Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 7(5); 2016 > Article
-
Original Article
Tuberculosis Notification Completeness and Timeliness in the Republic of Korea During 2012–2014 - Hae-Young Kang, Hyosoon Yoo, Wonseo Park, Unyeong Go, Eunkyeong Jeong, Ki-Suck Jung, Hyunjin Son
-
Osong Public Health and Research Perspectives 2016;7(5):320-326.
DOI: https://doi.org/10.1016/j.phrp.2016.08.002
Published online: September 21, 2016
Centers for Disease Control and Prevention, Cheongju, Korea
- ∗Corresponding author. hjson78@gmail.com
• Received: May 18, 2016 • Revised: July 6, 2016 • Accepted: August 1, 2016
© 2016 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- Completeness and timeliness are key attributes of accurate disease surveillance. This study aimed to evaluate the completeness and timeliness of tuberculosis (TB) notification in the Republic of Korea, by comparing notification data from the Korean National Tuberculosis Surveillance System and reimbursement data from the National Health Insurance.
-
Methods
- We evaluated reimbursement data from 103,075 cases (2012–2014) and surveillance data from 215,055 cases (2011–2015); cases were matched using Resident Registration Numbers. Completeness was evaluated using notifications that were reported within 365 days of the corresponding insurance claim. Timeliness was evaluated using the delay between starting TB treatment and the corresponding notification. Multivariate logistic regression analysis was used to analyze factors that affected completeness (e.g., sex, age, institution type, and nationality).
-
Results
- The completeness values were 90.0% in 2012 (33,094/36,775), 93.0% in 2013 (31,445/33,803), and 94.0% in 2014 (30,537/32,497). The rates of notification within 7 days of the corresponding claim were 81.6% in 2012 (27,323/33,489), 79.8% in 2013 (25,469/31,905), and 80.4% in 2014 (24,891/30,978). Increases over time were observed in the sex-, age-, institution type-, and nationality-specific analyses. Multivariate analyses revealed that completeness was affected by institution type [hospitals: odds ratio (OR) = 1.82, p < 0.001; general hospitals: OR = 4.18, p < 0.001] and nationality (native Korean status: OR = 1.48, p < 0.001).
-
Conclusion
- Notification completeness exhibited a 4.0% increase during 2012–2014 in Korea, and institution type and nationality significantly affected the completeness of TB notifications.
- Tuberculosis (TB) remains the highest public health priority in the Republic of Korea. In 2014, Korean surveillance detected 34,869 new cases (68.7/100,000 population) and 5,069 relapse cases (10.0/100,000 population) [1], as well as 2305 TB-related deaths (4.5/100,000 population) [2]. Since 2011, the Republic of Korea has enhanced its National Tuberculosis Control Program with a goal of reducing the incidence of TB to < 50/100,000 population by 2020. To achieve this goal, a 3-fold increase in TB management expenditures has been used to support various programs through a Public–Private Mix (PPM), which is anticipated to increase the completeness of TB notifications. PPM nurses assumed full charge of TB patients, performing thorough patient management tasks such as reporting TB patients, case investigations, consultations, nonadherence patient management, hospital order for nonadherence patients. In this context, complete notification regarding TB cases is critical to initiating appropriate public control measures (e.g., contact investigation) and case management (e.g., directly observed therapy).
- According to the World Health Organization's 2015 Global Tuberculosis Report, the Korean incidence of TB in 2014 was 86/100,000 population [3]. This rate includes officially notified new and relapse cases (78.7/100,000 population), as well as an estimate of nonnotified TB cases. Therefore, studies regarding the completeness of TB notification in Korea are needed to obtain an accurate estimate of the incidence of TB. However, only a few studies have evaluated the completeness of TB notifications in the Republic of Korea, and these studies found relatively low estimates of 68.1% in 2006 [4] and 57.1% in 2008 [5]. Moreover, the findings of these studies were limited by their use of a physician-completed sampling survey or analyses of data from a single year.
