Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(5); 2023 > Article
-
Original Article
The risk associated with psychiatric disturbances in patients with diabetes in Indonesia (2018): a cross-sectional observational study -
Siti Isfandari1
 , Betty Roosihermiatie1
, Betty Roosihermiatie1 , Sulistyowati Tuminah1
, Sulistyowati Tuminah1 , Laurentia Konadi Mihardja2,3
, Laurentia Konadi Mihardja2,3
-
Osong Public Health and Research Perspectives 2023;14(5):368-378.
DOI: https://doi.org/10.24171/j.phrp.2023.0144
Published online: October 18, 2023
1Research Center for Public Health and Nutrition, Research Organization for Health, National Research and Innovation Agency, Bandung, Indonesia
2Research Center for Pre-Clinical and Clinical Medicine, Research Organization for Health, National Research and Innovation Agency, Bandung, Indonesia
3Faculty of Medicine, University of Malahayati, Bandar Lampung, Indonesia
- Corresponding author: Sulistyowati Tuminah Research Center for Public Health and Nutrition, Research Organization for Health, National Research and Innovation Agency, Cibinong Science Center, Jalan Raya Jakarta-Bogor Km.46, Kec. Cibinong, Kabupaten Bogor, West Java 16915, Indonesia E-mail: suli017@brin.go.id / watidarjoko@gmail.com
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
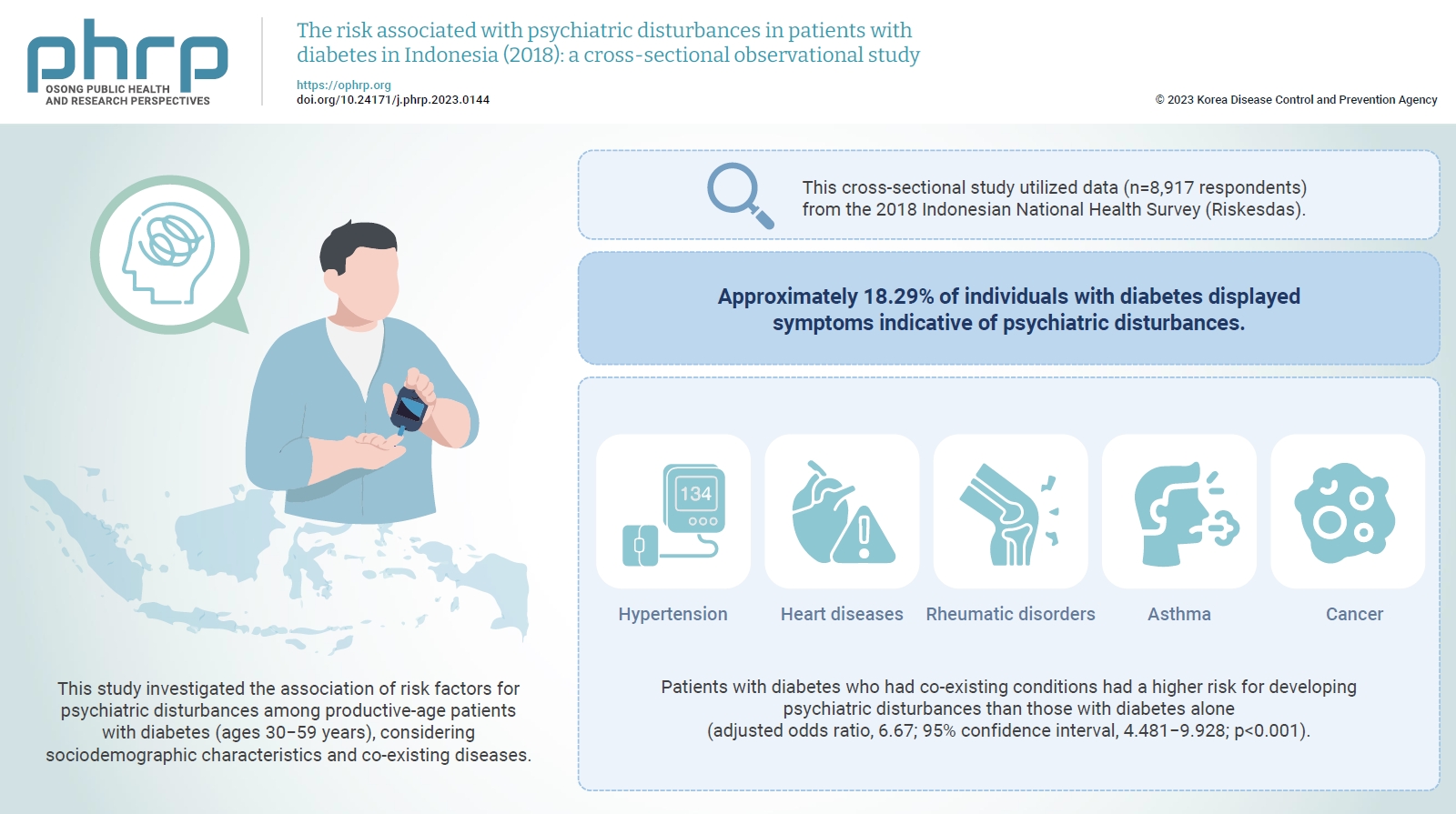
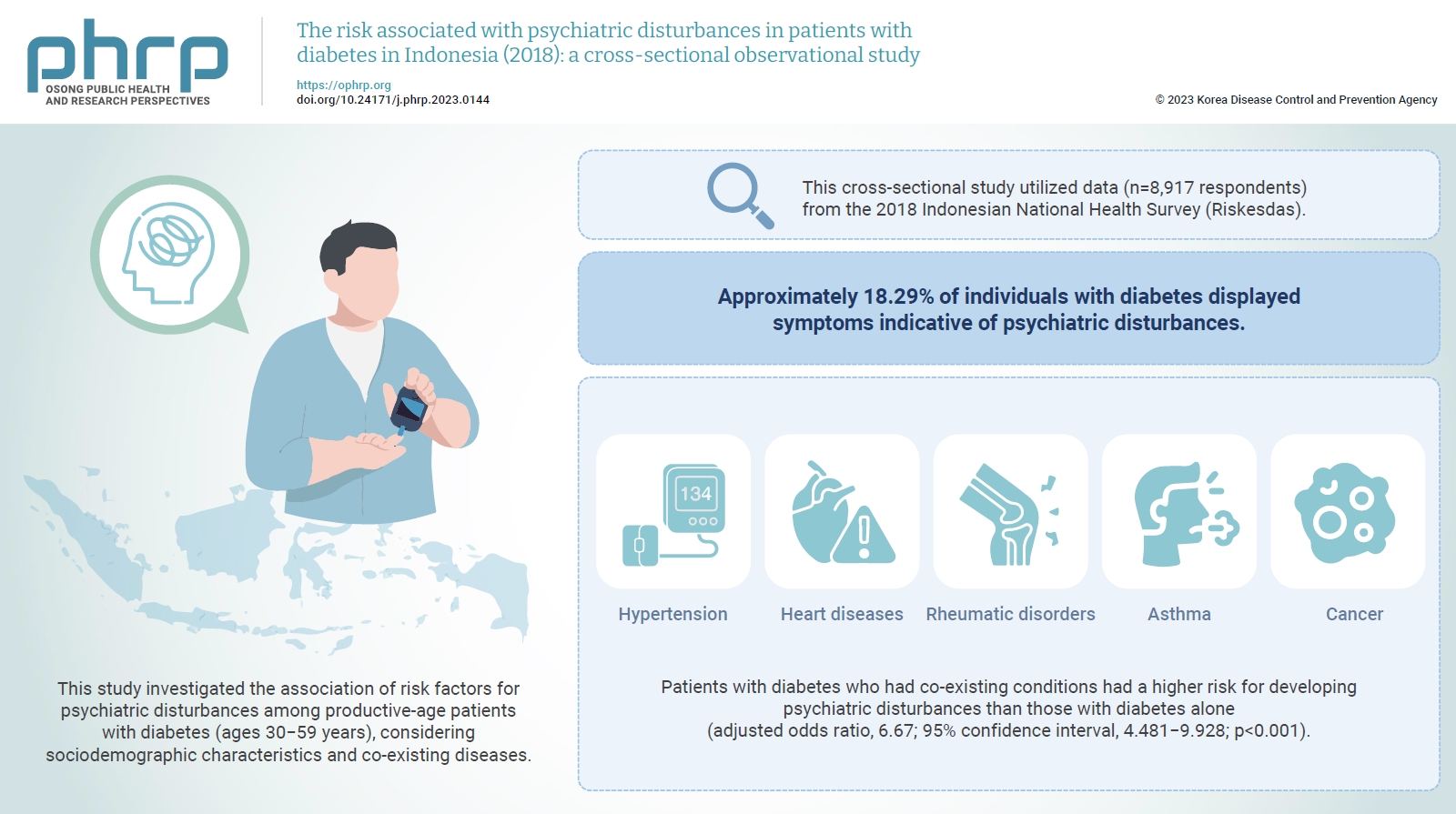
Objectives
- The global prevalence of psychiatric disturbances is rising, detrimentally affecting the quality of care and treatment outcomes for individuals, particularly those with diabetes.This study investigated the association of risk factors for psychiatric disturbances among productive-age patients with diabetes (ages 30−59 years), considering sociodemographic characteristics and co-existing diseases. The risk factors considered included sociodemographic factors (e.g., residence, age, sex, marital status, education, and occupation) and co-existing diseases (e.g., hypertension, heart disease, stroke, renal failure, rheumatism, asthma, and cancer).
-
Methods
