Search
- Page Path
- HOME > Search
- Drug resistance and the genotypic characteristics of rpoB and katG in rifampicin- and/or isoniazid-resistant Mycobacterium tuberculosis isolates in central Vietnam
- Thi Binh Nguyen Nguyen, Thi Kieu Diem Nguyen, Van Hue Trương, Thi Tuyet Ngoc Tran, van Bao Thang Phan, Thi Tuyen Nguyen, Hoang Bach Nguyen, Viet Quynh Tram Ngo, Van Tuan Mai, Paola Molicotti
- Osong Public Health Res Perspect. 2023;14(5):347-355. Published online October 18, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0124
- 1,116 View
- 76 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 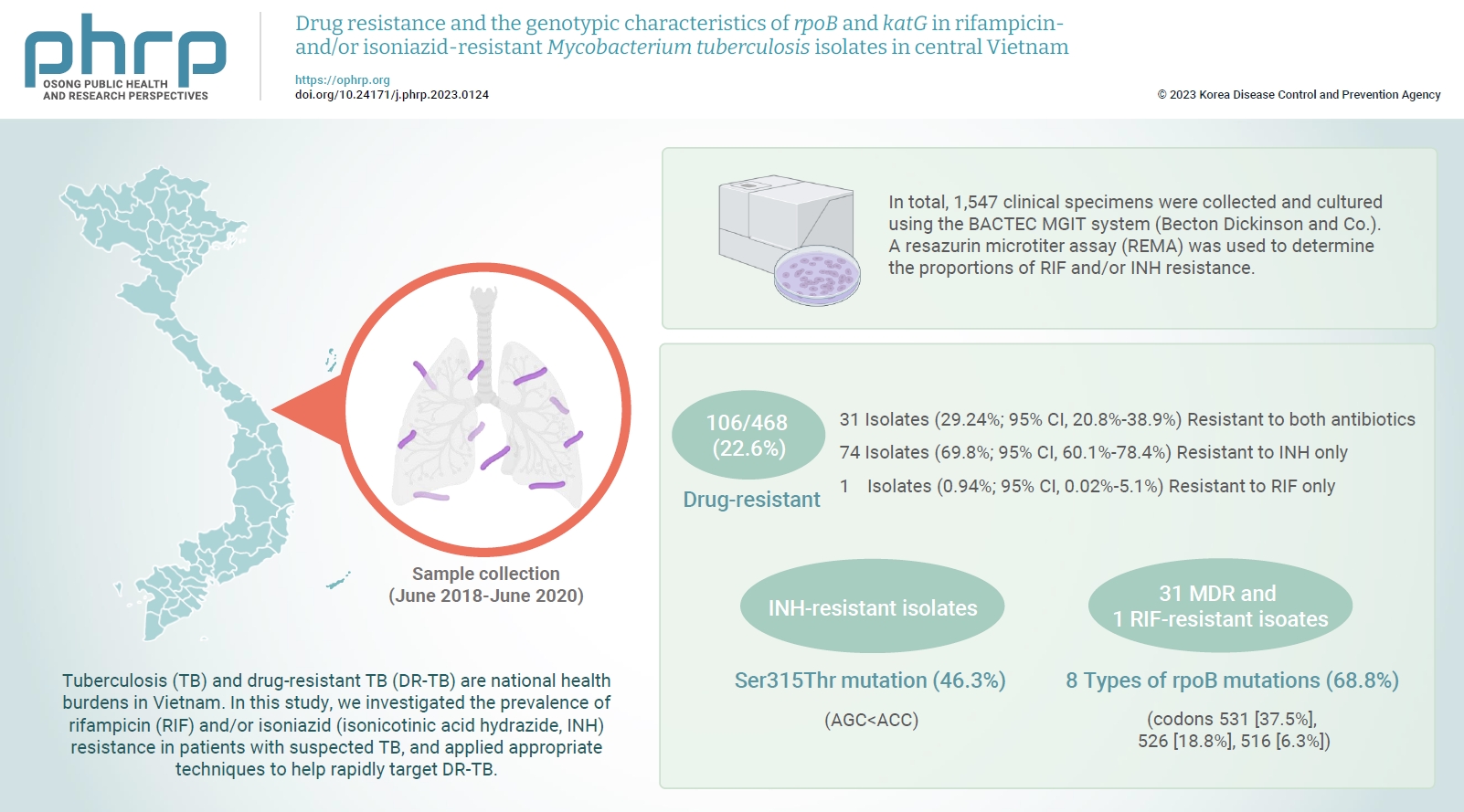
- Objectives
Tuberculosis (TB) and drug-resistant TB (DR-TB) are national health burdens in Vietnam. In this study, we investigated the prevalence of rifampicin (RIF) and/or isoniazid (isonicotinic acid hydrazide, INH) resistance in patients with suspected TB, and applied appropriate techniques to help rapidly target DR-TB. Methods: In total, 1,547 clinical specimens were collected and cultured using the BACTEC MGIT system (Becton Dickinson and Co.). A resazurin microtiter assay (REMA) was used to determine the proportions of RIF and/or INH resistance. A real-time polymerase chain reaction panel with TaqMan probes was employed to identify the mutations of rpoB and katG associated with DR-TB in clinical isolates. Genotyping of the identified mutations was also performed. Results: A total of 468 Mycobacterium tuberculosis isolates were identified using the REMA. Of these isolates, 106 (22.6%) were found to be resistant to 1 or both antibiotics. Of the resistant isolates, 74 isolates (69.8%) were resistant to isoniazid (INH) only, while 1 isolate (0.94%) was resistant to RIF only. Notably, 31 isolates (29.24%) were resistant to both antibiotics. Of the 41 phenotypically INH-resistant isolates, 19 (46.3%) had the Ser315Thr mutation. There were 8 different rpoB mutations in 22 (68.8%) of the RIF-resistant isolates. The most frequently detected mutations were at codons 531 (37.5%), 526 (18.8%), and 516 (6.3%). Conclusion: To help prevent new cases of DR-TB in Vietnam, it is crucial to gain a comprehensive understanding of the genotypic DR-TB isolates.
- A low risk of nosocomial transmission of subclinical tuberculosis to neonates in a postpartum care center under COVID-19 control measures
- In Kyoung Kim, So Jung Kim, Kyoung Hee Bae, Mi Young Kim, Ji Eun Oh, Mi Gyeong Lee, Young Ae Kang, Jin Su Song
- Osong Public Health Res Perspect. 2022;13(6):448-452. Published online December 16, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0235
- 2,087 View
- 98 Download
-
 Abstract
Abstract
 PDF
PDF - We report the results of investigating and managing a tuberculosis (TB) exposure in apostpartum care center. Among the contacts exposed to a nursing assistant with subclinical TB,5 of 44 neonates (11.4%) had positive tuberculin skin tests (TSTs) at 3 months of age, and all theTST-positive neonates received the Bacille Calmette-Guérin vaccination. Seven of 28 healthcareworkers (25.0%) and 1 of 3 household contacts (33.3%) were positive in the initial or repeatedinterferon-gamma release assay. None of the contacts developed TB disease during the studyperiod. Annual TB examinations of healthcare personnel at a postpartum care center under theTuberculosis Prevention Act in South Korea enabled the early detection of subclinical TB, whichreduced the risk of transmission to neonates under strict coronavirus disease 2019 preventionmeasures.
- Delays in the diagnosis and treatment of tuberculosis during the COVID-19 outbreak in the Republic of Korea in 2020
- Jiyeon Yang, Yunhyung Kwon, Jaetae Kim, Yoojin Jang, Jiyeon Han, Daae Kim, Hyeran Jeong, Hyekyung Park, Eunhye Shim
- Osong Public Health Res Perspect. 2021;12(5):293-303. Published online September 23, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0063
- 7,322 View
- 188 Download
- 8 Web of Science
- 8 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
We investigated the impact of the coronavirus disease 2019 (COVID-19) pandemic on tuberculosis (TB) management in the Republic of Korea (ROK).
Methods
This retrospective cross-sectional study used nationwide ROK TB notification data (98,346 cases) from 2017 to 2020. The median time from the onset of TB symptoms to treatment initiation and the compliance rates with the required timing for notification and individual case investigations were measured and compared across periods and regions affected by the COVID-19 epidemic.