- In the Republic of Korea, physicians originally reported cases of TB using a paper format, according to the Act on Tuberculosis Prevention Article 8 (notification obligations of healthcare providers) and the Enforcement Regulation of TB Prevention Act. This notification is mandatory when a physician diagnoses or treats a patient with confirmed or suspected TB, or when a physician or other medical personnel perform a postmortem examination for a confirmed or suspected case of TB. A web-based notification system was implemented in 2000, which allows physicians to notify the Korean National Tuberculosis Surveillance System (KNTSS) regarding cases of TB. In addition, treatment reimbursement for cases of TB is documented in the Tuberculosis Registry of the National Health Insurance (NHI) program. Therefore, the present study aimed to evaluate the completeness of the web-based notification system using the 2012–2014 data from the NHI database.
Introduction
- The completeness of the TB notification system in the Republic of Korea was evaluated for 2012–2014, by matching KNTSS notifications with claims data from the NHI database. The present study included all patients who were diagnosed with TB, based on the Tuberculosis Prevention Act and the National Tuberculosis Management Guidelines for the Republic of Korea. The exclusion criteria were duplicated data and data from public health centers, which do not receive treatment reimbursement from the NHI. All data were anonymized prior to the analyses.
- 2.1 Healthcare facilities in the Republic of Korea
- In the Republic of Korea, almost all TB cases are diagnosed and treated in private medical institutions, which can be categorized as general hospitals, hospitals, and clinics. Clinics typically provide medical treatment to outpatients, hospitals typically have > 30 beds and provide medical treatment to inpatients, and general hospitals typically have >100 beds and provide medical treatment to inpatients. In 2014, 91.4% of all TB notifications were from private medical institutions (general hospital, 78.9%; hospital, 9.5%; clinic, 3.0%), and only 8.6% of all notifications were from public health centers.
- 2.2 NHI TB registry
- The Republic of Korea's NHI covers 99.9% of the general population (approximately 50 million people), which includes the 3.6% of the population who receive Medical Aid (approximately 1.8 million people) [6]. Since April 2011, the NHI has provided additional reimbursement to enhance TB treatment access, which now covers 95% of the related medical costs (5% are paid out of pocket). However, to receive reimbursement, physicians must register TB cases with the NHI system. The present study evaluated 2,161,967 registered cases of newly diagnosed TB that were treated between 2012 and 2014. The NHI data include the patients' personal information [demographic characteristics and Resident Registration Number (RRN)], date of started treatment, and amount of reimbursement.
- 2.3 Korean National Tuberculosis Surveillance System
- The KNTSS web-based notification system was launched in August 2000 to notify the Korea Centers for Disease Control and Prevention of individual TB cases. Thus, the KNTSS receives notifications regarding most patients who are diagnosed with or treated for TB in private medical facilities. The notification data include the patients' personal information (demographic characteristics and RRN), examination results, treatments, and treatment outcomes. The present study evaluated 215,055 notifications within a 5-year period (2011–2015).
- 2.4 Notification completeness
- The present study assumed that the vast majority of TB cases would be registered with the NHI, as most TB cases are diagnosed or treated in private medical institutions. Thus, the TB notification completeness was calculated as the number of notified cases (KNTSS data, 2011–2015) divided by the number of newly registered TB cases (NHI data, 2012–2014), which were matched using the patients' RRNs. The wider time frame for the KNTSS data was used because physicians and other medical personnel occasionally delay the notification to the KNTSS database.
- 2.5 Notification timeliness
- Notification timeliness was defined as the difference between the date of starting treatment (NHI data) and the date of the KNTSS notification. The differences were categorized as < 7, < 30, < 60, < 90, < 180, and < 365 days. We also calculated the proportions of the notified cases for each lag period by dividing the number of notifications by the total number of notified cases for each period.
- 2.6 Statistical analysis
- Multivariate logistic regression analyses were performed to analyze the factors that affected TB notification completeness. Factors were selected using a stepwise approach, and odds ratios were calculated after adjusting for sex, age group, institution type, and patient nationality. All analyses were performed using the SAS software (version 9.4), and differences with a p value of < 0.05 were considered statistically significant.
