Search
- Page Path
- HOME > Search
- The effect of the COVID-19 pandemic on the trends and characteristics of natural and unnatural deaths in an urban Sri Lankan cohort viewed through retrospective analysis of forensic death investigations from 2019 to 2022
- Sameera Anuruddha Gunawardena, Nishani Dassanayake, Buddhika Indeewarie Keerawelle, Shivasankarie Kanthasamy, Hasini Ranganatha, Jayani Wathsala Gunawardana
- Osong Public Health Res Perspect. 2023;14(6):468-482. Published online November 23, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0175
- 1,164 View
- 45 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 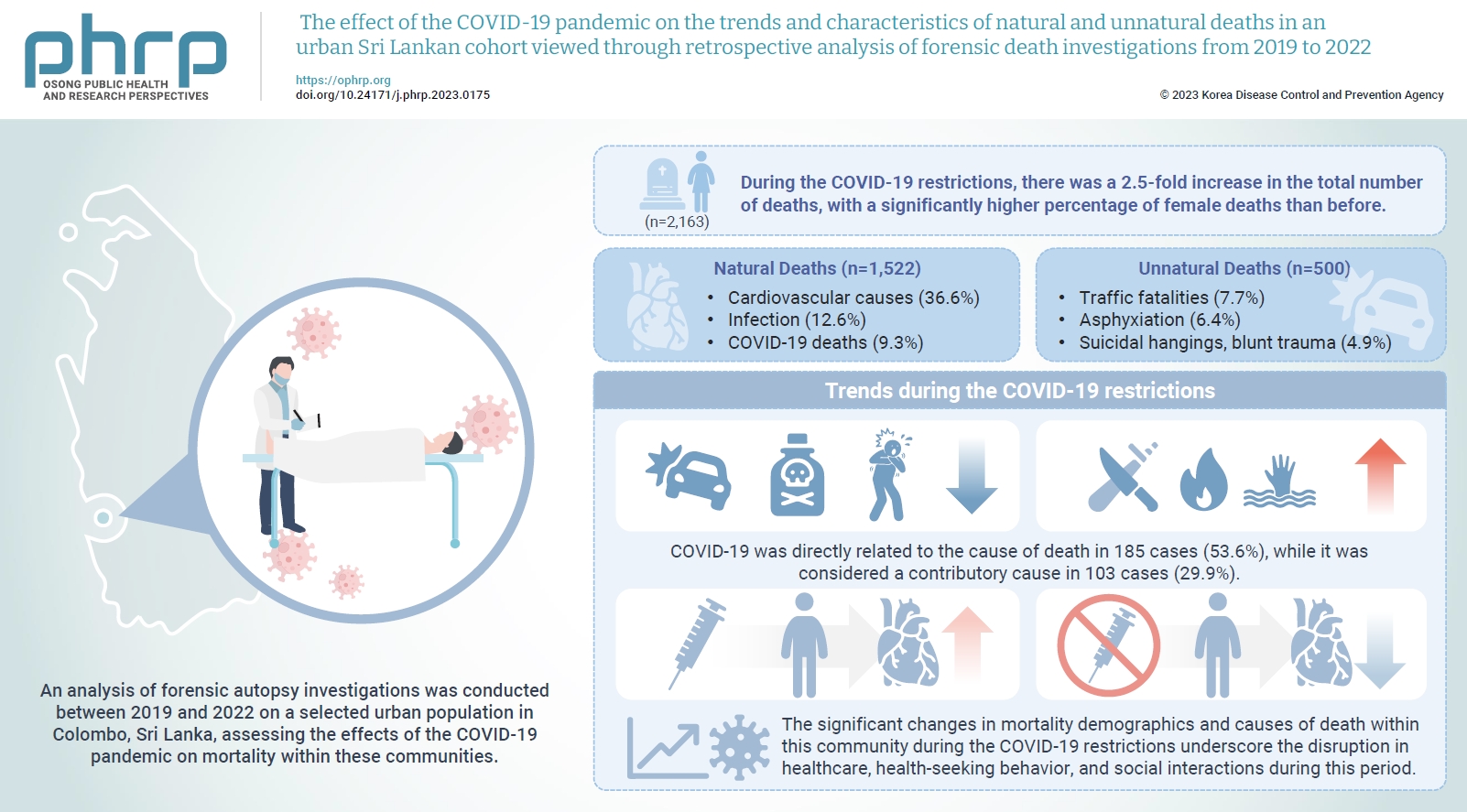
- Objectives
The coronavirus disease 2019 (COVID-19) pandemic has had a severe impact on global health. Apart from the disease itself, the strict restrictions and lockdowns enforced to minimize its spread have also substantially disrupted personal and public health. Methods: An analysis of forensic autopsy investigations was conducted between 2019 and 2022 on a selected urban population in Colombo, Sri Lanka, assessing the effects of the COVID-19 pandemic on mortality within these communities. Results: During the COVID-19 restrictions, there was a 2.5-fold increase in the total number of deaths, with a significantly higher percentage of female deaths than before. The majority of these deaths were due to cardiovascular causes, while COVID-19-related deaths ranked third overall. The highest proportion of COVID-19 deaths occurred among unvaccinated females. The monthly frequency of deaths from traffic accidents, poisoning, and asphyxiation decreased, while deaths from blunt trauma, sharp trauma, burns, and immersion increased. There was also a rise in blunt homicides and a greater number of femicides during the COVID-19 restrictions than in the pre-pandemic period. A significantly higher percentage of males who received the COVID-19 vaccine died from cardiovascular causes compared to those in the unvaccinated group. Conclusion: The significant changes in mortality demographics and causes of death within this community during the COVID-19 restrictions underscore the disruption in healthcare, healthseeking behavior, and social interactions during this period. The vulnerability of individuals residing in highly urbanized areas with lower socioeconomic status, particularly women, is brought into sharp focus.
- Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates
- Yongmoon Kim, Bryan Inho Kim, Sangwoo Tak
- Osong Public Health Res Perspect. 2022;13(6):424-434. Published online November 28, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0212
- 2,732 View
- 111 Download
- 1 Web of Science
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
Although it is widely used as a measure for mortality, the case fatality rate (CFR) ofcoronavirus disease 2019 (COVID-19) can vary over time and fluctuate for many reasons otherthan viral characteristics. To compare the CFRs of different countries in equal measure, weestimated comparable CFRs after adjusting for multiple covariates and examined the mainfactors that contributed to variability in the CFRs among 21 countries.Methods: For statistical analysis, time-series cross-sectional data were collected from OurWorld in Data, CoVariants.org, and GISAID. Biweekly CFRs of COVID-19 were estimated bypooled generalized linear squares regression models for the panel data. Covariates includedthe predominant virus variant, reproduction rate, vaccination, national economic status,hospital beds, diabetes prevalence, and population share of individuals older than age 65. Intotal, 21 countries were eligible for analysis.Results: Adjustment for covariates reduced variation in the CFRs of COVID-19 across countriesand over time. Regression results showed that the dominant spread of the Omicron variant,reproduction rate, and vaccination were associated with lower country-level CFRs, whereasage, the extreme poverty rate, and diabetes prevalence were associated with higher countrylevel CFRs.Conclusion: A direct comparison of crude CFRs among countries may be fallacious, especiallyin a cross-sectional analysis. Our study presents an adjusted comparison of CFRs over timefor a more proper comparison. In addition, our findings suggest that comparing CFRs amongdifferent countries without considering their context, such as the epidemic phase, medicalcapacity, surveillance strategy, and socio-demographic traits, should be avoided. -
Citations
Citations to this article as recorded by- Comments on the article "Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates"
Gaetano Perone
Osong Public Health and Research Perspectives.2023; 14(2): 146. CrossRef
- Comments on the article "Time-series comparison of COVID-19 case fatality rates across 21 countries with adjustment for multiple covariates"
- A spatial analysis of the association between social vulnerability and the cumulative number of confirmed deaths from COVID-19 in United States counties through November 14, 2020
- Baksun Sung
- Osong Public Health Res Perspect. 2021;12(3):149-157. Published online June 2, 2021
- DOI: https://doi.org/10.24171/j.phrp.2020.0372
- 6,655 View
- 150 Download
- 4 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 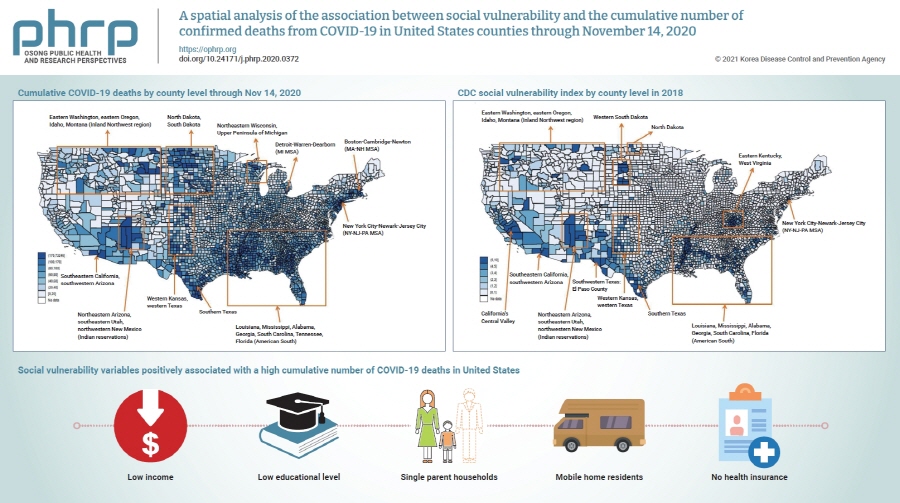
- Objectives
Coronavirus disease 2019 (COVID-19) is classified as a natural hazard, and social vulnerability describes the susceptibility of social groups to potential damages from natural hazards. Therefore, the objective of this study was to examine the association between social vulnerability and the cumulative number of confirmed COVID-19 deaths (per 100,000) in 3,141 United States counties.
Methods
The cumulative number of COVID-19 deaths was obtained from USA Facts. Variables related to social vulnerability were obtained from the Centers for Disease Control and Prevention Social Vulnerability Index and the 2018 5-Year American Community Survey. Data were analyzed using spatial autoregression models.
Results
Lowest income and educational level, as well as high proportions of single parent households, mobile home residents, and people without health insurance were positively associated with a high cumulative number of COVID-19 deaths.