Results
TB diagnosis during the COVID-19 pandemic was delayed. The median time to TB treatment initiation (25 days) in 2020 increased by 3 days compared to that of the previous 3 years (22 days) (p<0.0001). In the outbreak in Seoul, Incheon, and Gyeonggi province during August, the time to TB diagnosis was 4 days longer than in the previous 3 years (p=0.0303). In the outbreak in Daegu and Gyeongbuk province from February to March 2020, the compliance rate with the required timing for individual case investigations was 2.2%p points lower than in other areas in 2020 (p=0.0148). For public health centers, the rate was 13%p lower than in other areas (80.3% vs. 93.3%, p=0.0003).
Conclusion
TB diagnoses during the COVID-19 pandemic in the ROK were delayed nationwide, especially for patients notified by public-private mix TB control hospitals. TB individual case investigations were delayed in regional COVID-19 outbreak areas (Daegu and Gyeongbuk province), especially in public health centers. Developing strategies to address this issue will be helpful for sustainable TB management during future outbreaks. -
Citations
Citations to this article as recorded by- A Review of the Impact of Patent Medicine Vendors in Driving Community Tuberculosis Case Finding in the COVID-19 Pandemic in Nigeria
Arinze Emmanuel Ajogwu, Onwubiko Iheanyichukwu Samuel, Nnanyelugo Longinus Ochike, Uzoma Chidinma Ajegbo, Chinedu Paschal Maduka
Matrix Science Medica.2024; 8(2): 33. CrossRef - Tuberculosis: Republic of Korea, 2021
Jinsoo Min, Hyung Woo Kim, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2023; 86(1): 67. CrossRef - Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study
Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Jeong Mi Seo, Hongjo Choi, Young Ae Kang
BMJ Open.2023; 13(3): e069642. CrossRef - Increased Healthcare Delays in Tuberculosis Patients During the First Wave of COVID-19 Pandemic in Korea: A Nationwide Cross-Sectional Study
Jinsoo Min, Yousang Ko, Hyung Woo Kim, Hyeon-Kyoung Koo, Jee Youn Oh, Yun-Jeong Jeong, Hyeon Hui Kang, Kwang Joo Park, Yong Il Hwang, Jin Woo Kim, Joong Hyun Ahn, Yangjin Jegal, Ji Young Kang, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Time trend prediction and spatial–temporal analysis of multidrug-resistant tuberculosis in Guizhou Province, China, during 2014–2020
Wang Yun, Chen Huijuan, Liao Long, Lu Xiaolong, Zhang Aihua
BMC Infectious Diseases.2022;[Epub] CrossRef - Real-world association of adherence with outcomes and economic burden in patients with tuberculosis from South Korea claims data
Sun-Hong Kwon, Jin Hyun Nam, Hye-Lin Kim, Hae-Young Park, Jin-Won Kwon
Frontiers in Pharmacology.2022;[Epub] CrossRef - The Impact of the COVID-19 Pandemic on Tuberculosis Case Notification and Treatment Outcomes in Eswatini
Hloniphile Victory Masina, I-Feng Lin, Li-Yin Chien
International Journal of Public Health.2022;[Epub] CrossRef - Trends in incidences of newly notified tuberculosis in Jeju Province, Korea, 2017-2021
Jinhee Kim, Nam-Hun Kang, Jong-Myon Bae
Journal of Medicine and Life Science.2022; 19(3): 103. CrossRef
- A Review of the Impact of Patent Medicine Vendors in Driving Community Tuberculosis Case Finding in the COVID-19 Pandemic in Nigeria
- Army Soldiers’ Knowledge of, Attitude Towards, and Preventive Behavior Towards Tuberculosis in Korea
- Yun Choi, Geum Hee Jeong
- Osong Public Health Res Perspect. 2018;9(5):269-277. Published online October 31, 2018
- DOI: https://doi.org/10.24171/j.phrp.2018.9.5.09
- 6,323 View
- 150 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The aim of this study was to gather information about Korean Army soldiers’ attitude towards tuberculosis to enable the development of an informed educational program and potential intervention plans.
Methods There were 500 male soldiers serving in the Korean Army who responded to questionnaires regarding knowledge of, attitudes towards, and preventive behavior towards tuberculosis. The questionnaires were collected between September 10 until October 1, 2014. Participants’ characteristic that influenced differences in knowledge, attitudes, and preventive behavior towards tuberculosis were compared by
t test. Variables that influenced preventive behavior were identified by multiple regression analysis.Results The mean scores assessing knowledge of, attitude, and preventive behavior towards tuberculosis were 11.64 (± 4.03) out of 20 points, 3.21 (± 0.38) out of 4 points, and 2.88 (± 0.42) out of 4 points, respectively. Non-smokers were more knowledgeable about tuberculosis than smokers. Participants who had family or friends with tuberculosis had better knowledge and a more productive attitude to tuberculosis. Participants who were educated or obtained information about tuberculosis, received better scores in all areas of knowledge, attitude and preventive behavior compared to other participants. Non-smoking, family or friends who have had tuberculosis, obtaining information about tuberculosis, and positive attitudes towards treatment and preventive education had an explanatory power of 24.6% with regard to preventive behavior against tuberculosis.
Conclusion More relatable, systemized education should be provided regularly to improve soldiers’ knowledge of, attitudes towards, and prevention against tuberculosis in the Republic of Korea Army.
-
Citations
Citations to this article as recorded by- Tingkat Pengetahuan Keluarga Tinggal Serumah Tentang Pencegahan Penularan Pasien Tuberkulosis Paru
Komang Yuliani, I Dewa Agung Ketut Sudarsana
Journal Nursing Research Publication Media (NURSEP.2023; 2(1): 47. CrossRef - Knowledge, Attitudes, and Preventative Behavior Toward Tuberculosis in University Students in Indonesia
Irma Melyani Puspitasari, Rano Kurnia Sinuraya, Arini Nurhaqiqi Aminudin, Rika Rahmi Kamilah
Infection and Drug Resistance.2022; Volume 15: 4721. CrossRef - The Relationship between Health Literacy and Preventive Behaviors of Soldiers
Javad Azimzadeh, Maryam Nezamzadeh, Fatemeh Kalroozi, Seyyed Amir Hossein Pishgooie
Military Caring Sciences.2021; 8(2): 109. CrossRef - Factors Affecting Preventive Behavior related to Tuberculosis among University Students in Korea: Focused on Knowledge, Attitude and Optimistic Bias related to Tuberculosis
Myung Soon Kwon, Yun Choi
Journal of Korean Academy of Fundamentals of Nursi.2020; 27(3): 236. CrossRef - Assessment of knowledge, attitude and practice on tuberculosis among teacher trainees of Samtse College of Education, Bhutan
Thinley Dorji, Tandin Tshering, Kinley Wangdi, Ritesh G. Menezes
PLOS ONE.2020; 15(11): e0241923. CrossRef - The Infectivity of Pulmonary Tuberculosis in Korean Army Units: Evidence from Outbreak Investigations
Chang-gyo Yoon, Dong Yoon Kang, Jaehun Jung, Soo Yon Oh, Jin Beom Lee, Mi-Hyun Kim, Younsuk Seo, Hee-Jin Kim
Tuberculosis and Respiratory Diseases.2019; 82(4): 298. CrossRef
- Tingkat Pengetahuan Keluarga Tinggal Serumah Tentang Pencegahan Penularan Pasien Tuberkulosis Paru
- Cost of Tuberculosis Treatment: Evidence from Iran’s Health System
- Vahid Bay, Payam Tabarsi, Aziz Rezapour, Sima Marzban, Ehsan Zarei
- Osong Public Health Res Perspect. 2017;8(5):351-357. Published online October 31, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.5.09
- 4,686 View
- 40 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives This study aimed to estimate the cost of smear-positive drug-susceptible pulmonary tuberculosis (TB) treatment of the patients in the Azadshahr district, Golestan Province, Iran.
Methods In this retrospective study, all new smear positive pulmonary TB patients who had been registered at the district’s health network between April, 2013 and December, 2015 and had successfully completed their treatment were entered into the study (45 patients). Treatment costs were estimated from the provider’s perspective using an activity-based costing (ABC) method.