Materials and methods
- Figure 1 shows the study flowchart based on the 2012–2014 NHI data, and the calculations for notification completeness. Among the 2,161,967 TB cases that received NHI reimbursement, we found 2,058,892 claims for ≥ 2 rounds of treatment using the patients' RRNs. To evaluate data for each patient's first treatment only, we excluded the records for later claims and only analyzed data from 103,075 first-claim treatment records. These first-claim records included 36,775 cases of TB in 2012, 33,803 cases of TB in 2013, and 32,497 cases of TB in 2014. We evaluated notification completeness by comparing the number of KNTSS notifications with a < 365-day lag to the corresponding number of NHI claims for each year. These analyses revealed notification completeness values of 90.0% in 2012 (33,094/36,775), 93.0% in 2013 (31,445/33,803), and 94.0% in 2014 (30,537/32,497).
- Table 1 shows the results from the TB notification timeliness analyses according to the various lag periods. Table 2 shows the completeness analyses results according to sex, age group, institution type, nationality, and change in completeness over time. The completeness values increased during the study period for most subgroups, with the exception of clinics, which exhibited a minor decrease during the study period. All sex and age groups exhibited TB notification completeness of ≥ 90% after 2013. The TB notification completeness for foreigners was lower than that for native Koreans, and the increase for foreigners (3.5%) was slightly smaller than that for native Koreans (4.0%).
- Table 3 shows the overall notification completeness values for 2012–2014, and the factors that affected completeness. Sex and age groups did not significantly affect TB notification completeness. Institution type significantly affected TB notification completeness, with adjusted odds ratios of 4.18 for general hospitals and 1.82 for hospitals, compared to clinics. Compare to foreigners, native Koreans exhibited an adjusted odds ratio of 1.48 for completeness.
- In the present study, we considered the potential effects of reporting lag in our comparisons of the NHI and KNTSS data, by considering KNTSS notifications that were received within 365 days after the corresponding NHI claim. However, when we included all notifications (regardless of lag), the TB notification completeness values increased to 91.1% (33,489/36,775) in 2012 (+1.1%), 94.4% (31,905/33,803) in 2013 (+1.4%), and 95.3% (30,978/32,497) in 2014 (+1.3%). However, the rates of notification within 7 days from the corresponding NHI claim decreased to 74.3% (27,323/36,775) in 2012 (−15.7%), 75.3% (25,469/33,803) in 2013 (−17.7%), and 76.6% (24,891/32,497) in 2014 (−17.4%). The rates of notifications within 30 days from the corresponding NHI claim were 81.8% (30,094/36,775) in 2012 (−8.2%), 85.0% (28,732/33,803) in 2013 (−8.0%), and 84.9% (27,606/32,497) in 2014 (−9.1%). The rates of notifications within 180 days from the corresponding NHI claim were 87.5% (32,187/36,775) in 2012 (−2.5%), 90.9% (30,737/33,803) in 2013 (−2.1%), and 91.2% (29,633/32,497) in 2014 (−2.8%).
Results
- In the present study, the proportions of TB notifications within 7 days were 81.6% in 2012 (27,323/33,489), 79.8% in 2013 (25,469/31,905), and 80.4% in 2014 (24,891/30,978). However, the notification completeness values for newly diagnosed cases were 90.0% in 2012, 93.0% in 2013, and 94.0% in 2014. These findings indicate that the current notification completeness in the Republic of Korea is higher than the values from previous studies (68.1% in 2006 and 57.1% in 2008) 4, 5. Furthermore, these findings indicate that the current completeness and timeliness values for TB notification in the Republic of Korea are comparable to those from other countries. Lo et al [7] used NHI data to analyze timeliness of TB reporting in Taiwan, and found that 81.8% of the cases were reported within 7 days, with notification completeness values of 95.5% in 2005, 96.8% in 2006, and 96.8% in 2007. Furthermore, Curtis et al [8] evaluated American data from laboratory logbooks, death certificates, hospital discharge records, Medicaid databases, and pharmacy databases in seven states during 1993–1994, and found that the rate of timely reporting (< 7 days) ranged from 47% to 95% in their state-, city-, and source-specific analyses. Moreover, TB notification completeness was 99.5% in that study. Trepka et al [9] evaluated TB notification completeness in Wisconsin, and found that the 1995 rates were 98.9% using laboratory data and 98.0% using hospital discharge data. Driver et al [10] also found that TB notification completeness for Puerto Rico was 80.5% in 1992, using data from hospital discharge records, pharmacy listings for anti-TB medications, and laboratory and Acquired Immunodeficiency Syndrome registry databases.