Conclusion
In conclusion, there are regional differences in the cumulative number of COVID-19 deaths in United States counties, which are affected by various social vulnerabilities. Hence, these findings underscore the need to take social vulnerability into account when planning interventions to reduce COVID-19 deaths. -
Citations
Citations to this article as recorded by- Ecological comparison of six countries in two waves of COVID-19
Meiheng Liu, Leiyu Shi, Manfei Yang, Jun Jiao, Junyan Yang, Mengyuan Ma, Wanzhen Xie, Gang Sun
Frontiers in Public Health.2024;[Epub] CrossRef - Social vulnerability and COVID-19 in Maringá, Brazil
Matheus Pereira Libório, Oseias da Silva Martinuci, Patrícia Bernardes, Natália Cristina Alves Caetano Chav Krohling, Guilherme Castro, Henrique Leonardo Guerra, Eduardo Alcantara Ribeiro, Udelysses Janete Veltrini Fonzar, Ícaro da Costa Francisco
Spatial Information Research.2023; 31(1): 51. CrossRef - A county-level analysis of association between social vulnerability and COVID-19 cases in Khuzestan Province, Iran
Mahmoud Arvin, Shahram Bazrafkan, Parisa Beiki, Ayyoob Sharifi
International Journal of Disaster Risk Reduction.2023; 84: 103495. CrossRef - Global mapping of epidemic risk assessment toolkits: A scoping review for COVID-19 and future epidemics preparedness implications
Bach Xuan Tran, Long Hoang Nguyen, Linh Phuong Doan, Tham Thi Nguyen, Giang Thu Vu, Hoa Thi Do, Huong Thi Le, Carl A. Latkin, Cyrus S. H. Ho, Roger C. M. Ho, Md Nazirul Islam Sarker
PLOS ONE.2022; 17(9): e0272037. CrossRef - COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities
Victoria J McGowan, Clare Bambra
The Lancet Public Health.2022; 7(11): e966. CrossRef
- Ecological comparison of six countries in two waves of COVID-19
- Epidemiological, imaging, laboratory, and clinical characteristics and factors related to mortality in patients with COVID-19: a single-center study
- Zohreh Azarkar, Hamid Salehiniya, Toba Kazemi, Hamid Abbaszadeh
- Osong Public Health Res Perspect. 2021;12(3):169-176. Published online May 26, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0012
- 5,714 View
- 120 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Coronavirus disease 2019 (COVID-19) is a novel pandemic. Considerable differences in disease severity and the mortality rate have been observed in different parts of the world. The present study investigated the characteristics and outcomes of patients hospitalized with COVID-19 in Iran.
Methods
We established a retrospective cohort to study hospitalized COVID-19 patients in Iran. Epidemiological, imaging, laboratory, and clinical characteristics and outcomes were recorded from medical documents. The chi-square test, t-test, and logistic regression models were used to analyze the data. A p<0.05 was considered to indicate statistical significance.
Results
In total, 364 cases (207 males and 157 females) were analyzed. The most common symptoms were cough, fever, and dyspnea. Multifocal bilateral ground-glass opacities with peripheral distribution were the predominant imaging finding. The mean age of patients was 54.28±18.81 years. The mean age of patients who died was 71.50±14.60 years. The mortality rate was 17.6%. The total proportion of patients with a comorbidity was 47.5%, and 84.4% of patients who died had a comorbidity. Sex, history of diabetes mellitus, and dyslipidemia were not significantly associated with mortality (p>0.05). However, mortality showed significant relationships with body mass index; age; history of hypertension, chronic kidney disease (CKD), ischemic heart disease, cerebrovascular accident (CVA), pulmonary disease, and cancer; and abnormal high-resolution computed tomography (HRCT) findings (p<0.05 for all). Cancer had the highest odds ratio.
Conclusion
Comorbidities (especially cancer, CKD, and CVA), severe obesity, old age, and abnormal HRCT findings affected the health outcomes of patients hospitalized with COVID-19. -
Citations
Citations to this article as recorded by- Obesity as a Risk Factor for Complications and Mortality in Individuals with SARS-CoV-2: A Systematic Review
Marielle Priscila de Paula Silva-Lalucci, Déborah Cristina de Souza Marques, Pablo Valdés-Badilla, Leonardo Vidal Andreato, Braulio Henrique Magnani Branco
Nutrients.2024; 16(4): 543. CrossRef - Effects of SARS-CoV-2 infections in patients with cancer on mortality, ICU admission and incidence: a systematic review with meta-analysis involving 709,908 participants and 31,732 cancer patients
Mehmet Emin Arayici, Nazlican Kipcak, Ufuktan Kayacik, Cansu Kelbat, Deniz Keskin, Muhammed Emin Kilicarslan, Ahmet Veli Kilinc, Sumeyye Kirgoz, Anil Kirilmaz, Melih Alihan Kizilkaya, Irem Gaye Kizmaz, Enes Berkin Kocak, Enver Kochan, Begum Kocpinar, Fatm
Journal of Cancer Research and Clinical Oncology.2023; 149(7): 2915. CrossRef - Risk Factors Associated with Severity and Death from COVID-19 in Iran: A Systematic Review and Meta-Analysis Study
Ahmad Mehri, Sahar Sotoodeh Ghorbani, Kosar Farhadi-Babadi, Elham Rahimi, Zahra Barati, Niloufar Taherpour, Neda Izadi, Fatemeh Shahbazi, Yaser Mokhayeri, Arash Seifi, Saeid Fallah, Rezvan Feyzi, Koorosh Etemed, Seyed Saeed Hashemi Nazari