- This cross-sectional study utilized data from the 2018 Indonesian National Health Survey (Riskesdas). The study population comprised respondents aged between 30 and 59 years who had diabetes and had completed the 20-question self-reporting questionnaire (SRQ-20). After the exclusion of incomplete SRQ-20 data, the sample included 8,917 respondents. Data were analyzed using logistic regression.
-
Results
- Approximately 18.29% of individuals with diabetes displayed symptoms indicative of psychiatric disturbances. After adjusting for sociodemographic factors such as age, sex, education level, occupation, marital status, and place of residence, patients with diabetes who had co-existing conditions such as hypertension, heart diseases, rheumatic disorders, asthma, or cancer had a higher risk for developing psychiatric disturbances than those with diabetes alone (adjusted odds ratio, 6.67; 95% confidence interval, 4.481−9.928; p<0.001).
-
Conclusion
- The elevated risk of psychiatric disturbances among patients with diabetes who had comorbidities underscores the importance of addressing mental health issues in the management of diabetes, especially in patients with concurrent disease conditions.
- Diabetes mellitus is a widespread chronic disease with substantial medical and economic consequences [1]. The International Diabetes Federation estimates that around 451 million adults globally are living with diabetes [2]. In Indonesia, it is the third leading cause of disability-adjusted life years [3]. The coexistence of comorbidities like cardiovascular diseases with diabetes can elevate the risk of premature mortality, underscoring the need for effective diabetes management [4].
- Depression is a psychiatric disturbance that can profoundly impact an individual’s functioning, contribute to physical health issues, and decrease life expectancy. The global prevalence of psychiatric disturbances, including depression, is substantial, affecting approximately 300 million people at present [5,6]. Individuals with diabetes are more likely to exhibit depressive symptoms compared to those without the condition [7]. Both conditions can impede treatment adherence, disrupt metabolic control, and result in poor compliance with medication and dietary plans. As a result, these conditions can lower the quality of life and escalate healthcare costs.