- We also compared the annual reimbursement claims from the NHI report [11] with TB notification data (newly diagnosed and relapsed cases) [1] in the Republic of Korea over the past decade (2004–2014; Figure 2). A gradual decrease was observed in the annual number of reimbursement claims based on TB-related International Classification of Diseases (ICD)-10 codes (A15–A19), although the overall TB notification completeness remained stable. However, given that NHI claims data may have multiple claims during the same year (using codes A15–A19), and that not all cases necessarily involve patients with TB, it is difficult to interpret the absolute value of this comparison. In contrast, the present study revealed a gradual decrease in TB notifications, from 36,775 in 2012 to 32,497 in 2014, and the parallel decreases in the NHI and KNTSS data suggest that the incidence of TB is gradually decreasing in the Republic of Korea. The reliability of this finding is supported by the high completeness of the TB notification data, and the 4.0% increase in completeness from 2012 to 2014 suggests that the recent improvements in the National Tuberculosis Control Program have been effective. These effects may be related to improvements in the rate of individuals with TB symptoms seeking medical attention, and improvements in KNTSS notifications from general hospitals, hospitals, and clinics. Moreover, the present study only evaluated medical institutions, and it is possible that the completeness rates are underestimated, as a small proportion of TB cases are diagnosed and treated in public health centers. As patients diagnosed and treated in public health centers are all reported, the TB notification completeness in the Republic of Korea for 2014 may be considered to be higher than 94.0%.
- The multivariate analyses revealed that TB notification completeness is affected by the type of medical institution, as we observed adjusted odds ratios of 4.18 for general hospitals and 1.82 for hospitals, compared to clinics. In addition, we observed institution-specific changes in completeness, with general hospitals exhibiting an increase of 4.3%, hospitals exhibiting an increase of 2.6%, and clinics exhibiting a change of −2.1%. These findings are consistent with the findings of Lo et al [7], who reported that TB notification completeness was lower in Taiwanese clinics, compared to Taiwanese hospitals. Although hospitals and clinics accounted for a relatively small proportion of the present study's sample (11,983/103,075; 11.6%), additional efforts may need to target these centers if they are to achieve a TB notification completeness of > 94%. Furthermore, the present study revealed that high TB notification completeness was associated with older age groups, native Korean status, and general hospitals; these findings are also similar to the findings of Lo et al [7].
- The present study has several limitations that warrant consideration. First, only a small proportion of NHI data variables were used, which made it impossible to analyze the variables according to the type of TB, bacteriological test results, and socioeconomic status. Second, a > 7-day delay in reporting was observed in approximately 20% of the cases, which highlights the need for more specific analysis. Third, we only considered the timeliness and completeness of notifications for the first diagnosis and treatment.
- The present study revealed that TB notification completeness values in the Republic of Korea increased by 4.0% during the study period, from 90.0% in 2012 to 94.0% in 2014. Furthermore, the type of medical institution and patient nationality appeared to have the greatest effect on notification completeness.
Discussion
- The authors have no financial, general, or institutional conflicts of interest.
Conflicts of interest
- 1. Korea Centers for Disease Control and Prevention, Republic of Korea [Internet] . Annual report on notified tuberculosis in Korea 2014. 2015. [cited 2015 Jul 31]. Available from:. http://tbzero.cdc.go.kr/tbzero/board/boardList.do.
- 2. Statistics Korea, Republic of Korea [Internet] . Annual report on the cause of death statistics 2014. 2015. [cited 2015 Sep 23]. Available from:. http://kostat.go.kr/portal/english/index.action.