Results The cost of treating a new smear-positive pulmonary TB patient was US dollar (USD) 1,409.00 (Iranian Rial, 39,438,260), which can be divided into direct and indirect costs (USD 1,226.00 [87%] and USD 183.00 [13%], respectively). The highest cost (58.1%) was related to care and management of TB patients (including 46.1% human resources costs and 12% directly-observed treatment, short course implementation) and then respectively related to hospitalization (12.1%), supportive activity centers (11.4%), transportation (6.5%), medicines (5.3%), and laboratory tests and radiography (3.2%).
Conclusion Using disease-specific cost studies can help the healthcare system management to have correct insight into the financial burden created by the disease. This can subsequently be used in prioritization, planning, operational budgeting, economic evaluation of programs, interventions, and ultimately in disease management.
-
Citations
Citations to this article as recorded by- Costs of services and funding gap of the Bangladesh National Tuberculosis Control Programme 2016–2022: An ingredient based approach
Md. Zahid Hasan, Sayem Ahmed, Zeenat Islam, Farzana Dorin, Md. Golam Rabbani, Gazi Golam Mehdi, Mohammad Wahid Ahmed, Tazeen Tahsina, Shehrin Shaila Mahmood, Ziaul Islam, Kevin Schwartzman
PLOS ONE.2023; 18(6): e0286560. CrossRef - Distribution incidence, mortality of tuberculosis and human development index in Iran: estimates from the global burden of disease study 2019
Hossien Fallahzadeh, Zaher Khazaei, Moslem Lari Najafi, Sajjad Rahimi Pordanjani, Elham Goodarzi
BMC Public Health.2023;[Epub] CrossRef - Spatio-temporal epidemiology of the tuberculosis incidence rate in Iran 2008 to 2018
Behzad Kiani, Amene Raouf Rahmati, Robert Bergquist, Soheil Hashtarkhani, Neda Firouraghi, Nasser Bagheri, Elham Moghaddas, Alireza Mohammadi
BMC Public Health.2021;[Epub] CrossRef - An Analysis of the Survival Probability of Tuberculosis Patients with Right Censored and Interval Censored Observation in Zahedan during 2014 - 2016
Mohammad Hossein Dehghan, Seyyed Mohammad Hashemi Shahri, Mojgan Salari
Zahedan Journal of Research in Medical Sciences.2019;[Epub] CrossRef - Extent and determinants of catastrophic health expenditure for tuberculosis care in Chongqing municipality, China: a cross-sectional study
Weixia Duan, Wen Zhang, Chengguo Wu, Qingya Wang, Ya Yu, Hui Lin, Ying Liu, Daiyu Hu
BMJ Open.2019; 9(4): e026638. CrossRef - Demographic, socio-economic and behavior as risk factors of tuberculosis in Malaysia: a systematic review of the literature
Nur Adibah Mohidem, Zailina Hashim, Malina Osman, Rafiza Shaharudin, Farrah Melissa Muharam, Punitha Makeswaran
Reviews on Environmental Health.2018; 33(4): 407. CrossRef
- Costs of services and funding gap of the Bangladesh National Tuberculosis Control Programme 2016–2022: An ingredient based approach
- Low Levels of Extensively Drug-resistant Tuberculosis among Multidrug Resistant Tuberculosis Isolates and Their Relationship to Risk Factors: Surveillance in Tehran, Iran; 2006 to 2014
- Alireza Hadizadeh Tasbiti, Shamsi Yari, Mostafa Ghanei, Mohammad Ali Shokrgozar, Abolfazl Fateh, Ahmadreza Bahrmand
- Osong Public Health Res Perspect. 2017;8(2):116-123. Published online April 30, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.2.03
- 3,676 View
- 27 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives Extensively drug-resistant tuberculosis (XDR-TB) is more expensive and difficult to treat than multidrug-resistant tuberculosis (MDR-TB), and outcomes for patients are much worse; therefore, it is important that clinicians understand the magnitude and distribution of XDR-TB. We conducted a retrospective study to compare the estimated incidence of and risk factors for M/XDR-TB with those of susceptible TB controls.
Methods Sputum culture and drug susceptibility testing (DST) were performed in patients with known or suspected TB. Strains that were identified as MDR were subjected to DST for second-line drugs using the proportion method.
Results Among 1,442 TB patients (mean age, 46.48 ± 21.24 years) who were culture-positive for
Mycobacterium tuberculosis , 1,126 (78.1%) yielded isolates that were resistant to at least one first-line drug; there were 33 isolates (2.3%) of MDR-TB, of which three (0.2%) were classified as XDR-TB. Ofloxacin resistance was found in 10 (0.7%) isolates. Women were 15% more likely than men to yield M/XDR-TB isolates, but this difference was not significant. In a multivariate analysis comparing susceptible TB with X/MDR-TB, only one variable—the number of previous treatment regimens—was associated with MDR (odds ratio, 1.06; 95% confidence interval, 1.14–21.2).Conclusion The burden of M/XDR-TB cases is not sizeable in Iran. Nonetheless, strategies must be implemented to identify and cure patients with pre-XDR-TB before they develop XDR-TB. Our results provide a greater understanding of the evolution and spread of M/XDR-TB in an environment where drug-resistant TB has a low incidence.
-
Citations
Citations to this article as recorded by- Global prevalence of drug-resistant tuberculosis: a systematic review and meta-analysis
Nader Salari, Amir Hossein Kanjoori, Amin Hosseinian-Far, Razie Hasheminezhad, Kamran Mansouri, Masoud Mohammadi
Infectious Diseases of Poverty.2023;[Epub] CrossRef - Pre-extensively drug-resistant tuberculosis among pulmonary multidrug-resistant tuberculosis patients in Eastern Nigeria
Ndubuisi O. Nwachukwu, Amara E. Ulasi, Christopher U. Okoronkwo, Valentine N. Unegbu
Lung India.2023; 40(6): 492. CrossRef - Mycobacterium tuberculosis PPE7 Enhances Intracellular Survival of Mycobacterium smegmatis and Manipulates Host Cell Cytokine Secretion Through Nuclear Factor Kappa B and Mitogen-Activated Protein Kinase Signaling
Jing Suo, Xinyan Wang, Rongchuan Zhao, Pengjiao Ma, Liang Ge, Tao Luo
Journal of Interferon & Cytokine Research.2022; 42(10): 525. CrossRef - The burden of pre-extensively and extensively drug-resistant tuberculosis among MDR-TB patients in the Amhara region, Ethiopia
Agumas Shibabaw, Baye Gelaw, Wondwossen Gebreyes, Richard Robinson, Shu-Hua Wang, Belay Tessema, Shampa Anupurba
PLOS ONE.2020; 15(2): e0229040. CrossRef Spoligotype and Drug Susceptibility Profiles of Mycobacterium tuberculosis Complex Isolates in Golestan Province, North Iran
Noormohamad Mansoori, Farzam Vaziri, Sirus Amini, Sharareh Khanipour, Shahin Pourazar Dizaji, Masoumeh Douraghi
Infection and Drug Resistance.2020; Volume 13: 2073. CrossRef- A comparative study of phenotypic and genotypic first- and second-line drug resistance testing of Mycobacterium tuberculosis
Fatemeh Sakhaee, Morteza Ghazanfari, Nayereh Ebrahimzadeh, Farzam Vaziri, Fatemeh Rahimi Jamnani, Mehdi Davari, Safoora Gharibzadeh, Fatemeh Hemati Mandjin, Abolfazl Fateh, Seyed Davar Siadat
Biologicals.2017; 49: 33. CrossRef
- Global prevalence of drug-resistant tuberculosis: a systematic review and meta-analysis
- Tuberculosis Notification Completeness and Timeliness in the Republic of Korea During 2012–2014
- Hae-Young Kang, Hyosoon Yoo, Wonseo Park, Unyeong Go, Eunkyeong Jeong, Ki-Suck Jung, Hyunjin Son
- Osong Public Health Res Perspect. 2016;7(5):320-326. Published online October 31, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.08.002
- 3,940 View
- 27 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Completeness and timeliness are key attributes of accurate disease surveillance. This study aimed to evaluate the completeness and timeliness of tuberculosis (TB) notification in the Republic of Korea, by comparing notification data from the Korean National Tuberculosis Surveillance System and reimbursement data from the National Health Insurance.
