037 (39.7) |
|
Small city or rural area |
1,664 (45.3) |
1,802 (45.8) |
2,483 (48.4) |
3,236 (52.8) |
3,533 (51.8) |
4,154 (53.5) |
2,914 (43.5) |
3,116 (48.6) |
4,435 (55.1) |
3,590 (57.1) |
4,119 (62.4) |
4,912 (65.1) |
3,093 (60.3) |
Table 3Characteristics of human immunodeficiency virus-infected individuals among suspected tuberculosis cases in public health centers in Korea (2001–2013).
|
N (%) |
|
Total |
32 (100) |
|
Sex |
|
Men |
30 (93.8) |
|
Women |
2 (6.2) |
|
Age (y) |
|
<20 |
0 (0.0) |
|
20–29 |
3 (9.4) |
|
30–39 |
11 (34.4) |
|
40–49 |
11 (34.4) |
|
50–59 |
5 (15.6) |
|
60 or older |
2 (6.2) |
|
Nationality |
|
Korean |
30 (93.8) |
|
Foreign |
2 (6.2) |
|
Region |
|
Metropolis |
17 (53.1) |
|
Small city or rural area |
15 (46.9) |




 PubReader
PubReader Cite
Cite