- 3. http://www.who.int/tb/publications/global_report/en/.
- 4. Korea Centers for Disease Control and Prevention, Republic of Korea . K.A.P (Knowledge, Attitude, Practice) study of physicians for improving performance of communicable diseases surveillance system. 2006.
- 5. Korea Centers for Disease Control and Prevention, Republic of Korea . Nationwide medical records survey of patients with tuberculosis. 2010.
- 6. World Health Organization [Internet] . Republic of Korea country health information profile. 2012. [cited 2015 Oct 28]. Available from:. http://www.who.int/gho/countries/kor.pdf?ua=1http://www.who.int/countries/en/.
- 7. Lo H.Y., Yang S.L., Chou P.. Completeness and timeliness of tuberculosis notification in Taiwan. BMC Public Health 11:2011 Dec;915PMID: 22151346.ArticlePubMed
- 8. Curtis A.B., McCray E., McKenna M.. Completeness and timeliness of tuberculosis case reporting. A multistate study. Am J Prev Med 20(2). 2001 Feb;108−112. PMID: 11165451.PubMed
- 9. Trepka M.J., Beyer T.O., Proctor M.E.. An evaluation of the completeness of tuberculosis case reporting using hospital billing and laboratory data; Wisconsin, 1995. Ann Epidemiol 9(7). 1999 Oct;419−423. PMID: 10501409.ArticlePubMed