Journal of Intensive Care Medicine.2023; 38(9): 825. CrossRef - The association between stroke and COVID-19-related mortality: a systematic review and meta-analysis based on adjusted effect estimates
Shuwen Li, Jiahao Ren, Hongjie Hou, Xueya Han, Jie Xu, Guangcai Duan, Yadong Wang, Haiyan Yang
Neurological Sciences.2022; 43(7): 4049. CrossRef - Mental health status of dentists during COVID‐19 pandemic: A systematic review and meta‐analysis
Hamid Salehiniya, Sare Hatamian, Hamid Abbaszadeh
Health Science Reports.2022;[Epub] CrossRef - Laboratory biomarker predictors for disease progression and outcome among Egyptian COVID-19 patients
Lamiaa A Fathalla, Lamyaa M Kamal, Omina Salaheldin, Mahmoud A Khalil, Mahmoud M Kamel, Hagar H Fahim, Youssef AS Abdel-Moneim, Jawaher A Abdulhakim, Ahmed S Abdel-Moneim, Yomna M El-Meligui
International Journal of Immunopathology and Pharm.2022; 36: 039463202210962. CrossRef - Obesity and Infection: What Have We Learned From the COVID-19 Pandemic
Emilia Vassilopoulou, Roxana Silvia Bumbacea, Aikaterini Konstantina Pappa, Athanasios N. Papadopoulos, Dragos Bumbacea
Frontiers in Nutrition.2022;[Epub] CrossRef
- Obesity as a Risk Factor for Complications and Mortality in Individuals with SARS-CoV-2: A Systematic Review
- Global variation of COVID-19 mortality rates in the initial phase
- Saman Hasan Siddiqui, Azza Sarfraz, Arjumand Rizvi, Fariha Shaheen, Mohammad Tahir Yousafzai, Syed Asad Ali
- Osong Public Health Res Perspect. 2021;12(2):64-72. Published online April 29, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.12.2.03
- 6,593 View
- 149 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objectives
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused devastation in over 200 countries. Italy, Spain, and the United States (US) were most severely affected by the first wave of the pandemic. The reasons why some countries were more strongly affected than others remain unknown. We identified the most-affected and less-affected countries and states and explored environmental, host, and infrastructure risk factors that may explain differences in the SARS-CoV-2 mortality burden.
Methods
We identified the top 10 countries/US states with the highest deaths per population until May 2020. For each of these 10 case countries/states, we identified 6 control countries/states with a similar population size and at least 3 times fewer deaths per population. We extracted data for 30 risk factors from publicly available, trusted sources. We compared case and control countries/states using the non-parametric Wilcoxon rank-sum test, and conducted a secondary cluster analysis to explore the relationship between the number of cases per population and the number of deaths per population using a scalable EM (expectation–maximization) clustering algorithm.
Results
Statistically significant differences were found in 16 of 30 investigated risk factors, the most important of which were temperature, neonatal and under-5 mortality rates, the percentage of under-5 deaths due to acute respiratory infections (ARIs) and diarrhea, and tuberculosis incidence (p <0.05)
Conclusion
Countries with a higher burden of baseline pediatric mortality rates, higher pediatric mortality from preventable diseases like diarrhea and ARI, and higher tuberculosis incidence had lower rates of coronavirus disease 2019-associated mortality, supporting the hygiene hypothesis. -
Citations
Citations to this article as recorded by- Prediction models of COVID-19 fatality in nine Peruvian provinces: A secondary analysis of the national epidemiological surveillance system
Wendy Nieto-Gutierrez, Jaid Campos-Chambergo, Enrique Gonzalez-Ayala, Oswaldo Oyola-Garcia, Alberti Alejandro-Mora, Eliana Luis-Aguirre, Roly Pasquel-Santillan, Juan Leiva-Aguirre, Cesar Ugarte-Gil, Steev Loyola, Sizulu Moyo
PLOS Global Public Health.2024; 4(1): e0002854. CrossRef - The effect of the urban exposome on COVID-19 health outcomes: A systematic review and meta-analysis
Laura Houweling, Anke-Hilse Maitland-Van der Zee, Judith C.S. Holtjer, Somayeh Bazdar, Roel C.H. Vermeulen, George S. Downward, Lizan D. Bloemsma
Environmental Research.2024; 240: 117351. CrossRef - Demographic Characteristics and Status of Vaccinated Individuals with a History of COVID-19 Infection Pre- or Post-Vaccination: A Descriptive Study of a Nationally Representative Sample in Saudi Arabia
Yazed AlRuthia, Haya F. Al-Salloum, Omar A. Almohammed, Amani S. Alqahtani, Hana A. Al-Abdulkarim, Yousef M. Alsofayan, Sami S. Almudarra, Sara H. AlQahtani, Abdullah Almutlaq, Khaled Alabdulkareem, Bander Balkhi, Hamoud T. Almutairi, Abdullah S. Alanazi,
Vaccines.2022; 10(2): 323. CrossRef - Temporal variation, socioeconomic status, and out‐of‐hospital deaths as factors that influence mortality rates among hospitalized COVID‐19 patients receiving ACEIs/ARBs
Owais M. Aftab, Anurag Modak, Jai C. Patel
The Journal of Clinical Hypertension.2022; 24(4): 519. CrossRef - Coinfection of leptospirosis and coronavirus disease 2019: A retrospective case series from a coastal region in South India