- The concurrent presence of hypertension and diabetes alongside psychiatric disorders detrimentally impacts both healthcare outcomes and prognosis. A comprehensive survey carried out by the World Health Organization (WHO) across 60 countries reported that comorbid depression affects 9.3% to 23.0% of individuals with chronic diseases [8].
- Understanding the impact of psychiatric disturbances on individuals with type 2 diabetes mellitus is essential for achieving treatment goals [1]. Prior research exploring the connection between diabetes and psychiatric disturbances in Indonesia has predominantly focused on healthcare environments [9,10]. This study investigated the risk association of psychiatric disturbances among patients with diabetes, considering sociodemographic factors and concurrent disease conditions. The insights gained from this analysis are beneficial for healthcare providers, as they can guide the creation of programs and interventions that encourage treatment compliance and self-care among individuals with diabetes.
Introduction
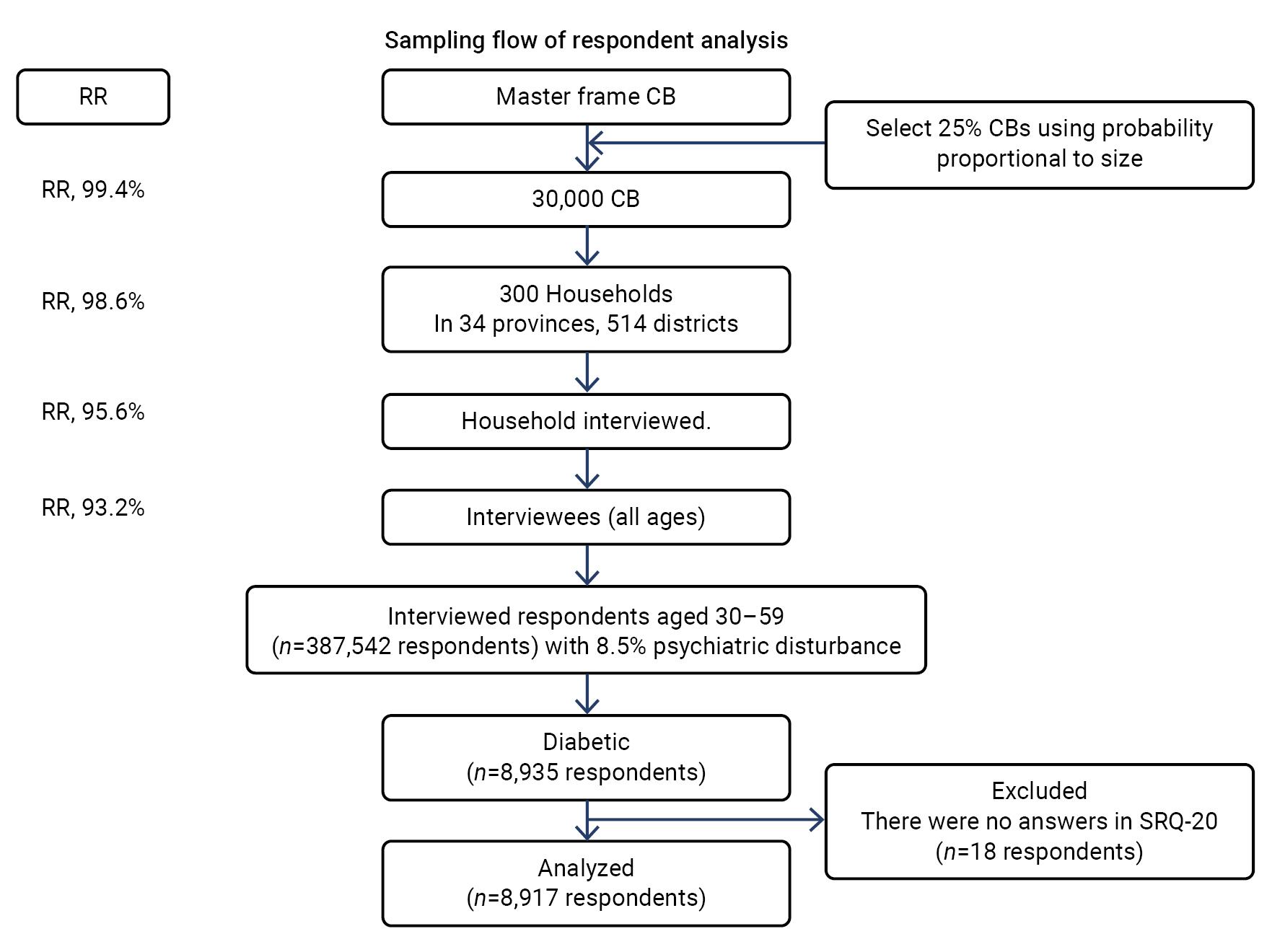
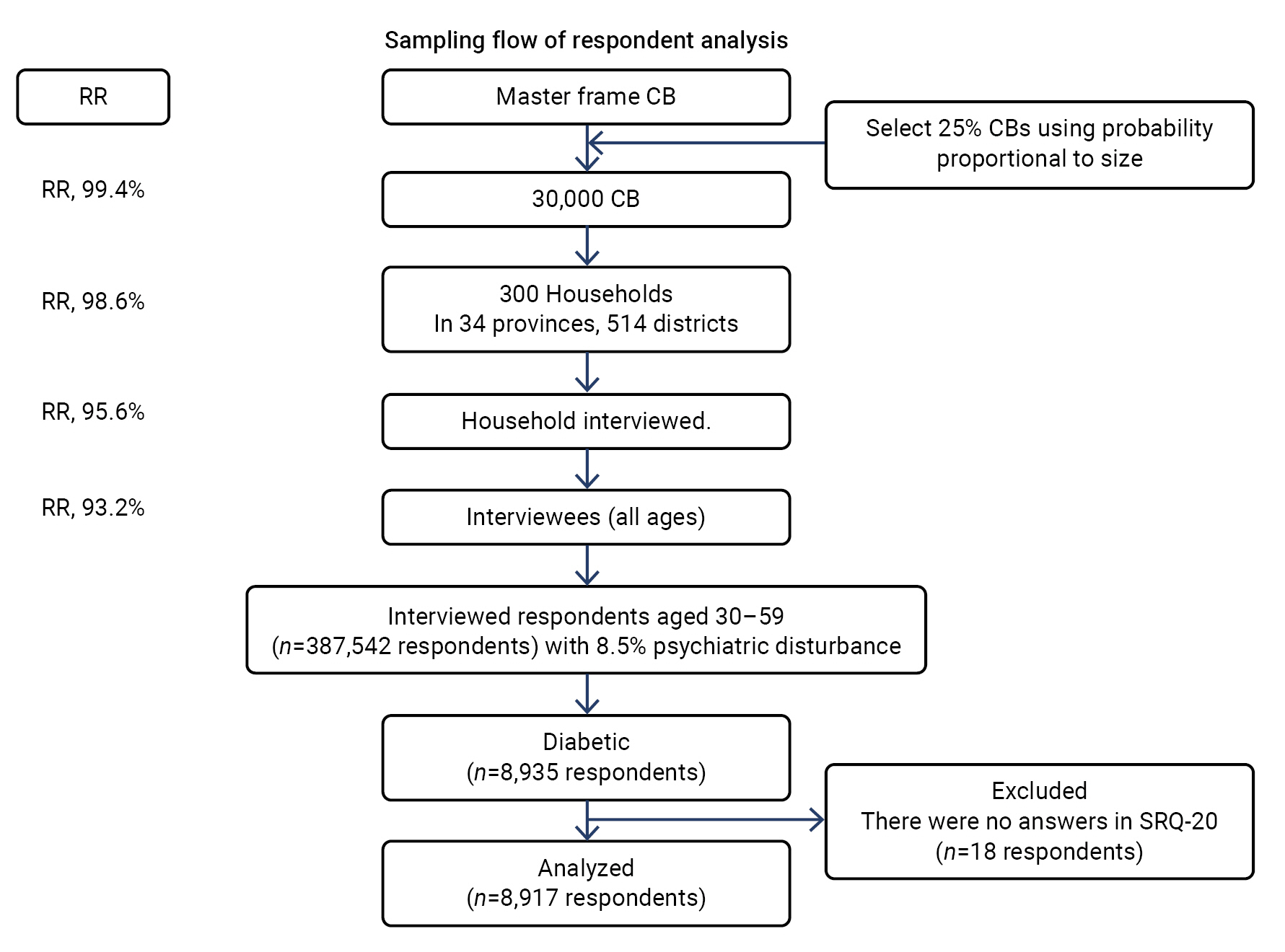
- Study Design
- We analyzed data from the 2018 National Health Survey (NHS), which was carried out by the Ministry of Health in the Republic of Indonesia. The NHS employed a multistage systematic random sampling approach to select participants. The initial step involved identifying and designating census blocks as primary sampling units (PSUs). From each PSU, census blocks were chosen using the probability proportional to size method, which was based on the master sampling from the 2010 Indonesian Central Bureau of Statistics (Badan Pusat Statistik). This process resulted in the selection of 180,000 census blocks from a total of 720,000, representing both urban and rural areas within each sub-district at the district level. Researchers carried out face-to-face interviews with all members of the selected households who had resided there for a minimum of 6 months and were part of the same food management unit [11,12]. Our analysis focused on the age group of 30 to 59 years from the 387,542 respondents in the 2018 Indonesian NHS. This focus was due to the reported sharp increase in the prevalence of diabetes within this demographic. Among the participants, we identified 8,935 individuals (2.3%) with diabetes. However, we excluded 18 individuals (0.2%) from the analysis because they had not completed the 20-question self-reporting questionnaire (SRQ-20). Consequently, our study incorporated complete data from 8,917 individuals (Figure 1) [11,12].