Methods
We evaluated reimbursement data from 103,075 cases (2012–2014) and surveillance data from 215,055 cases (2011–2015); cases were matched using Resident Registration Numbers. Completeness was evaluated using notifications that were reported within 365 days of the corresponding insurance claim. Timeliness was evaluated using the delay between starting TB treatment and the corresponding notification. Multivariate logistic regression analysis was used to analyze factors that affected completeness (e.g., sex, age, institution type, and nationality).
Results
The completeness values were 90.0% in 2012 (33,094/36,775), 93.0% in 2013 (31,445/33,803), and 94.0% in 2014 (30,537/32,497). The rates of notification within 7 days of the corresponding claim were 81.6% in 2012 (27,323/33,489), 79.8% in 2013 (25,469/31,905), and 80.4% in 2014 (24,891/30,978). Increases over time were observed in the sex-, age-, institution type-, and nationality-specific analyses. Multivariate analyses revealed that completeness was affected by institution type [hospitals: odds ratio (OR) = 1.82, p < 0.001; general hospitals: OR = 4.18, p < 0.001] and nationality (native Korean status: OR = 1.48, p < 0.001).
Conclusion
Notification completeness exhibited a 4.0% increase during 2012–2014 in Korea, and institution type and nationality significantly affected the completeness of TB notifications. -
Citations
Citations to this article as recorded by- Nationwide Treatment Outcomes of Patients With Multidrug/Rifampin-Resistant Tuberculosis in Korea, 2011–2017: A Retrospective Cohort Study (Korean TB-POST)
Hongjo Choi, Jeongha Mok, Young Ae Kang, Dawoon Jeong, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Doosoo Jeon
Journal of Korean Medical Science.2023;[Epub] CrossRef - Retreatment after loss to follow-up reduces mortality in patients with multidrug/rifampicin-resistant tuberculosis
Hongjo Choi, Jeongha Mok, Young Ae Kang, Dawoon Jeong, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Doosoo Jeon
ERJ Open Research.2023; 9(4): 00135-2023. CrossRef - Cohort Profile: Korean Tuberculosis and Post-Tuberculosis Cohort Constructed by Linking the Korean National Tuberculosis Surveillance System and National Health Information Database
Dawoon Jeong, Hee-Yeon Kang, Jinsun Kim, Hyewon Lee, Bit-Na Yoo, Hee-Sun Kim, Hongjo Choi
Journal of Preventive Medicine and Public Health.2022; 55(3): 253. CrossRef - Hidden loss to follow-up among tuberculosis patients managed by public–private mix institutions in South Korea
Hyung Woo Kim, Sohee Park, Jinsoo Min, Jiyu Sun, Ah Young Shin, Jick Hwan Ha, Jae Seuk Park, Sung-Soon Lee, Marc Lipman, Ibrahim Abubakar, Helen R. Stagg, Ju Sang Kim
Scientific Reports.2022;[Epub] CrossRef - Assessing the Quality of Reporting to China’s National TB Surveillance Systems
Tao Li, Lijia Yang, Sarah E. Smith-Jeffcoat, Alice Wang, Hui Guo, Wei Chen, Xin Du, Hui Zhang
International Journal of Environmental Research an.2021; 18(5): 2264. CrossRef - Quality and Utility of Information Captured by Surveillance Systems Relevant to Antimicrobial Resistance (AMR): A Systematic Review
Mustafa Al-Haboubi, Rebecca E. Glover, Elizabeth Eastmure, Mark Petticrew, Nick Black, Nicholas Mays
Antibiotics.2021; 10(4): 431. CrossRef - Risk of tuberculosis in patients with cancer treated with immune checkpoint inhibitors: a nationwide observational study
Seongman Bae, Ye-Jee Kim, Min-ju Kim, Jwa Hoon Kim, Sung-Cheol Yun, Jiwon Jung, Min Jae Kim, Yong Pil Chong, Sung-Han Kim, Sang-Ho Choi, Yang Soo Kim, Sang-Oh Lee
Journal for ImmunoTherapy of Cancer.2021; 9(9): e002960. CrossRef - Underreporting of patients diagnosed with tuberculosis in the Region of Southern Denmark
Frederik D. Thrane, Peter H. Andersen, Isik S. Johansen, Inge K. Holden
Scandinavian Journal of Public Health.2020; 48(8): 870. CrossRef - Effects of particulate air pollution on tuberculosis development in seven major cities of Korea from 2010 to 2016: methodological considerations involving long-term exposure and time lag
Honghyok Kim, Sarah Yu, Hongjo Choi
Epidemiology and Health.2020; 42: e2020012. CrossRef - Latent tuberculosis infection screening and treatment in congregate settings (TB FREE COREA): protocol for a prospective observational study in Korea
Jinsoo Min, Hyung Woo Kim, Helen R Stagg, Marc Lipman, Molebogeng X Rangaka, Jun-Pyo Myong, Hyeon Woo Yim, Jeong Uk Lim, Yunhee Lee, Hyeon-Kyoung Koo, Sung-Soon Lee, Jae Seuk Park, Kyung Sook Cho, Ju Sang Kim
BMJ Open.2020; 10(2): e034098. CrossRef - Tuberculosis Surveillance and Monitoring under the National Public-Private Mix Tuberculosis Control Project in South Korea 2016–2017
Jinsoo Min, Hyung Woo Kim, Yousang Ko, Jee Youn Oh, Ji Young Kang, Joosun Lee, Young Joon Park, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2020; 83(3): 218. CrossRef - Prediction of treatment failure and compliance in patients with tuberculosis
Hyeon-Kyoung Koo, Jinsoo Min, Hyung Woo Kim, Joosun Lee, Ju Sang Kim, Jae Seuk Park, Sung-Soon Lee
BMC Infectious Diseases.2020;[Epub] CrossRef - Impact of COVID-19 Pandemic on the National PPM Tuberculosis Control Project in Korea: the Korean PPM Monitoring Database between July 2019 and June 2020
Jinsoo Min, Hyung Woo Kim, Hyeon-Kyoung Koo, Yousang Ko, Jee Youn Oh, Jaetae Kim, Jiyeon Yang, Yunhyung Kwon, Young-Joon Park, Ji Young Kang, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Journal of Korean Medical Science.2020;[Epub] CrossRef - Clinical profiles of early and tuberculosis-related mortality in South Korea between 2015 and 2017: a cross-sectional study
Jinsoo Min, Ju Sang Kim, Hyung Woo Kim, Ah Young Shin, Hyeon-Kyoung Koo, Sung-Soon Lee, Yang-Ki Kim, Kyeong-Cheol Shin, Jung Hyun Chang, Gayoung Chun, Joosun Lee, Mi Sun Park, Jae Seuk Park
BMC Infectious Diseases.2019;[Epub] CrossRef - Treatment outcomes and factors affecting treatment outcomes of new patients with tuberculosis in Busan, South Korea: a retrospective study of a citywide registry, 2014–2015
Jeongha Mok, Daeseong An, Seoungjin Kim, Miyoung Lee, Changhoon Kim, Hyunjin Son
BMC Infectious Diseases.2018;[Epub] CrossRef - Tuberculosis prevention and care in Korea: Evolution of policy and practice
Unyeong Go, Misun Park, Un-Na Kim, Sodam Lee, Sunmi Han, Joosun Lee, Jiyeon Yang, Jieun Kim, Shinyoung Park, Youngman Kim, Hyosoon Yoo, Jeongok Cha, Wonseo Park, Haeyoung Kang, Hwon Kim, Guri Park, Minjung Kim, Ok Park, Hyunjin Son, Enhi Cho, Kyoungin Na,
Journal of Clinical Tuberculosis and Other Mycobac.2018; 11: 28. CrossRef - The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 korean community health survey of 156,747 participants
JooYeon Seo, BoYoul Choi, Shinah Kim, HyeYoung Lee, DongHoon Oh
BMC Public Health.2017;[Epub] CrossRef - Vitamin D Deficiency among Adults with History of Pulmonary Tuberculosis in Korea Based on a Nationwide Survey
Mi Joo, Mi Han, Sun Park, Hwan Shin
International Journal of Environmental Research an.2017; 14(4): 399. CrossRef - Tuberculosis Control in the Republic of Korea
Cho, Kyung Sook
Health and Social Welfare Review.2017; 37(4): 179. CrossRef
- Nationwide Treatment Outcomes of Patients With Multidrug/Rifampin-Resistant Tuberculosis in Korea, 2011–2017: A Retrospective Cohort Study (Korean TB-POST)
- Rapid Detection of Rifampicin- and Isoniazid-Resistant
Mycobacterium tuberculosis using TaqMan Allelic Discrimination - Davood Darban-Sarokhalil, Mohammad J. Nasiri, Abbas A.I. Fooladi, Parvin Heidarieh, Mohammad M. Feizabadi
- Osong Public Health Res Perspect. 2016;7(2):127-130. Published online April 30, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.01.003
- 3,068 View
- 18 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Multidrug-resistant tuberculosis (MDR-TB) is a global problem that many countries are challenged with. Rapid and accurate detection of MDR-TB is critical for appropriate treatment and controlling of TB. The aim of the present study was to evaluate the TaqMan allelic discrimination without minor groove binder (MGB) as a rapid, efficient, and low-cost method for detection of drug resistant strains of Mycobacterium tuberculosis.