- 10. Driver C.R., Braden C.R., Nieves R.L.. Completeness of tuberculosis case reporting, San Juan and Caguas Regions, Puerto Rico, 1992. Public Health Rep 111(2). 1996 Mar–Apr;157−161. PMID: 8606915.PubMed
- 11. https://www.hira.or.kr/eng/index.html#&panel1-1.
References
Figure 1Flow chart for calculating completeness of tuberculosis notification in the Republic of Korea, 2012–2014.
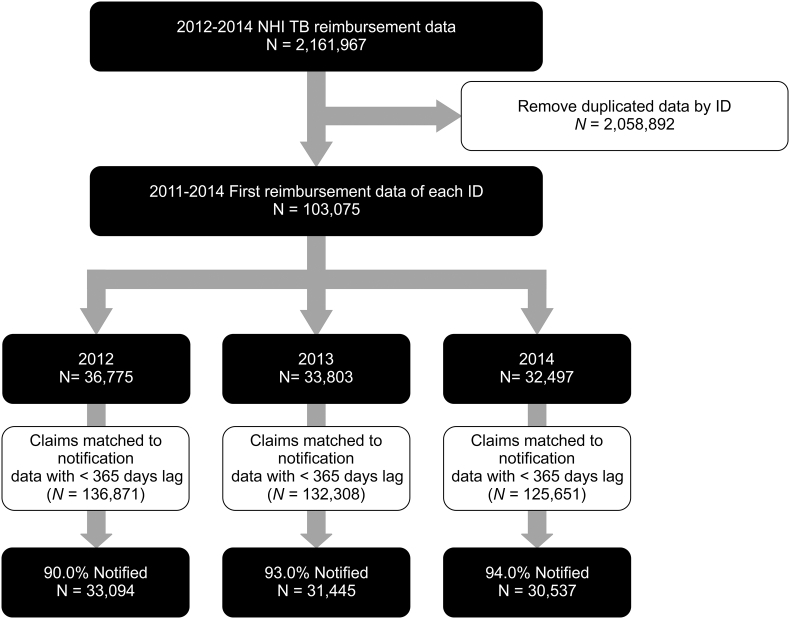
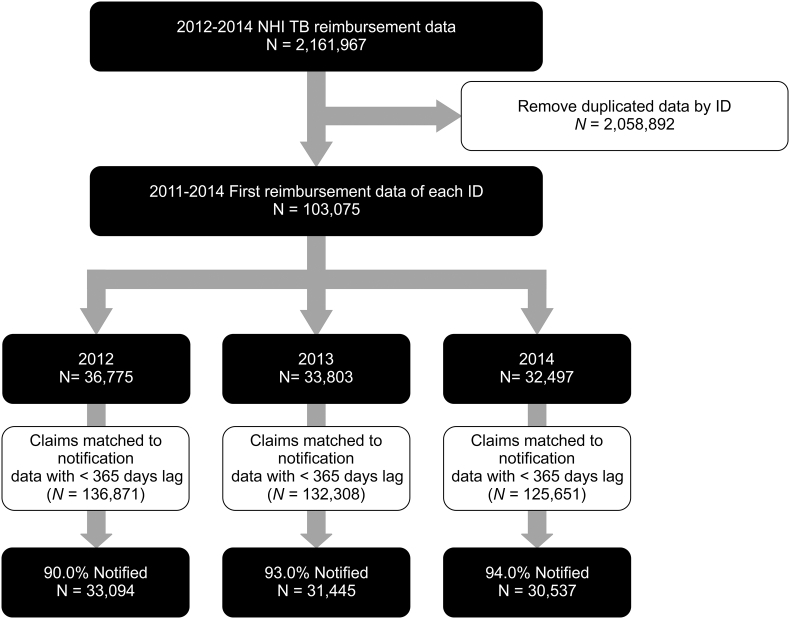
Figure 2Trends in National Health Insurance claims using tuberculosis-related ICD-10 codes (A15–A19) and tuberculosis notifications (new and relapse cases). ICD-10 = International Classification of Diseases, version 10.
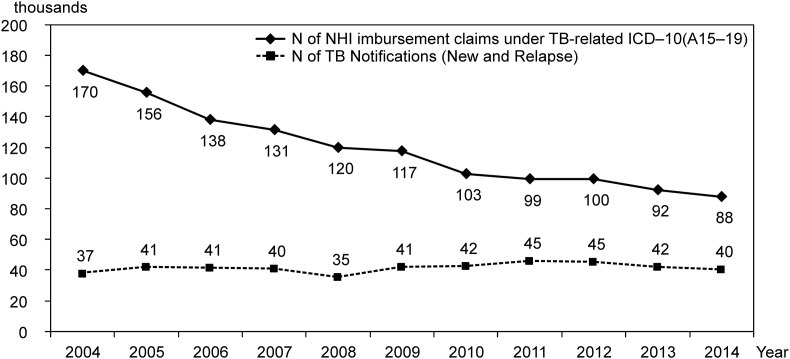
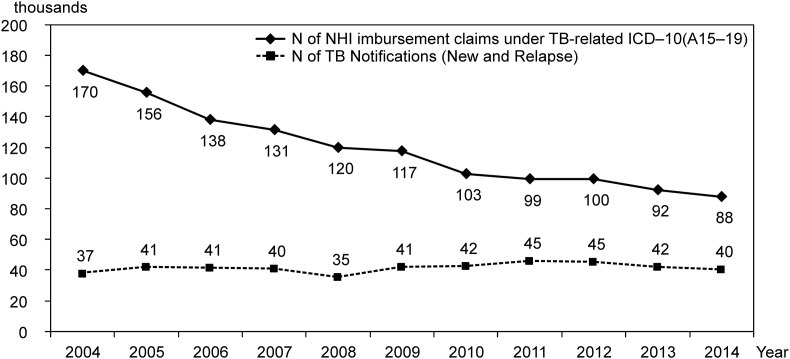
Table 1Timeliness of tuberculosis notification in the Republic of Korea (2012–2014).
Table 2Completeness of tuberculosis notification according to sex, age group, institution type, and nationality in the Republic of Korea (2012–2014).