- Samples
- This study included participants in the Indonesian NHS of 2018. The inclusion criteria specified that participants must be Indonesian, have participated in the 2018 NHS, have diabetes, and be between the ages of 30 and 59 years. The exclusion criteria were set to omit any participants with incomplete data, including those without the SRQ-20. The study sample comprised 8,917 participants, all of whom were between the ages of 30 and 59 and had diabetes.
- The data were gathered from the Health Development Policy Agency, adhering to specific requirements and procedures available at https://www.badankebijakan.kemkes.go.id/.
- The outcome variable under investigation was psychiatric disturbances, which included anxiety and depression, and were determined based on the respondent’s mental and emotional state over the past 30 days. The SRQ, developed by the WHO, was utilized for this purpose. This questionnaire is specifically designed to identify psychiatric disturbances, particularly in developing countries. It comprises 20 yes-or-no questions pertaining to the respondent’s mental state over the previous 30 days (SRQ-20). The reliability of the SRQ-20 in this study was confirmed by a Cronbach α of 0.899 (Supplementary Material 1). This Cronbach α value of 0.899 (>0.60) indicates that all the questionnaire items related to psychiatric disturbances were reliable. Respondents were categorized as having a psychiatric disturbance if they responded affirmatively to at least 6 questions [13,14].
- The primary explanatory variable in this study was diabetes status, which was categorized as either with or without co-existing disease conditions. These co-existing conditions encompassed a range of diseases such as heart disease, stroke, hypertension, renal failure, rheumatic disorders, asthma, or cancer, all of which were diagnosed by a medical professional. The multivariate analyses incorporated several covariates, including sex (categorized as male or female), age groups (divided into 30−39 years, 40−49 years, and 50−59 years), occupation (distinguished as working or not working), marital status (classified as single or married), education (categorized as either having a high school certificate or not), and place of residence (classified as either rural or urban).