Methods
A total of 112 M. tuberculosis isolates from cases with diagnosed TB were subjected to drug susceptibility testing (DST), using the proportion method. Resistant isolates were tested for characterization of mutations in the rpoB and KatG genes by TaqMan genotyping.
Results
Of 112 M. tuberculosis isolates for which DST was performed, three, one, and two isolates were MDR, rifampin (RIF) resistant, and isoniazid (INH) resistant, respectively. According to the threshold cycle (Ct) and curve pattern of mutants, TaqMan probes detect all of the mutations in the analyzed genes (katG 315, AGC→ACC, rpoB 531, TCG→TTG, and rpoB 531, TCG→TGG).
Conclusion
The present study suggests that drug-resistant strains of M. tuberculosis can be detected by pattern’s curve or Ct with TaqMan probes without MGB in real-time polymerase chain reaction (PCR). -
Citations
Citations to this article as recorded by- Drug resistance and the genotypic characteristics of rpoB and katG in rifampicin- and/or isoniazid-resistant Mycobacterium tuberculosis isolates in central Vietnam
Thi Binh Nguyen Nguyen, Thi Kieu Diem Nguyen, Van Hue Trương, Thi Tuyet Ngoc Tran, van Bao Thang Phan, Thi Tuyen Nguyen, Hoang Bach Nguyen, Viet Quynh Tram Ngo, Van Tuan Mai, Paola Molicotti
Osong Public Health and Research Perspectives.2023; 14(5): 347. CrossRef - The Value of the inhA Mutation Detection in Predicting Ethionamide Resistance Using Melting Curve Technology
Yanhua Song, Guirong Wang, Qiang Li, Rongmei Liu, Liping Ma, Qi Li, Mengqiu Gao
Infection and Drug Resistance.2021; Volume 14: 329. CrossRef
- Drug resistance and the genotypic characteristics of rpoB and katG in rifampicin- and/or isoniazid-resistant Mycobacterium tuberculosis isolates in central Vietnam
- Trends and Characteristics of HIV Infection among Suspected Tuberculosis Cases in Public Health Centers in Korea: 2001–2013
- Meekyung Kee, Kyoung-Ho Lee, Sae-Young Lee, Chun Kang, Chaeshin Chu
- Osong Public Health Res Perspect. 2014;5(Suppl):S37-S42. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.11.002
- 2,867 View
- 18 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The Republic of Korea reports approximately 35,000 new tuberculosis (TB) patients each year, and the number of HIV-infected individuals is steadily increasing. Public health centers (PHCs) conduct TB diagnosis and treatment for risk groups in communities. This study aimed to identify possible trends and characteristics of HIV infection among suspected TB cases in PHCs.
Methods
Study subjects were suspected TB cases in PHCs who agreed to be tested for HIV from 2001 to 2013. Trends in HIV seroprevalence were assessed through a series of annual cross-sectional analyses. We analyzed suspected TB cases, and HIV-infected individuals among suspected TB cases, by gender, age, nationality, and region.
Results
The number of suspected tuberculosis cases who took an HIV test in PHCs was approximately 6,000 each year from 2001 to 2013. Among the suspected TB cases who took an HIV test, the number of those aged 20–39 is gradually decreasing, while the number of those aged 50–69 is increasing. During this period, 32 HIV-infected individuals were identified; the majority were men (94%), aged 30–49 (68%), Korean (94%), and residents in a metropolitan area (53%). HIV seroprevalence decreased from 8.2 per 10,000 persons in 2001 to 1.9 per 10,000 persons in 2013.
Conclusion
This study has identified trends and characteristics of HIV infection among suspected tuberculosis cases in PHCs. This national data provides a basis for public health policy for HIV and tuberculosis infections. -
Citations
Citations to this article as recorded by- Is Tuberculosis Still the Number One Infectious Disease in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5: S1. CrossRef
- Is Tuberculosis Still the Number One Infectious Disease in Korea?
- A Study on the Relapse Rate of Tuberculosis and Related Factors in Korea Using Nationwide Tuberculosis Notification Data
- Hyungmin Lee, Jusang Kim
- Osong Public Health Res Perspect. 2014;5(Suppl):S8-S17. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.11.001
- 2,872 View
- 22 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
From the perspective of public health, tuberculosis (TB) remains an important issue that threatens health. Korea is an intermediate burden country with a TB incidence of 97/100,000 individuals. Among many TB control measures, a relapse rate of TB is one indicator that can be used to indirectly assess the level of TB control in countries and in communities. Relapse TB has an approximately 12% yearly incidence in Korea. This study aims to estimate the relapse rate of TB and to investigate the associated factors by using nationwide TB notification data in Korea.
Methods
The nationwide TB notification data in 2005 was used with the exclusion criteria of duplicated reporting, foreign-born patients, outcome–died, and outcome–diagnosis changed. The data were double-checked as to whether they were reported again during 2006–2010 and the estimated relapse rate of TB. Associated factors were analyzed by multivariate logistic regression with the variables of age, sex, registration type, results of sputum smear test, medication, and outcome of treatment.
Results
Among 45,434 TB patients in 2005, 4,371 patients were again reported as TB patients from 2006 to 2010. Five hundred and sixty-four patients were reported more than twice and the cumulative number of relapses was 5,072 cases. The 5-year relapse rate was estimated as 9.62%. The relapse rate decreased yearly: 4.8% in 2006, 2.4% in 2007, 1.6% in 2008, 1.4% in 2009, and 1.0% in 2010. Age, sex, registration type, tuberculosis type, and medication were independently associated with a relapse of TB. In the multivariate logistic regression analysis, the following factors were related: male sex, 40–49 years old; registration type, relapse, treatment after failure, treatment after default, transfer in, and other, the sputum smear-positive pulmonary TB, and medications (including individuals taking 2–5 drugs).