Nitin Gupta, William Wilson, Prithvishree Ravindra, Roshini Raghu, Kavitha Saravu
Journal of Medical Virology.2022; 94(9): 4508. CrossRef - Dietary, comorbidity, and geo-economic data fusion for explainable COVID-19 mortality prediction
Milena Trajanoska, Risto Trajanov, Tome Eftimov
Expert Systems with Applications.2022; 209: 118377. CrossRef - Paraoxonase 1 rs662 polymorphism, its related variables, and COVID-19 intensity: Considering gender and post-COVID complications
Zohreh-Al-Sadat Ghoreshi, Mojtaba Abbasi-jorjandi, Gholamreza Asadikaram, Mohsen Sharif-zak, Fatemeh Seyedi, Mohammad Khaksari Haddad, Mohammadreza Zangouey
Experimental Biology and Medicine.2022; : 153537022211285. CrossRef - Clinical Effect of Q192R Paraoxonase 1 Polymorphism and its Related Variables on the COVID-19 Intensity Considering Gender and Post-COVID Complications
Zohreh-al-sadat Ghoreshi, Mojtaba abasi, Gholamreza Asadikaram, Mohsen sharif-zak, Mitra Rezazadeh-Jabalbarzi, Hamidreza rashidinejad, Mohammadreza Zangouey
SSRN Electronic Journal .2022;[Epub] CrossRef - Risk Factors and a Novel Score (CARI-65) Predicting Mortality in COVID-19 Patients
Fayaz Ahmad Sofi, Umar Hafiz Khan, Sonaullah Shah, Nazia Mehfooz, Farhana Siraj, Afshan Shabir, Tajamul Hussain Shah, Muzaffar Bindroo, Mushtaq Ahmad, Rafi Ahmed Jan, Asma Shah, Faizan Wani
Indian Journal of Respiratory Care.2022; 11(2): 154. CrossRef - Variances in BCG protection against COVID-19 mortality: A global assessment
Zouina Sarfraz, Azza Sarfraz, Krunal Pandav, Sarabjot Singh Makkar, Saman Hasan Siddiqui, Gaurav Patel, Tania Platero-Portillo, Bishnu Mohan Singh, Mohamed Iburahim Haja Maideen, Deepika Sarvepalli, Muzna Sarfraz, Jose Cardona-Guzman, Marcos A. Sanchez-Go
Journal of Clinical Tuberculosis and Other Mycobac.2021; 24: 100249. CrossRef
- Prediction models of COVID-19 fatality in nine Peruvian provinces: A secondary analysis of the national epidemiological surveillance system
- Comparative Analysis of the Trends in Medical Utilization of Cancer Inpatients in Korea
- Hyun-Ju Lee, Sung-Soo Kim
- Osong Public Health Res Perspect. 2017;8(5):342-350. Published online October 31, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.5.08
- 3,366 View
- 32 Download
-
 Abstract
Abstract
 PDF
PDF Objectives Cancer has attracted worldwide attention. The incidence and prevalence are increasing, and it is the main cause of death. The purpose of this study was to identify the characteristics of hospitalized cancer patients.
Methods This study is a secondary data study using the Korean National Hospital Discharge In-depth Injury Survey Data conducted annually by the Korea Centers for Disease Control and Prevention. Using these data, we extracted inpatients who principal diagnosis is cancer for nine years from 2005 to 2013.
Results According to the analysis, the annual trend of cancer inpatients is steadily increasing. In 2025, it is expected to increase to about 670,000 inpatients. A cancer diagnosis created a change in medical utilization depending on the characteristics of patients and hospital. Men are more at risk of cancer than women. The number of hospital beds and hospital days were inversely proportional to cancer inpatients. There was also a difference in the equity of medical utilization by region. Other cancer management policies should be based on sex.
Conclusion Populations between the ages of 45 and 64 years should be a priority in cancer policy. Because of the long-term hospitalization of patients with death as the outcome, a terminal cancer patient care facility is needed. These conclusions can provide a basis for various health policies.
- Epidemiology and Inequality in the Incidence and Mortality of Nasopharynx Cancer in Asia
- Neda Mahdavifar, Mahshid Ghoncheh, Abdollah Mohammadian-Hafshejani, Bahman Khosravi, Hamid Salehiniya
- Osong Public Health Res Perspect. 2016;7(6):360-372. Published online December 31, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.11.002
- 4,004 View
- 21 Download
- 45 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
One of the most common head and neck cancers is nasopharynx cancer. Knowledge about the incidence and mortality of this disease and its distribution in terms of geographical areas is necessary for further study and better planning. Therefore, this study was conducted with the aim of determining the incidence and mortality rates of nasopharynx cancer and its relationship with the Human Development Index (HDI) in Asia in 2012.
Methods
The aim of this ecologic study was to assess the correlation between age-specific incidence rate (ASIR) and age-specific mortality rate (ASMR) with HDI and its components, which include the following: life expectancy at birth, mean years of schooling, and gross national income per capita. Data about SIR and SMR for every Asian country for 2012 were obtained from the global cancer project. We used the correlation bivariate method for the assessment. Statistical significance was assumed if p < 0.05. All reported p values are two-sided. Statistical analyses were performed using SPSS (Version 15.0, SPSS Inc.).