- Data Analysis
- We conducted a series of univariate, bivariate, and multivariate analyses. The multivariate analysis involved the execution of logistic regression using IBM SPSS ver. 21.0 (IBM Corp.). Variables from the bivariate analysis that had a p-value of less than 0.2 were incorporated into the multivariate analysis.
- Ethical Considerations
- Ethical approval for Riskesdas 2018 was granted by the Ethical Committee of Health Research, National Institute of Health Research and Development, Ministry of Health, Republic of Indonesia, under the reference number LB.02.01/2/KE.267/2017 [11].
Materials and Methods
Population
Data collection
Variables
Explanatory
- Table 1 illustrates the distribution of diabetes in Indonesia, both as a standalone condition and in conjunction with other diseases. Of the total, 4,652 cases (52.2%) were of diabetes alone, while 4,265 cases (47.8%) involved diabetes with co-existing disease conditions. The 3 most prevalent co-existing conditions were all cardiovascular-related diseases: 17.0% of cases involved diabetes with hypertension, 6.2% involved diabetes with hypertension and other conditions, and 2.5% involved diabetes with heart diseases. In terms of chronic diseases co-existing with diabetes, the highest prevalence was seen in cases of diabetes with rheumatic diseases at 9.1%, followed by diabetes with asthma at 1.8%, and diabetes with cancer at 0.3%.
- Table 2 presents the demographic data of the participants. The majority, 5,253 (58.9%), resided in urban areas. There were 5,248 participants (58.9%) in the age group of 50 to 59 years old. Females constituted a significant portion of the participants, with 5,590 (62.7%) in total. Regarding education, 5,407 (60.6%) had not completed high school. Most of the participants were married, with a total of 7,773 (87.2%). Additionally, 5,768 (64.7%) of the participants were employed.
- Among the participants with diabetes, 1,631 individuals, or 18.3%, exhibited psychiatric disturbances. The socioeconomic factors associated with these disturbances included living in urban areas (crude odds ratio [cOR], 0.69), being between the ages of 50 and 59 (cOR, 0.83), and being unemployed (cOR, 1.73). Conversely, the risk of psychiatric disturbances was higher for female participants (cOR, 1.77), single individuals (cOR, 1.65), and those who did not complete high school (cOR, 2.28). Diabetes combined with other chronic diseases displayed an increasing association with psychiatric disturbances. This was observed in cases of diabetes with rheumatic conditions (cOR, 1.81), diabetes with asthma (cOR, 1.90), and diabetes with cancer (cOR, 2.09). The association was even stronger when diabetes was combined with 1 or more of these conditions: rheumatic conditions, asthma, or cancer (cOR, 4.47). The strongest association was found in cases of diabetes, hypertension, and heart disease, combined with a variety of rheumatic conditions, asthma, and/or cancer (cOR, 6.40) (Table 2).
- Table 3 illustrates the adjusted ORs (aORs) of the associations of sociodemographic characteristics, diabetes, and co-existing disease conditions with psychiatric disturbances among individuals with diabetes. This table presents the same pattern as depicted in Table 2, but with a different degree of influence.
Results
- Prior research has consistently shown that when individuals with diabetes and/or hypertension also exhibit depression, they tend to exhibit decreased self-care practices, diminished adherence to treatment, less than optimal glycemic control, heightened complication rates, increased healthcare costs, reduced quality of life, and higher mortality rates. Unfortunately, many individuals within these populations who have undiagnosed depression do not receive the requisite treatment [15–17].
- The relationship between psychiatric disturbances and chronic diseases such as diabetes is mutually influential. Psychiatric disturbances can exacerbate the conditions of individuals with diabetes, and conversely, diabetes can intensify psychiatric disturbances, impacting overall well-being [18]. In this context, “diabetic distress” is defined as the emotional response marked by fear, discomfort, or disappointment that arises from the perceived inability to effectively manage the challenges of living with diabetes [19]. Our analysis revealed that among Indonesians aged 30 to 59 (387,542 respondents), the prevalence of psychiatric disturbances was 8.5%, while the prevalence of diagnosed diabetes was 2.3% (Figure 1). Furthermore, nearly 18.3% of diabetes patients (8,917 respondents) displayed symptoms of nonspecific psychological distress indicative of psychiatric disturbances.
- Our findings did not reveal a significant impact of age on the incidence of psychiatric disturbances. It is possible that older adults have already developed coping mechanisms and resources, unlike their younger counterparts who are still grappling with various challenges [20]. Our study also found that women were 1.21 times more likely to experience psychiatric disturbances than men. This finding is consistent with the research by Deischinger et al. [21], which suggests that major depressive disorder is more prevalent in women, especially those between the ages of 40 and 49. The higher incidence of psychiatric disturbances in women could be due to biological factors and psychological burdens. Conversely, men may be less likely to openly express depressive symptoms [21]. In the case of patients with diabetes, those with co-existing disease conditions were more common among younger individuals, females, and single individuals. These individuals had a 1.51 times higher risk compared to married individuals. Furthermore, individuals with lower education levels had a 1.91 times higher risk than those with higher education. These findings align with the 2018 Canadian clinical practice guideline, which identifies risk factors for developing diabetes distress. These risk factors include being younger, being female, having a lower level of education, and living alone [22].
- Our study revealed that the incidence of psychiatric disturbances in individuals with both diabetes and hypertension was 1.42 times greater than in those with only diabetes and no comorbidities. AlKhathami et al. [23] found a high prevalence of depression and anxiety in patients with diabetes and/or hypertension, with these mental health disorders affecting 57.3% of the 368 participants. The participants had an average age of 50.9±11.7 years. Among those diagnosed with depression, 39.8% exhibited mild symptoms, 7.1% showed moderate symptoms, and 1.8% displayed severe symptoms. In terms of anxiety, 25.1% had mild symptoms, 8.8% had moderate symptoms, and 4.4% had severe symptoms. The simultaneous presence of depression and anxiety was noted in 29.5% of the participants. Sleep disturbances, weight fluctuations, and low income were identified as significant independent predictors of depression and anxiety [23]. Fisher et al. [24] conducted a study that showed a common association between a combination of depression, anxiety, and other psychological distress with type 2 diabetes.