Conclusion
This study has estimated a 5-year relapse rate of TB in Korea that is slightly lower than the rate of relapse TB in the annual reports. This study could be conducted and cross-checked with data from the National Health Insurance in the future. -
Citations
Citations to this article as recorded by- Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - Recurrence of pulmonary tuberculosis in India: Findings from the 2019–2021 nationwide community-based TB prevalence survey
Prathiksha Giridharan, Sriram Selvaraju, Raghuram Rao, Kiran Rade, Kannan Thiruvengadam, Smita Asthana, Rakesh Balachandar, Sampada Dipak Bangar, Avi Kumar Bansal, Jyothi Bhat, Debjit Chakraborty, Vishal Chopra, Dasarathi Das, Shanta Dutta, Kangjam Rekha
PLOS ONE.2023; 18(12): e0294254. CrossRef - Risk factors associated with tuberculosis recurrence in South Korea determined using a nationwide cohort study
Hin Moi Youn, Moon-Kyung Shin, Dawoon Jeong, Hee-Jin Kim, Hongjo Choi, Young Ae Kang, Jun Hyeok Lim
PLOS ONE.2022; 17(6): e0268290. CrossRef - Facteurs de risque de récurrence de tuberculose pulmonaire bactériologique confirmé à Kisangani (République démocratique du Congo)
Catherine Marie Nomopuane Kabudri, Shadrack Kandala Ngianga II, Léon Okenge Ngongo
Santé Publique.2022; Vol. 34(4): 591. CrossRef - Predicting the impact of control strategies on the tuberculosis burden in South and North Korea using a mathematical model
Hyunwoo Cho, Youngmok Park, Jeongjoo Seok, Joon Sup Yeom, Jun Yong Choi, Hee Jin Kim, Young Ae Kang, Jeehyun Lee
BMJ Global Health.2021; 6(10): e005953. CrossRef - Preferred product characteristics for therapeutic vaccines to improve tuberculosis treatment outcomes: Key considerations from World Health Organization consultations
Johan Vekemans, Michael James Brennan, Mark Hatherill, Lewis Schrager, Bernard Fritzell, Kathryn Rutkowski, Beatrice De Vos, Matteo Zignol, Georges Thiry, Ann M. Ginsberg, Barry Walker
Vaccine.2020; 38(2): 135. CrossRef - Rate and risk factors of recurrent tuberculosis in Yemen: a 5-year prospective study
Mohammed Saif Anaam, Alian A. Alrasheedy, Saud Alsahali, Saeed O. Alfadly, Adel H. Aldhubhani
Infectious Diseases.2020; 52(3): 161. CrossRef - Small Animal Model of Post-chemotherapy Tuberculosis Relapse in the Setting of HIV Co-infection
Matthew B. Huante, Tais B. Saito, Rebecca J. Nusbaum, Kubra F. Naqvi, Sadhana Chauhan, Robert L. Hunter, Jeffrey K. Actor, Jai S. Rudra, Mark A. Endsley, Joshua G. Lisinicchia, Benjamin B. Gelman, Janice J. Endsley
Frontiers in Cellular and Infection Microbiology.2020;[Epub] CrossRef - Proteomic analysis of infected primary human leucocytes revealed PSTK as potential treatment-monitoring marker for active and latent tuberculosis
Benjawan Kaewseekhao, Sittiruk Roytrakul, Yodying Yingchutrakul, Kanin Salao, Wipa Reechaipichitkul, Kiatichai Faksri, HASNAIN SEYED EHTESHAM
PLOS ONE.2020; 15(4): e0231834. CrossRef - The association between proton pump inhibitor use and the risk of tuberculosis: A case‐control study
Hyun Jin Song, Haesuk Park, Susan Park, Jin‐Won Kwon
Pharmacoepidemiology and Drug Safety.2019; 28(6): 830. CrossRef - Recurrence of tuberculosis in a low-incidence setting: a retrospective cross-sectional study augmented by whole genome sequencing
Laila Parvaresh, Taryn Crighton, Elena Martinez, Andrea Bustamante, Sharon Chen, Vitali Sintchenko
BMC Infectious Diseases.2018;[Epub] CrossRef - Treatment Outcomes of Patients Treated for Pulmonary Tuberculosis after Undergoing Gastrectomy
In Young Jung, Moo Hyun Kim, Woo Yong Jeong, Mi Young Ahn, Yong Duk Jeon, Hea Won Ahn, Jin Young Ahn, Je Eun Song, Dong Hyun Oh, Yong Chan Kim, Eun Jin Kim, Su Jin Jeong, Nam Su Ku, June Myung Kim, Jun Yong Choi
The Tohoku Journal of Experimental Medicine.2016; 240(4): 281. CrossRef - Is Tuberculosis Still the Number One Infectious Disease in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5: S1. CrossRef
- Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
- Results of Tuberculosis Contact Investigation in Congregate Settings in Korea, 2013
- Yunhyung Kwon, So Jung Kim, Jieun Kim, Seol-yi Kim, Eun Mi Song, Eun Jung Lee, Yun Choi, Yejin Kim, Byoung ok Lim, Da Sul Kim, Duksun Choi, Hye Sung Kim, Ji Eun Park, Ji-eun Yun, Jin A. Park, Jong Rak Jung, Joo-kyoung Kim, Sang Hee Kang, Seo Yean Hong, Seung Jae Lee, Soo Jin Park, Sun Hwa Park, Sunhye Yoon, Yoonsun Kim, Yunjeong Choi, Yun Jeong Seo, Yul A Seo, Jiseon Park, Minhee Sung, Minjang Shin, Hyunjin Son, Yeonkyeng Lee, Unyeong Go, Geun-Yong Kwon
- Osong Public Health Res Perspect. 2014;5(Suppl):S30-S36. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.10.010
- 3,368 View
- 22 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aimed to check the status of the contact investigation in congregate settings to eradicate tuberculosis (TB) in the Republic of Korea.
Methods
The “Integrated System for Disease and Public Health Management” is used for care and follow-up for patients and contacts of TB. We downloaded data for contact investigations conducted from January to December 2013.
Results
A total of 1,200 contact investigations in congregate settings were carried out by 25 field investigators in 2013. We performed the status of contact investigation, TB, and LTBI rate by age, accept rate of LTBI treatment, and complete rate of LTBI treatment during 2013. A total of 1,547 index TB patients, 149,166 contacts, and 259 additional TB patients were found through the investigation. Kindergartens showed the highest LTBI rate, 19.8%, among educational facilities. The second highest was in elementary schools and the subtotal LTBI rate of educational facilities was 7.8%. Social welfare/correctional facilities and workplaces showed relatively high LTBI rates of 23.8% and 23.6%, respectively. By age, individuals >35 years showed the highest LTBI rate, followed by those aged 0–4 years, 30–34 years, and 5–9 years, with rates of 18.1%, 16.4%, and 15.4% respectively. When comparing the tuberculin skin test (TST) positive conversion ratio by facility, middle school and high school were relatively high compared to the others. The accept rate of LTBI treatment in the workplace was lowest at 63% and the complete rate in elementary schools was lowest at 76.5%.
Conclusion
TB contact investigation is considered as a meaningful strategy for preventing TB outbreaks in congregate settings and decreasing the prevalence of TB in young people. Results of this study could be used to establish the LTBI management policy. -
Citations
Citations to this article as recorded by- Latent Tuberculosis Cascade of Care Among Healthcare Workers: A Nationwide Cohort Analysis in Korea Between 2017 and 2018
Jinsoo Min, Hyung Woo Kim, Joon Young Choi, Ah Young Shin, Ji Young Kang, Yunhee Lee, Jun-Pyo Myong, Hyunsuk Jeong, Sanghyuk Bae, Hyeon-Kyoung Koo, Sung-Soon Lee, Jae Seuk Park, Hyeon Woo Yim, Ju Sang Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Risk of active tuberculosis development in contacts exposed to infectious tuberculosis in congregate settings in Korea
Shin Young Park, Sunmi Han, Young-Man Kim, Jieun Kim, Sodam Lee, Jiyeon Yang, Un-Na Kim, Mi-sun Park
Scientific Reports.2020;[Epub] CrossRef - The risk of active tuberculosis among individuals living in tuberculosis-affected households in the Republic of Korea, 2015
Jiyeon Yang, Sodam Lee, Suhyeon Oh, Sunmi Han, Shin Young Park, Youngman Kim, Jieun Kim, Mi-sun Park, Philip C. Hill
PLOS ONE.2019; 14(12): e0225744. CrossRef - The Infectivity of Pulmonary Tuberculosis in Korean Army Units: Evidence from Outbreak Investigations
Chang-gyo Yoon, Dong Yoon Kang, Jaehun Jung, Soo Yon Oh, Jin Beom Lee, Mi-Hyun Kim, Younsuk Seo, Hee-Jin Kim
Tuberculosis and Respiratory Diseases.2019; 82(4): 298. CrossRef - Tuberculosis prevention and care in Korea: Evolution of policy and practice
Unyeong Go, Misun Park, Un-Na Kim, Sodam Lee, Sunmi Han, Joosun Lee, Jiyeon Yang, Jieun Kim, Shinyoung Park, Youngman Kim, Hyosoon Yoo, Jeongok Cha, Wonseo Park, Haeyoung Kang, Hwon Kim, Guri Park, Minjung Kim, Ok Park, Hyunjin Son, Enhi Cho, Kyoungin Na,
Journal of Clinical Tuberculosis and Other Mycobac.2018; 11: 28. CrossRef - The Prevalence and Risk Factors of Latent Tuberculosis Infection among Health Care Workers Working in a Tertiary Hospital in South Korea
Jae Seuk Park
Tuberculosis and Respiratory Diseases.2018; 81(4): 274. CrossRef
- Latent Tuberculosis Cascade of Care Among Healthcare Workers: A Nationwide Cohort Analysis in Korea Between 2017 and 2018
- The Usefulness of the Tuberculosis Skin Test and the Interferon-gamma Release Assay in the Diagnosis of Latent Tuberculosis Infection in South Korea
- Ju Young Jang, In Won Park, Byoung Whui Choi, Jae Chol Choi
- Osong Public Health Res Perspect. 2014;5(Suppl):S18-S23. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.10.009
- 3,115 View
- 22 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
South Koreans receive the bacillus Calmette-Guerin (BCG) vaccination, which influence the result of the tuberculin skin test (TST); however, only a few studies have described the usefulness of the TST and interferon-γ release assay (IGRA) for diagnosing latent TB infection (LTBI). Therefore, our aim was to determine the usefulness of the TST and IGRA for diagnosing LTBI in a household contacts investigation.