Results
A total of 68,272 cases (males, 71.02%; females, 28.97%; sex ratio, 2.45) and 40,530 mortalities (males, 71.63%; females, 28.36%; sex ratio, 2.52) were recorded in Asian countries in 2012. The five countries with the highest ASIR of nasopharynx cancer were Malaysia, Singapore, Indonesia, Vietnam, and Brunei, and the five countries with the highest ASMR were Indonesia, Vietnam, Singapore, Malaysia, and Brunei. The correlation between HDI and ASIR was 0.097 (p = 0.520) [0.105 in men (p = 0.488) and 0.119 in women (p = 0.901)]. The correlation between HDI and ASMR was –0.102 (p = 0.502) [–0.072 in men (p = 0.633) and –0.224 in women (p = 0.134)].
Conclusion
Nasopharynx cancer is native to Southeast Asia. The highest incidence and mortality rates are found in Malaysia, Singapore, Indonesia, Vietnam, and Brunei. No significant relation was found between the standardized incidence and mortality rates of nasopharynx cancer and the HDI components. Further studies are recommended in Southeast Asian countries in order to find the etiology of cancer, as well as its diagnosis and treatment. -
Citations
Citations to this article as recorded by- Regulatory role of miRNAs in nasopharyngeal cancer involving PTEN/PI3K/AKT, TGFβ/SMAD, RAS/MAPK, Wnt/β‐catenin and pRB‐E2F signaling pathways: A review
Rabiatul Basria S. M. N. Mydin, Adam Azlan, Simon I. Okekpa, Nigel J. Gooderham
Cell Biochemistry and Function.2024;[Epub] CrossRef - Rapid and sensitive detection of Epstein-Barr virus antibodies in nasopharyngeal carcinoma by chemiluminescence strips based on iron-porphyrin single atom nanozyme
Daji Wang, Jie Wang, Dan Liu, Jiuyang He, Meiying Wang, Haibing Huang, Guohui Nie, Hui Ding, Xiyun Yan
Nano Research.2024; 17(3): 1827. CrossRef - The association between chronic sinonasal inflammation and nasopharyngeal carcinoma - A systematic review and meta-analysis
Yuxing Wang, Kylynn Kathleen Koh, Elizabeth Chua, Kimberley Liqin Kiong, Yu Heng Kwan, Tze Choong Charn
American Journal of Otolaryngology.2024; 45(2): 104206. CrossRef - Correlation between socioeconomic indices and epidemiological indices of thyroid cancer from 1990 to 2019 year: a global ecologic study
Zahra Maleki, Jafar Hassanzadeh, Haleh Ghaem
BMC Cancer.2024;[Epub] CrossRef - Study of Three Potential Diagnostic Biomarkers in Nasopharyngeal Carcinoma Samples from Guilan, North of Iran
Saghi Jani Kargar Moghaddam, Amaneh Mohammadi Roushandeh, Mehryar Habibi Roudkenar, Shadman Nemati, Nima Najafi-Ghalehlou, Toofan Pakzad, Masoud Hamidi
International Archives of Otorhinolaryngology.2023; 27(03): e461. CrossRef - Oncogenic Viruses-Encoded microRNAs and Their Role in the Progression of Cancer: Emerging Targets for Antiviral and Anticancer Therapies
Mahmoud Kandeel
Pharmaceuticals.2023; 16(4): 485. CrossRef - Nasopharyngeal Carcinoma Subtype Discovery via Immune Cell Scores from Tumor Microenvironment
Yanbo Sun, Yun Liu, Hanqi Chu, Zhen-Jian Zhuo
Journal of Immunology Research.2023; 2023: 1. CrossRef - The application of Aptamer in biomarker discovery
Yongshu Li, Winnie Wailing TAM, Yuanyuan Yu, Zhenjian Zhuo, Zhichao Xue, Chiman Tsang, Xiaoting Qiao, Xiaokang Wang, Weijing Wang, Yongyi Li, Yanyang Tu, Yunhua Gao
Biomarker Research.2023;[Epub] CrossRef - Blood-based DNA methylation in advanced Nasopharyngeal Carcinoma exhibited distinct CpG methylation signature
Koustav Chatterjee, Sudipa Mal, Monalisha Ghosh, Nabanita Roy Chattopadhyay, Sankar Deb Roy, Koushik Chakraborty, Syamantak Mukherjee, Moatoshi Aier, Tathagata Choudhuri
Scientific Reports.2023;[Epub] CrossRef - Circular RNA circ_0008450 regulates the proliferation, migration, invasion, apoptosis and chemosensitivity of CDDP-resistant nasopharyngeal carcinoma cells by the miR-338-3p/SMAD5 axis
Lin Liu, Bin Lu, Yan Li
Anti-Cancer Drugs.2022; 33(1): e260. CrossRef - Hypermethylation of the RASSF1A gene promoter as the tumor DNA marker for nasopharyngeal carcinoma
Thuan Duc Lao, Hue Hong Thieu, Dung Huu Nguyen, Thuy Ai Huyen Le
The International Journal of Biological Markers.2022; 37(1): 31. CrossRef - miR-135b-5p Targets SIRT1 to Inhibit Deacetylation of c-JUN and Increase MMP7 Expression to Promote Migration and Invasion of Nasopharyngeal Carcinoma Cells