- Our analysis indicated that individuals with diabetes who also have co-existing conditions such as hypertension, heart disease, rheumatic disease, asthma, or cancer are at the highest risk of experiencing psychiatric disturbances. The OR was significantly high at 6.67 (95% confidence interval [CI], 4.48−9.93; p<0.001) compared to those with diabetes alone. This finding aligns with a previous study by Widakdo and Besral [18], which established a statistically significant relationship between psychological stress and diabetes, along with other chronic diseases, with an OR of 1.6 (95% CI, 1.5−1.7). However, their study did not provide a detailed breakdown of co-existing diseases within the diabetic population, which could account for the lower OR observed in comparison to our study.
- We noted that the risk correlation between diabetes and concurrent heart disease on psychiatric disturbances did not statistically differ from that of diabetic individuals without co-existing diseases (p=0.24). This comparable risk could be due to our study not distinguishing the type of psychiatric disturbance, such as depression, anxiety, or neuroticism. Hu et al. [25] reported similar findings, stating that the cause of mental disorders in patients with coronary artery disease (CAD) and diabetes remains unclear. There was no definitive causal link between CAD and anxiety or neuroticism in patients with diabetes. Given these findings, healthcare providers should prioritize mental health treatments to prevent CAD in patients with diabetes [25]. The disruption of cortisol, a stress hormone, is associated with both short-term and long-term stress factors [26]. Inflammation is another potential biological mechanism that links psychosocial factors to cardiovascular disease and diabetes. Individuals under high levels of psychosocial stress often show increased concentrations of inflammatory cytokines [27].
- Our research suggests that individuals who have both diabetes and rheumatic conditions are 1.75 times more likely to experience psychiatric disturbances compared to those who only have diabetes and no co-existing diseases. This observation is consistent with the study conducted by Nazarinasab et al. [28], which discovered that individuals suffering from both knee osteoarthritis (OA) and diabetes experience more severe pain and higher incidences of physical and mental health disorders than those without diabetes. The linear regression models used in the study further established that diabetes, independent of other factors such as higher body mass index and the severity of radiographic OA, is a risk factor for increased pain [28].
- In addition, our analysis revealed that individuals with both diabetes and asthma had a 1.81-fold higher risk of psychiatric disturbances than those who had diabetes but did not have any co-existing diseases. It is important to note that diabetes is associated with an increased risk of schizophrenia and type 2 diabetes, which in turn further escalates the risk of cardiovascular complications and reduces life expectancy.
- Imbalances in Ca2+ signaling may establish a link between these diseases and the cAMP signaling pathways. Both the Ca2+ and cAMP signaling pathways play a role in regulating the release of neurotransmitters and hormones, as well as controlling the contractility of airway smooth muscles. Any disruptions in these cellular processes could potentially contribute to the dysregulation observed in these diseases [29].
- In this study, the incidence of psychiatric disturbances in individuals with both diabetes and cancer was not significantly different from those with diabetes alone. The risk of psychiatric disturbances in individuals with both diabetes and cancer was represented by an OR of 2.23, but this association was not statistically significant. This could be due to the fact that the study did not differentiate between types of cancer. Furthermore, the number of individuals with both diabetes and cancer was relatively small, which may have contributed to the unstable association observed in our analysis due to the limited number of cases. The research of Vissers et al. [30] suggests that individuals diagnosed with both cancer and diabetes tend to have a poorer health-related quality of life compared to those diagnosed with either disease alone. Other studies have proposed that patient empowerment and self-management strategies can help to lessen the impact of these conditions on patient-reported outcomes, such as depression [30].
- Individuals who have diabetes and multiple concurrent diseases may experience more severe psychiatric disturbances than those with diabetes and fewer co-existing conditions. For instance, the combination of diabetes, hypertension, heart disease, and other conditions was more significant than just diabetes, hypertension, and heart disease, with an aOR of 6.67 (95% CI, 4.48−9.93). However, it is crucial to consider other factors such as the duration of the illness, the quality of sleep, family income, and specific types of psychiatric disturbances. These factors also impact cognitive and emotional disorders.
- Diagnosing psychiatric disorders in individuals with diabetes often presents a challenge due to the absence of specific guidelines for screening and diagnosis within the healthcare system. This leads to a frequent underdiagnosis of psychiatric disturbances in patients with diabetes [31]. In India, data on the prevalence of non-communicable diseases (NCDs) and psychiatric disturbances are limited. Rajan et al. [32] found that anxiety disorders and depression were present in 3.9% to 44.0% and 8.0% to 46.0% of individuals with NCDs, respectively. These mental health issues were strongly associated with poor quality of life, overall health status, and physical function. Therefore, it is crucial to focus on integrated healthcare approaches to improve the screening and identification of NCDs and psychiatric disturbances [32].
- Depression, anxiety, and schizophrenia are commonly observed in individuals with diabetes. These observations underscore the importance of addressing mental health issues within the realm of diabetes care. This is particularly crucial for those with co-existing disease conditions. Providing such information would be beneficial for local policymakers.
- Effective diabetes management should engage patients in modifying their lifestyle, monitoring their condition independently, and adhering to prescribed medication. The diagnosis and treatment of mental disorders represent critical elements of diabetes therapy. This is because addressing both physical and psychological health components is vital for providing comprehensive care [33].
- After accounting for sociodemographic factors, our analysis suggests that individuals with uncomplicated diabetes or any co-existing diseases exhibit the lowest risk of developing psychiatric disturbances. While the relationship between diabetes and psychiatric disturbances remains uncertain, community health studies have reported a higher prevalence of psychiatric disturbances among individuals with diabetes compared to those without diabetes. Psychiatric disturbances in patients with diabetes can impede treatment adherence and deteriorate treatment outcomes [34].