Methods
We reviewed the 329 household contacts who visited Chung-Ang University Hospital (Seoul, Korea) from May 1, 2011 to February 28, 2014. To evaluate the effectiveness of TST and IGRA for the diagnosis of LTBI, we examined the concordance rate between the two tests, based on age. We also evaluated the risk factors for LTBI.
Results
The concordance rate between the two tests in individuals 0–24 years, 25–54 years, and over 55 years were 82.6% (κ = 0.64, p < 0.01), 68.9% (κ = 0.40, p < 0.01), and 68.4% (κ = 0.35, p < 0.01), respectively. The ratio of positive TST to negative IGRA was higher in individuals 25–44 years old, whereas the ratio of negative TST to positive IGRA was higher in individuals older than 55 years old. Based on the TST, the risk factor for LTBI was a cavity (p < 0.01). When using IGRA, the risk factors were contact time (p = 0.04) and age over 55 years old (p = 0.02).
Conclusion
The concordance rate between TST and IGRA was not good after the age of 25 years. The IGRA test reflects the known risk factors more exactly. -
Citations
Citations to this article as recorded by- Household tuberculosis contact investigation in a tuberculosis-prevalent country
Jung Seop Eom, Insu Kim, Won-Young Kim, Eun-Jung Jo, Jeongha Mok, Mi-Hyun Kim, Kwangha Lee, Ki Uk Kim, Hye-Kyung Park, Min Ki Lee
Medicine.2018; 97(3): e9681. CrossRef - QuantiFERON-TB Gold In-tube test for the diagnosis of active and latent tuberculosis in selected health facilities of Addis Ababa, Ethiopia
Selam Niguse, Kassu Desta, Gebremdihin Gebremichael, Atsebeha Gebrezgeaxier, Mulluwork Getahun, Desta Kassa
BMC Research Notes.2018;[Epub] CrossRef - Predictors for false-negative QuantiFERON-TB Gold assay results in patients with extrapulmonary tuberculosis
Youn Jeong Kim, Ji Young Kang, Sang Il Kim, Mee Soo Chang, Yang Ree Kim, Yeon Joon Park
BMC Infectious Diseases.2018;[Epub] CrossRef
- Household tuberculosis contact investigation in a tuberculosis-prevalent country
- Activities of the Korean Institute of Tuberculosis
- Sungweon Ryoo, Hee Jin Kim
- Osong Public Health Res Perspect. 2014;5(Suppl):S43-S49. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.10.007
- 2,932 View
- 20 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF - The Korean National Tuberculosis Association (KNTA) set up the Korean Institute of Tuberculosis (KIT) in 1970 to foster research and technical activities pertaining to tuberculosis (TB). The KNTA/KIT had successfully conducted a countrywide TB prevalence survey from 1965 to 1995 at 5-year intervals. The survey results (decline in TB rates) established Korea as a country that had successfully implemented national control programs for TB. The KIT developed the Korea Tuberculosis Surveillance System and the Laboratory Management Information System, both of which were transferred to the Korea Centers for Disease Control and Prevention after its establishment. The KIT functions as a central and supranational reference TB laboratory for microbiological and epidemiological research and provides training and education for health-care workers and medical practitioners. Recently, the KIT has expanded its activities to countries such as Ethiopia, Laos, and Timor-Leste to support TB control and prevention. The KIT will continue to support research activities and provide technical assistance in diagnosing the infection until it is completely eliminated in Korea.
-
Citations
Citations to this article as recorded by- A Review of Recent Advances in Deep Learning Models for Chest Disease Detection Using Radiography
Adnane Ait Nasser, Moulay A. Akhloufi
Diagnostics.2023; 13(1): 159. CrossRef - AI-based radiodiagnosis using chest X-rays: A review
Yasmeena Akhter, Richa Singh, Mayank Vatsa
Frontiers in Big Data.2023;[Epub] CrossRef - Deep Learning for Pneumonia Classification in Chest Radiography Images using Wavelet Transform
Amal Azeroual, Benayad Nsiri, Taoufiq Belhoussine Drissi, Amine El Ammari, Abdessamad Charrafi, Ittimade Nassar, Brahim Benaji
WSEAS TRANSACTIONS ON INFORMATION SCIENCE AND APPL.2023; 20: 245. CrossRef - The response to COVID-19 in Timor-Leste: lessons learnt
Joshua R Francis, Rui Maria de Araujo, Odete da Silva Viegas, Sergio Lobo, Danina Coelho, Arvind Mathur, Vinay Bothra, Dongbao Yu, Anthony D K Draper, Jennifer Yan, Nelson Martins
BMJ Global Health.2023; 8(10): e013573. CrossRef - Review on Pneumonia Image Detection: A Machine Learning Approach
Amer Kareem, Haiming Liu, Paul Sant
Human-Centric Intelligent Systems.2022; 2(1-2): 31. CrossRef - Database and AI Diagnostic Tools Improve Understanding of Lung Damage, Correlation of Pulmonary Disease and Brain Damage in COVID-19
Ilona Karpiel, Ana Starcevic, Mirella Urzeniczok
Sensors.2022; 22(16): 6312. CrossRef - MS-CheXNet: An Explainable and Lightweight Multi-Scale Dilated Network with Depthwise Separable Convolution for Prediction of Pulmonary Abnormalities in Chest Radiographs
Shashank Shetty, Ananthanarayana V S., Ajit Mahale
Mathematics.2022; 10(19): 3646. CrossRef - An incremental learning approach to automatically recognize pulmonary diseases from the multi-vendor chest radiographs
Mehreen Sirshar, Taimur Hassan, Muhammad Usman Akram, Shoab Ahmed Khan
Computers in Biology and Medicine.2021; 134: 104435. CrossRef - Deep learning applied to automatic disease detection using chest X‐rays
Daniel A. Moses
Journal of Medical Imaging and Radiation Oncology.2021; 65(5): 498. CrossRef - Intelligent Pneumonia Identification From Chest X-Rays: A Systematic Literature Review
Wasif Khan, Nazar Zaki, Luqman Ali
IEEE Access.2021; 9: 51747. CrossRef - Incidence rate of active tuberculosis in solid organ transplant recipients: Data from a nationwide population cohort in a high‐endemic country
Da Eun Kwon, Sang Hoon Han, Kyung Do Han, Yeonju La, Kyoung Hwa Lee
Transplant Infectious Disease.2021;[Epub] CrossRef - Deep learning, reusable and problem-based architectures for detection of consolidation on chest X-ray images
Hamed Behzadi-khormouji, Habib Rostami, Sana Salehi, Touba Derakhshande-Rishehri, Marzieh Masoumi, Siavash Salemi, Ahmad Keshavarz, Ali Gholamrezanezhad, Majid Assadi, Ali Batouli
Computer Methods and Programs in Biomedicine.2020; 185: 105162. CrossRef - Deep learning applications in pulmonary medical imaging: recent updates and insights on COVID-19
Hanan Farhat, George E. Sakr, Rima Kilany
Machine Vision and Applications.2020;[Epub] CrossRef - PadChest: A large chest x-ray image dataset with multi-label annotated reports
Aurelia Bustos, Antonio Pertusa, Jose-Maria Salinas, Maria de la Iglesia-Vayá
Medical Image Analysis.2020; 66: 101797. CrossRef - Utilizing Knowledge Distillation in Deep Learning for Classification of Chest X-Ray Abnormalities
Thi Kieu Khanh Ho, Jeonghwan Gwak
IEEE Access.2020; 8: 160749. CrossRef - Computer-aided detection in chest radiography based on artificial intelligence: a survey
Chunli Qin, Demin Yao, Yonghong Shi, Zhijian Song
BioMedical Engineering OnLine.2018;[Epub] CrossRef - The Relationship between Illness Perception and Health Behaviors among Patients with Tuberculosis: Mediating Effects of Self-efficacy and Family Support
Hye-jin Kim, Myung Kyung Lee
Korean Journal of Adult Nursing.2017; 29(6): 626. CrossRef - Is Tuberculosis Still the Number One Infectious Disease in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5: S1. CrossRef
- A Review of Recent Advances in Deep Learning Models for Chest Disease Detection Using Radiography
- Evaluation and Comparison of Molecular and Conventional Diagnostic Tests for Detecting Tuberculosis in Korea, 2013
- Sang-Hee Park, Chang-Ki Kim, Hye-Ran Jeong, Hyunjin Son, Seong-Han Kim, Mi-Sun Park
- Osong Public Health Res Perspect. 2014;5(Suppl):S3-S7. Published online December 31, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.10.006
- 2,891 View
- 20 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
A fast and accurate diagnosis is necessary to control and eliminate tuberculosis (TB). In Korea, TB continues to be a serious public health problem. In this study, diagnostic tests on clinical samples from patients suspected to have TB were performed and the sensitivity and specificity of the various techniques were compared. The main objective of the study was to compare various diagnostic tests and evaluate their sensitivity and specificity for detecting tuberculosis.