Yali Cheng
Molecular Biotechnology.2022; 64(6): 693. CrossRef - Trends in the Incidence of Nasopharyngeal Cancer in Saudi Arabia Across One Decade (2007 to 2016)
Abdualrahman F Kabli, Khalil F Miyajan, Abdulmohsen S Alqurashi, Ammar K Mandili, Revan M Mujahed, Bayan F Hafiz, Roaa M Mandora, Ameen Z Herabi
Cureus.2022;[Epub] CrossRef - Causes of Death in Long-Term Nasopharyngeal Carcinoma Survivors
Shi-Ping Yang, Ming-Yue Rao, Qing-Shuang Chen, Ping Zhou, Chen-Lu Lian, San-Gang Wu
Frontiers in Public Health.2022;[Epub] CrossRef - Epstein-Barr Virus (EBV) Is Mostly Latent and Clonal in Angioimmunoblastic T Cell Lymphoma (AITL)
Racha Bahri, François Boyer, Mohamad Adnan Halabi, Alain Chaunavel, Jean Feuillard, Arnaud Jaccard, Sylvie Ranger-Rogez
Cancers.2022; 14(12): 2899. CrossRef - Ferroptosis-related gene ATG5 is a novel prognostic biomarker in nasopharyngeal carcinoma and head and neck squamous cell carcinoma
Ming Shi, Jiangnan Du, Jingjing Shi, Yunchuanxiang Huang, Yan Zhao, Lan Ma
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Platelet to Lymphocytes Ratio to Predict Nasopharyngeal Carcinoma Progressivity
Goesti Yudistira, Yussy Afriani Dewi, Melati Sudiro
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 2189. CrossRef - Skin sparing in intensity-modulated radiation therapy of nasopharyngeal carcinoma
MisbaHamid Baba, BenoyK Singh, Shaq ulQamar Wani
Journal of Medical Physics.2022; 47(3): 243. CrossRef - Assessment of Response to Chemoradiation and Radiation Therapy in Patients with Nasopharyngeal Carcinoma
Sebastian Ario Susanto, Yussy Afriani Dewi, Raden Ayu Hardianti Saputri
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 2307. CrossRef - Genetic variants in NKG2D axis and susceptibility to Epstein–Barr virus-induced nasopharyngeal carcinoma
Nguyen Hoang Viet, Nguyen Quang Trung, Le Thanh Dong, Ly Quoc Trung, J. Luis Espinoza
Journal of Cancer Research and Clinical Oncology.2021; 147(3): 713. CrossRef - Corticosteroid Therapy in Optic Neuropathy Secondary to Nasopharyngeal Carcinoma
Zulaikha Wahab, Evelyn Tai, Wan-Hazabbah Wan Hitam, Khairy Shamel Sonny Teo
Cureus.2021;[Epub] CrossRef - The Effect of Hispidulin, a Flavonoid from Salvia plebeia, on Human Nasopharyngeal Carcinoma CNE-2Z Cell Proliferation, Migration, Invasion, and Apoptosis
Yiqun Dai, Xiaolong Sun, Bohan Li, Hui Ma, Pingping Wu, Yingping Zhang, Meilin Zhu, Hong-Mei Li, Minjian Qin, Cheng-Zhu Wu
Molecules.2021; 26(6): 1604. CrossRef - δ-Tocotrienol induces apoptosis and inhibits proliferation of nasopharyngeal carcinoma cells
Junjun Shen, Tao Yang, Yiping Tang, Tianyi Guo, Ting Guo, Tao Hu, Feijun Luo, Qinlu Lin
Food & Function.2021; 12(14): 6374. CrossRef - WNT8B as an Independent Prognostic Marker for Nasopharyngeal Carcinoma
Chawalit Ngernsombat, Pongphol Prattapong, Noppadol Larbcharoensub, Krittika Khotthong, Tavan Janvilisri
Current Oncology.2021; 28(4): 2529. CrossRef - Nasopharyngeal Carcinoma and Its Association with Epstein-Barr Virus
Harish N. Vasudevan, Sue S. Yom
Hematology/Oncology Clinics of North America.2021; 35(5): 963. CrossRef - Association between stage and histopathological type of nasopharyngeal cancer on occurrence of postirradiation otitis media with effusion
Lina Lasminingrum, Shinta Fitri Boesoeri, Sally Mahdiani, Eveline Sabrina Ranti
International Journal of Surgery Open.2021; 36: 100376. CrossRef - Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma
Pui Yan Siak, Alan Soo-Beng Khoo, Chee Onn Leong, Boon-Peng Hoh, Shiau-Chuen Cheah
Cancers.2021; 13(14): 3490. CrossRef - Carcinomatous‑like mastitis due to axillary lymphadenopathy in a case of nasopharyngeal carcinoma: A case report
Cristina Oprean, Nusa Segarceanu, Alexandra Stan, Cristian Suciu, Daciana Grujic, Ioana Rivis, Alis Liliana Dema, Ana Bredicean
Experimental and Therapeutic Medicine.2021;[Epub] CrossRef - Dosimetric Comparison of Helical Tomotherapy, Volume-Modulated Arc Therapy, and Fixed-Field Intensity-Modulated Radiation Therapy in Locally Advanced Nasopharyngeal Carcinoma
Shan Lu, Huiqi Fan, Xueyuan Hu, Xin Li, Yingying Kuang, Deyang Yu, Shanshan Yang