- At the national level, the Indonesian government has enacted the GERMAS program, a healthy lifestyle movement initiated by Indonesian Ministry of Health. This policy intervention aims to prevent and identify NCDs at an early stage. However, there is a current deficiency in mental health interventions for individuals diagnosed with NCDs, including diabetes, within Indonesia. The WHO advocates for the personalization of mental health services for patients with NCDs. This includes conducting mental health screenings for those with diabetes and managing NCDs as a whole [35].
- Under the Indonesian Universal Health Insurance (Jaminan Kesehatan Nasional), the management of NCDs is a critical performance indicator with a focus on prevention. Regular screening programs for prevalent NCDs, including blood pressure checks and glucose tests for diabetes, are carried out in primary care environments via initiatives such as Posbindu, program initiated by Indonesian Ministry of Health, which aim for early detection and treatment. Nonetheless, the success of these programs is dependent on the resources and capabilities available in each district.
- Our analysis reveals varying risk associations of psychiatric disturbances in patients with diabetes, contingent upon their concurrent diseases and demographic traits. This underscores the necessity of customizing mental health services for individuals with diabetes, considering their demographic attributes and comorbidities. In the holistic healthcare management of type 2 diabetes, specific strategies for the early identification and treatment of psychiatric disturbances should be incorporated to lessen their effect on health outcomes [36].
Discussion
- Patients with diabetes who also have multiple diseases seem to exhibit a higher prevalence of mental disorders. Beyond the presence of co-existing diseases, several sociodemographic factors appear to influence the occurrence of cognitive and emotional disorders in individuals with diabetes. These factors include residing in rural areas, being female, being unmarried, having a lower level of education, and being unemployed.
- Recommendation
- These findings underscore the necessity of customizing mental health services within diabetic treatment plans, which should involve both health policymakers and specialists. The Indonesian government, in collaboration with internal medicine organizations, has implemented several programs to manage diabetes. These programs include promoting a healthy lifestyle and diet as preventative measures.
- Given that psychiatric disturbances can exacerbate treatment adherence and self-care issues among individuals with diabetes, it is crucial for healthcare providers and facilities to implement mental health screenings and support systems. Additionally, promoting mental health literacy among patients with diabetes and other NCDs can help prevent treatment non-compliance, which can lead to complications, and minimize stigmatization. It is now necessary for Indonesian healthcare providers to conduct psychiatric disturbance assessments in diabetes patients using the SRQ in primary care settings (Posbindu) and community health centers (Puskesmas). Integrated management for conditions such as diabetes, hypertension, asthma, arthritis, cancer, and others may aid in delaying or preventing the onset of diseases and mental disorders.
- Strengths and Limitations
- One advantage of our analysis is that it is grounded in the Indonesian NHS. The findings provide a comprehensive picture of the health status of Indonesians. Our analysis further dissects diabetes into specific comorbidities, thereby representing the range of comorbidities experienced by Indonesians with diabetes. The results indicate a significantly increased risk of psychiatric disturbances among Indonesian diabetes patients who have multiple chronic diseases. This insight prompts the Indonesian health system and practitioners to consider the integration of mental health services for patients with diabetes.
- A limitation of this study was that the information collected during the interviews was not derived from medical examinations, but rather depended on self-reported data. Despite our specific inquiries about whether a medical doctor had ever diagnosed the participants, some respondents may have either forgotten or been unaware of their diagnosis. It is crucial to acknowledge that the significant attrition of subjects with stroke or cancer could potentially introduce bias into our findings. Although our analytical approach does not permit us to make causal assertions, the fundamental assumption of our study was that various aspects of diabetes status could impact mental health status. Conversely, it is also conceivable that the relationship between psychiatric disturbances and diabetes with chronic diseases could operate in the reverse direction. That is to say, issues with psychiatric disturbances could contribute to the onset of diabetes with co-existing diseases. The data regarding diabetes and its co-existing conditions were gathered through the question, “Have you ever been diagnosed by a doctor?” Some respondents may need to recall or comprehend the medical term used, especially if a local term for the disease exists. Moreover, the estimates could be underreported, particularly in rural or remote areas and regions with limited resources, where access to doctors is often restricted to larger urban cities.
Conclusion
- • An interdependent relationship exists between diabetes and psychiatric disturbances. The presence of diabetes can exacerbate psychiatric disturbances, and vice versa.
- • We discovered that the risk associated with psychiatric disturbances was aggravated when diabetes co-existed with cardiovascular diseases and other chronic conditions.
- • It is essential to conduct screenings for psychiatric disturbances in patients with diabetes, especially those with co-existing diseases. These screenings should be performed using the 20-question self-reporting questionnaire tool in primary care settings (Posbindu) and community health centers (Puskesmas), as psychiatric disturbances can worsen treatment adherence and self-care.
HIGHLIGHTS
Supplementary Material
Supplementary Material 1.
-
Ethics Approval
Ethical approval for Riskesdas 2018 was granted by the Ethical Committee of Health Research, National Institute of Health Research and Development, Ministry of Health, Republic of Indonesia, under the reference number LB.02.01/2/KE.267/2017.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
This published article and its supplementary files include all data generated or analyzed during this study. The data that support the findings of this study can be obtained from the Data Management Laboratory of the National Institute of Health Research and Development (NIHRD), which is a part of the Ministry of Health of Indonesia. The data will be made available upon approval of a written request to the Data Management Laboratory—NIHRD at the following email address: datin.bkpk@kemkes.go.id.