Table 3Factors that were associated with completeness of tuberculosis notification in the Republic of Korea (2012–2014).
|
2012–2014 |
Adjusted ORa | p | 95% CI | ||
|---|---|---|---|---|---|
|
NHI n |
Notified n (%) |
||||
| Total | 103,075 | 95,076 (92.2) | |||
| Sex | |||||
| Female | 44,706 | 41,223 (92.2) | |||
| Male | 58,369 | 53,853 (92.3) | |||
| Age group (y) | |||||
| 0–19 | 3,401 | 3,136 (92.2) | |||
| 20–39 | 25,038 | 23,059 (92.1) | |||
| 40–59 | 32,410 | 29,797 (91.9) | |||
| ≥ 60 | 42,226 | 39,084 (92.6) | |||
| Type of medical institution | |||||
| Clinic | 2,695 | 2,074 (77.0) | 1.00 | ||
| Hospital | 9,288 | 7,982 (85.9) | 1.82 | 0.001 | 1.64–2.03 |
| General hospital | 91,092 | 85,020 (93.3) | 4.18 | 0.001 | 3.81–4.59 |
| Nationality | |||||
| Foreign | 2,509 | 2,230 (88.9) | 1.00 | ||
| Native | 100,566 | 92,846 (92.3) | 1.48 | 0.001 | 1.31–1.69 |
Figure & Data
References
Citations
Citations to this article as recorded by 

- Nationwide Treatment Outcomes of Patients With Multidrug/Rifampin-Resistant Tuberculosis in Korea, 2011–2017: A Retrospective Cohort Study (Korean TB-POST)
Hongjo Choi, Jeongha Mok, Young Ae Kang, Dawoon Jeong, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Doosoo Jeon
Journal of Korean Medical Science.2023;[Epub] CrossRef - Retreatment after loss to follow-up reduces mortality in patients with multidrug/rifampicin-resistant tuberculosis
Hongjo Choi, Jeongha Mok, Young Ae Kang, Dawoon Jeong, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Doosoo Jeon
ERJ Open Research.2023; 9(4): 00135-2023. CrossRef - Cohort Profile: Korean Tuberculosis and Post-Tuberculosis Cohort Constructed by Linking the Korean National Tuberculosis Surveillance System and National Health Information Database
Dawoon Jeong, Hee-Yeon Kang, Jinsun Kim, Hyewon Lee, Bit-Na Yoo, Hee-Sun Kim, Hongjo Choi
Journal of Preventive Medicine and Public Health.2022; 55(3): 253. CrossRef - Hidden loss to follow-up among tuberculosis patients managed by public–private mix institutions in South Korea
Hyung Woo Kim, Sohee Park, Jinsoo Min, Jiyu Sun, Ah Young Shin, Jick Hwan Ha, Jae Seuk Park, Sung-Soon Lee, Marc Lipman, Ibrahim Abubakar, Helen R. Stagg, Ju Sang Kim
Scientific Reports.2022;[Epub] CrossRef - Assessing the Quality of Reporting to China’s National TB Surveillance Systems
Tao Li, Lijia Yang, Sarah E. Smith-Jeffcoat, Alice Wang, Hui Guo, Wei Chen, Xin Du, Hui Zhang
International Journal of Environmental Research an.2021; 18(5): 2264. CrossRef - Quality and Utility of Information Captured by Surveillance Systems Relevant to Antimicrobial Resistance (AMR): A Systematic Review
Mustafa Al-Haboubi, Rebecca E. Glover, Elizabeth Eastmure, Mark Petticrew, Nick Black, Nicholas Mays
Antibiotics.2021; 10(4): 431. CrossRef - Risk of tuberculosis in patients with cancer treated with immune checkpoint inhibitors: a nationwide observational study
Seongman Bae, Ye-Jee Kim, Min-ju Kim, Jwa Hoon Kim, Sung-Cheol Yun, Jiwon Jung, Min Jae Kim, Yong Pil Chong, Sung-Han Kim, Sang-Ho Choi, Yang Soo Kim, Sang-Oh Lee
Journal for ImmunoTherapy of Cancer.2021; 9(9): e002960. CrossRef - Underreporting of patients diagnosed with tuberculosis in the Region of Southern Denmark
Frederik D. Thrane, Peter H. Andersen, Isik S. Johansen, Inge K. Holden