Methods
From January 2013 to December 2013, 170,240 clinical samples from patients suspected to have TB were tested with smear microscopy, acid-fast bacilli culture, and real-time polymerase chain reaction (PCR). The test results were compared and data were analyzed.
Results
A total of 8216 cultures tested positive for TB (positive detection rate, 4.8%). The contamination rate in the culture was 0.6% and the isolation rate of nontuberculous mycobacteria was 1.0%. The sensitivity and specificity of smear microscopy were 56.8% and 99.6%, respectively. The concordance rate between the solid and liquid cultures was 92.8%. Mycobacterium isolates were not detected in 0.4% of the cases in the liquid culture, whereas no Mycobacterium isolates were detected in 6.8% of the cases in the solid culture. The sensitivity and specificity of real-time PCR for the solid culture were 97.2% and 72.4%, respectively, whereas the corresponding data for the liquid culture were 93.5% and 97.2%.
Conclusion
The study results can be used to improve existing TB diagnosis procedure as well as for comparing the effectiveness of the assay tests used for detecting Mycobacterium tuberculosis isolates. -
Citations
Citations to this article as recorded by- The Xpert® MTB/RIF diagnostic test for pulmonary and extrapulmonary tuberculosis in immunocompetent and immunocompromised patients: Benefits and experiences over 2 years in different clinical contexts
Ana Paula de Oliveira Tomaz, Sonia Mara Raboni, Gislene Maria Botão Kussen, Keite da Silva Nogueira, Clea Elisa Lopes Ribeiro, Libera Maria Dalla Costa, Padmapriya P. Banada
PLOS ONE.2021; 16(3): e0247185. CrossRef - Comparative performance of the laboratory assays used by a Diagnostic Laboratory Hub for opportunistic infections in people living with HIV
Narda Medina, Ana Alastruey-Izquierdo, Danicela Mercado, Oscar Bonilla, Juan C. Pérez, Luis Aguirre, Blanca Samayoa, Eduardo Arathoon, David W. Denning, Juan Luis Rodriguez-Tudela
AIDS.2020; 34(11): 1625. CrossRef - Multiplex PCR is a Rapid, Simple and Cheap Method for Direct Diagnosis of M. tuberculosis from Sputum Samples
Tarig M.S. Alnour, Faisel Abuduhier , Mohammed Khatatneh , Fahad Albalawi , Khalid Alfifi , Bernard Silvala
Infectious Disorders - Drug Targets .2020; 20(4): 495. CrossRef - Naked eye detection of the Mycobacterium tuberculosis complex by recombinase polymerase amplification—SYBR green I assays
Nuntita Singpanomchai, Yukihiro Akeda, Kazunori Tomono, Aki Tamaru, Pitak Santanirand, Panan Ratthawongjirakul
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Retropharyngeal SOL: An unusual presentation of a multifaceted entity
Poojan Agarwal, Manju Kaushal, Shruti Dogra, Ankur Gupta, Nishi Sharma
CytoJournal.2018; 15: 12. CrossRef - Rapid Detection of Rifampicin- and Isoniazid-Resistant Mycobacterium tuberculosis using TaqMan Allelic Discrimination
Davood Darban-Sarokhalil, Mohammad J. Nasiri, Abbas A.I. Fooladi, Parvin Heidarieh, Mohammad M. Feizabadi
Osong Public Health and Research Perspectives.2016; 7(2): 127. CrossRef - Port site infection in laparoscopic surgery: A review of its management
Prakash K Sasmal
World Journal of Clinical Cases.2015; 3(10): 864. CrossRef
- The Xpert® MTB/RIF diagnostic test for pulmonary and extrapulmonary tuberculosis in immunocompetent and immunocompromised patients: Benefits and experiences over 2 years in different clinical contexts
- What Does a Mathematical Model Tell About the Impact of Reinfection in Korean Tuberculosis Infection?
- Sara Kim, Seoyun Choe, Junseong Kim, Sanga Nam, Yeon Shin, Sunmi Lee
- Osong Public Health Res Perspect. 2014;5(1):40-45. Published online February 28, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.01.002
- 3,063 View
- 14 Download
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
According to the Korea Centers for Disease Control and Prevention, new active tuberculosis (TB) cases have increased since 2001. Some key factors explain and characterize the transmission dynamics of Korean TB infection, such as a higher ratio of latent individuals and a new reporting system implemented in 2001, among others.
Methods
We propose a mathematical TB model that includes exogenous reinfection to gain a better understanding of the recent trend for TB incidence. We divide the simulation time window into two periods, 1970–2000 and 2001–2012, according to the implementation date of a new TB detection system.
Results
Two sets of parameters, including the transmission rate, the latent period, the recovery rate, and the proportion of exogenous reinfection, are estimated using the least-squares method and calibrated to data on the incidence of active TB.
Conclusion
Among some key parameters in the model, the case finding effort turned out to be the most significant impacting component on the reduction in the active TB cases. -
Citations
Citations to this article as recorded by- Analysis of the different interventions scenario for programmatic measles control in Bangladesh: A modelling study
Md Abdul Kuddus, Azizur Rahman, Farzana Alam, M. Mohiuddin, Jan Rychtář
PLOS ONE.2023; 18(6): e0283082. CrossRef - Mathematical analysis of a two-strain tuberculosis model in Bangladesh
Md Abdul Kuddus, Emma S. McBryde, Adeshina I. Adekunle, Lisa J. White, Michael T. Meehan
Scientific Reports.2022;[Epub] CrossRef - Age-Specific Mathematical Model for Tuberculosis Transmission Dynamics in South Korea
Sunmi Lee, Hae-Young Park, Hohyung Ryu, Jin-Won Kwon
Mathematics.2021; 9(8): 804. CrossRef - Scenario analysis for programmatic tuberculosis control in Bangladesh: a mathematical modelling study
Md Abdul Kuddus, Michael T. Meehan, Md. Abu Sayem, Emma S. McBryde
Scientific Reports.2021;[Epub] CrossRef - Modeling drug-resistant tuberculosis amplification rates and intervention strategies in Bangladesh
Md Abdul Kuddus, Michael T. Meehan, Lisa J. White, Emma S. McBryde, Adeshina I. Adekunle, Hasnain Seyed Ehtesham
PLOS ONE.2020; 15(7): e0236112. CrossRef - Predictors of job satisfaction and burnout among tuberculosis management nurses and physicians
Hae-Suk Seo, Hyunjoong Kim, Se-Min Hwang, Soo Hyun Hong, In-Young Lee
Epidemiology and Health.2016; 38: e2016008. CrossRef - Is Tuberculosis Still the Number One Infectious Disease in Korea?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5: S1. CrossRef - Journal Publishing: Never Ending Saga
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2014; 5(1): 1. CrossRef
- Analysis of the different interventions scenario for programmatic measles control in Bangladesh: A modelling study



 First
First Prev
Prev