Frontiers in Oncology.2021;[Epub] CrossRef - The dosimetric comparison between tomotherapy and RapidArc in normal tissue sparing for nasopharyngeal carcinoma
Pubade Kaewpruk, Somvilai Chakrabandhu, Somsak Wanwilairat, Wannapha Nobnop
Journal of Radiotherapy in Practice.2020; 19(3): 237. CrossRef - Combination of Plasma MIF and VCA-IgA Improves the Diagnostic Specificity for Patients With Nasopharyngeal Carcinoma
Ning Xue, Shan Xing, Weiguo Ma, Jiahe Sheng, Zhiliang Huang, Qingxia Xu
Technology in Cancer Research & Treatment.2020; 19: 153303382093577. CrossRef - Pathological features of nasopharyngeal carcinoma: A single-center study in Vietnam
Nguyen Cuong Pham, Thanh Xuan Nguyen, Nguyen Tuong Pham, Thanh Chinh Phan, Hai Thanh Phan
Annals of Cancer Research and Therapy.2020; 28(2): 125. CrossRef - Association between variant alleles of major histocompatibility complex class II regulatory genes and nasopharyngeal carcinoma susceptibility
Ping Zhou, Sha Liu, Nan-Nan Ji, Shuang Zhang, Peng Wang, Bing Lin, Ping Yang, Xian-Tao Lin, Yi-Zheng Cai, Zi-Ming Wang, Han Zhou, Shi-Yao Sun, Xin-Bao Hao
European Journal of Cancer Prevention.2020; 29(6): 531. CrossRef - Hyperperfusion Syndrome and Baroreflex Failure following Carotid Artery Angioplasty and Stenting for Symptomatic Radiation-Associated Carotid Artery Stenosis
Hui-Meng Chang
Case Reports in Neurology.2020; 12(Suppl. 1): 76. CrossRef - Novel patterns of the Epstein-Barr nuclear antigen (EBNA-1) V-Val subtype in EBV-associated nasopharyngeal carcinoma from Vietnam
LD Thuan, ND Kha, NT Minh, LHA Thuy
Balkan Journal of Medical Genetics.2019; 22(1): 61. CrossRef - miR-29c regulates resistance to paclitaxel in nasopharyngeal cancer by targeting ITGB1
Limin Huang, Chaoquan Hu, Hui Chao, Rongpin Wang, He Lu, Hong Li, Hui Chen
Experimental Cell Research.2019; 378(1): 1. CrossRef - Systematic review and meta-analysis of prognostic microRNA biomarkers for survival outcome in nasopharyngeal carcinoma
Shanthi Sabarimurugan, Chellan Kumarasamy, Siddhartha Baxi, Arikketh Devi, Rama Jayaraj, Yukinori Takenaka
PLOS ONE.2019; 14(2): e0209760. CrossRef - Epstein‐Barr virus strain variation and cancer
Teru Kanda, Misako Yajima, Kazufumi Ikuta
Cancer Science.2019; 110(4): 1132. CrossRef - Nasopharyngeal cancer in Saudi Arabia: Epidemiology and possible risk factors
Abdullah Dakheel Alotaibi, Hussain Gadelkarim Ahmed, Abdelbaset Mohamed Elasbali
Journal of Oncological Sciences.2019; 5(1): 23. CrossRef - Association BetweenLMP-1,LMP-2, and miR-155 Expression as Potential Biomarker in Nasopharyngeal Carcinoma Patients: A Case/Control Study in Vietnam
Thuan Duc Lao, Thuy Ai Huyen Le
Genetic Testing and Molecular Biomarkers.2019; 23(11): 815. CrossRef - Lapatinib sensitivity in nasopharyngeal carcinoma is modulated by SIRT2-mediated FOXO3 deacetylation
Sathid Aimjongjun, Zimam Mahmud, Yannasittha Jiramongkol, Glowi Alasiri, Shang Yao, Ernesto Yagüe, Tavan Janvilisri, Eric W.-F. Lam
BMC Cancer.2019;[Epub] CrossRef - PPARβ/δ Agonist GW501516 Inhibits Tumorigenicity of Undifferentiated Nasopharyngeal Carcinoma in C666-1 Cells by Promoting Apoptosis
Yangyang Ji, Hui Li, Fang Wang, Linglan Gu
Frontiers in Pharmacology.2018;[Epub] CrossRef - Pembrolizumab in Asia‐Pacific patients with advanced head and neck squamous cell carcinoma: Analyses from KEYNOTE‐012
Makoto Tahara, Kei Muro, Yasuhisa Hasegawa, Hyun Cheol Chung, Chia‐Chi Lin, Bhumsuk Keam, Kenichi Takahashi, Jonathan D. Cheng, Yung‐Jue Bang
Cancer Science.2018; 109(3): 771. CrossRef - Childhood Nasopharyngeal Carcinoma (NPC): A Review of Clinical-Imaging Features and Recent Trends in Management
Mark Yoi Sun Soo
International Journal of Pediatrics and Child Heal.2018; 6: 1. CrossRef - KISS1gene suppresses metastasis of nasopharyngeal cancerviaactivation of the ERK1/2 pathway
Tingting Li, Qian Sun, Yan Zhou, Zelai He, Hao Liu, Ping Xiang, Jin Xi, Xiazi Zhang, Hao Jiang
RSC Advances.2017; 7(84): 53445. CrossRef
- Regulatory role of miRNAs in nasopharyngeal cancer involving PTEN/PI3K/AKT, TGFβ/SMAD, RAS/MAPK, Wnt/β‐catenin and pRB‐E2F signaling pathways: A review



 First
First Prev
Prev