Scandinavian Journal of Public Health.2020; 48(8): 870. CrossRef - Effects of particulate air pollution on tuberculosis development in seven major cities of Korea from 2010 to 2016: methodological considerations involving long-term exposure and time lag
Honghyok Kim, Sarah Yu, Hongjo Choi
Epidemiology and Health.2020; 42: e2020012. CrossRef - Latent tuberculosis infection screening and treatment in congregate settings (TB FREE COREA): protocol for a prospective observational study in Korea
Jinsoo Min, Hyung Woo Kim, Helen R Stagg, Marc Lipman, Molebogeng X Rangaka, Jun-Pyo Myong, Hyeon Woo Yim, Jeong Uk Lim, Yunhee Lee, Hyeon-Kyoung Koo, Sung-Soon Lee, Jae Seuk Park, Kyung Sook Cho, Ju Sang Kim
BMJ Open.2020; 10(2): e034098. CrossRef - Tuberculosis Surveillance and Monitoring under the National Public-Private Mix Tuberculosis Control Project in South Korea 2016–2017
Jinsoo Min, Hyung Woo Kim, Yousang Ko, Jee Youn Oh, Ji Young Kang, Joosun Lee, Young Joon Park, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2020; 83(3): 218. CrossRef - Prediction of treatment failure and compliance in patients with tuberculosis
Hyeon-Kyoung Koo, Jinsoo Min, Hyung Woo Kim, Joosun Lee, Ju Sang Kim, Jae Seuk Park, Sung-Soon Lee
BMC Infectious Diseases.2020;[Epub] CrossRef - Impact of COVID-19 Pandemic on the National PPM Tuberculosis Control Project in Korea: the Korean PPM Monitoring Database between July 2019 and June 2020
Jinsoo Min, Hyung Woo Kim, Hyeon-Kyoung Koo, Yousang Ko, Jee Youn Oh, Jaetae Kim, Jiyeon Yang, Yunhyung Kwon, Young-Joon Park, Ji Young Kang, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Journal of Korean Medical Science.2020;[Epub] CrossRef - Clinical profiles of early and tuberculosis-related mortality in South Korea between 2015 and 2017: a cross-sectional study
Jinsoo Min, Ju Sang Kim, Hyung Woo Kim, Ah Young Shin, Hyeon-Kyoung Koo, Sung-Soon Lee, Yang-Ki Kim, Kyeong-Cheol Shin, Jung Hyun Chang, Gayoung Chun, Joosun Lee, Mi Sun Park, Jae Seuk Park
BMC Infectious Diseases.2019;[Epub] CrossRef - Treatment outcomes and factors affecting treatment outcomes of new patients with tuberculosis in Busan, South Korea: a retrospective study of a citywide registry, 2014–2015
Jeongha Mok, Daeseong An, Seoungjin Kim, Miyoung Lee, Changhoon Kim, Hyunjin Son
BMC Infectious Diseases.2018;[Epub] CrossRef - Tuberculosis prevention and care in Korea: Evolution of policy and practice
Unyeong Go, Misun Park, Un-Na Kim, Sodam Lee, Sunmi Han, Joosun Lee, Jiyeon Yang, Jieun Kim, Shinyoung Park, Youngman Kim, Hyosoon Yoo, Jeongok Cha, Wonseo Park, Haeyoung Kang, Hwon Kim, Guri Park, Minjung Kim, Ok Park, Hyunjin Son, Enhi Cho, Kyoungin Na,
Journal of Clinical Tuberculosis and Other Mycobac.2018; 11: 28. CrossRef - The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 korean community health survey of 156,747 participants
JooYeon Seo, BoYoul Choi, Shinah Kim, HyeYoung Lee, DongHoon Oh
BMC Public Health.2017;[Epub] CrossRef - Vitamin D Deficiency among Adults with History of Pulmonary Tuberculosis in Korea Based on a Nationwide Survey
Mi Joo, Mi Han, Sun Park, Hwan Shin
International Journal of Environmental Research an.2017; 14(4): 399. CrossRef - Tuberculosis Control in the Republic of Korea
Cho, Kyung Sook
Health and Social Welfare Review.2017; 37(4): 179. CrossRef


 PubReader
PubReader Cite
Cite