-
Authors’ Contributions
Conceptualization: SI, BR, LKM; Data curation: all authors; Formal analysis: SI, BR, ST; Investigation: all authors; Methodology: SI, ST; Supervision: all authors; Validation: all authors; Visualization: ST; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Article information
-
Acknowledgements
- The authors would like to express our gratitude to Aliza Hunt, MA, for her assistance in refining the English language and contributing to the analysis in this manuscript. We also extend our gratitude to the technical staff from the Data Management Laboratory of NIHRD, Ministry of Health, Indonesia, and other individuals who facilitated the realization of this research.
- 1. Sunny AK, Khanal VK, Sah RB, et al. Depression among people living with type 2 diabetes in an urbanizing community of Nepal. PLoS One 2019;14:e0218119.ArticlePubMedPMC
- 2. Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep 2020;10:14790. ArticlePubMedPMCPDF
- 3. Mboi N, Murty Surbakti I, Trihandini I, et al. On the road to universal health care in Indonesia, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018;392:581−91.ArticlePubMedPMC
- 4. Jung A, Du Y, Nubel J, et al. Are depressive symptoms associated with quality of care in diabetes?: findings from a nationwide population-based study. BMJ Open Diabetes Res Care 2021;9:e001804.ArticlePubMedPMC
- 5. Herrman H, Kieling C, McGorry P, et al. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet 2019;393:e42−3.ArticlePubMed
- 6. Chireh B, Li M, D’Arcy C. Diabetes increases the risk of depression: a systematic review, meta-analysis and estimates of population attributable fractions based on prospective studies. Prev Med Rep 2019;14:100822. ArticlePubMedPMC
- 7. Wright J, Mazumdar P, Barua D, et al. Integrating depression care within NCD provision in Bangladesh and Pakistan: a qualitative study. Int J Ment Health Syst 2020;14:63. ArticlePubMedPMCPDF
- 8. Verma M, Grover S, Tripathy JP, et al. Co-existing non-communicable diseases and mental illnesses amongst the elderly in Punjab, India. Eur Endocrinol 2019;15:106−12.ArticlePubMedPMC
- 9. Arifin B, van Asselt AD, Setiawan D, et al. Diabetes distress in Indonesian patients with type 2 diabetes: a comparison between primary and tertiary care. BMC Health Serv Res 2019;19:773. ArticlePubMedPMCPDF
- 10. Arifin B, Probandari A, Purba AK, et al. ‘Diabetes is a gift from god’: a qualitative study coping with diabetes distress by Indonesian outpatients. Qual Life Res 2020;29:109−25.ArticlePubMedPDF
- 11. Indonesian Ministry of Health. Report of national community health survey 2018. Indonesian Ministry of Health; 2019. Indonesian.
- 12. Idaiani S, Indrawati L. Functional status in relation to depression among elderly individuals in Indonesia: a cross-sectional analysis of the Indonesian National Health Survey 2018 among elderly individuals. BMC Public Health 2021;21:2332. ArticlePubMedPMCPDF
- 13. Beusenberg M, Orley J. A user’s guide to the self reporting questionnaire. World Health Organization; 1994. p 84.
- 14. Idaiani S, Suryaputri IY, Mubasyiroh R, et al. Validity of the Self Reporting Questionnaire-20 for depression based on National Health Survey [Preprint]. Posted 2021 Mar 26. Res Sq https://doi.org/10.21203/rs.3.rs-362342/v1.Article
- 15. van Bastelaar KM, Pouwer F, Geelhoed-Duijvestijn PH, et al. Diabetes-specific emotional distress mediates the association between depressive symptoms and glycaemic control in Type 1 and Type 2 diabetes. Diabet Med 2010;27:798−803.ArticlePubMed
- 16. Udedi M, Pence BW, Stewart RC, et al. Detection and prevalence of depression among adult type 2 diabetes mellitus patients attending non-communicable diseases clinics in Lilongwe, Malawi. Int J Ment Health Syst 2020;14:79. ArticlePubMedPMCPDF
- 17. Valladares-Garrido MJ, Soriano-Moreno AN, Rodrigo-Gallardo PK, et al. Depression among Peruvian adults with hypertension and diabetes: analysis of a national survey. Diabetes Metab Syndr 2020;14:141−6.ArticlePubMed
- 18. Widakdo G, Besral B. The effect of chronic illness on mental emotional disorder. Kesmas Natl Public Heal J 2013;7:309−16. Indonesian.
- 19. Kamrul-Hasan AB, Hannan MA, Asaduzzaman M, et al. Prevalence and predictors of diabetes distress among adults with type 2 diabetes mellitus: a facility-based cross-sectional study of Bangladesh. BMC Endocr Disord 2022;22:28. ArticlePubMedPMCPDF
- 20. Boehm JK, Trudel-Fitzgerald C, Kivimaki M, et al. The prospective association between positive psychological well-being and diabetes. Health Psychol 2015;34:1013−21.ArticlePubMedPMC
- 21. Deischinger C, Dervic E, Leutner M, et al. Diabetes mellitus is associated with a higher risk for major depressive disorder in women than in men. BMJ Open Diabetes Res Care 2020;8:e001430.ArticlePubMedPMC
- 22. Robinson DJ, Coons M, Haensel H, et al. Diabetes and mental health. Diabetes Canada Clinical Practice Guidelines Expert Committee. Can J Diabetes 2018;42 Suppl 1:S130−41.Article
- 23. AlKhathami AD, Alamin MA, Alqahtani AM, et al. Depression and anxiety among hypertensive and diabetic primary health care patients: could patients’ perception of their diseases control be used as a screening tool? Saudi Med J 2017;38:621−8.PubMedPMC
- 24. Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care 2007;30:542−8.ArticlePubMedPDF
- 25. Hu T, Yang F, He K, et al. Association of mental health with the risk of coronary artery disease in patients with diabetes: a mendelian randomization study. Nutr Metab Cardiovasc Dis 2022;32:703−9.ArticlePubMed
- 26. Adam EK, Hawkley LC, Kudielka BM, et al. Day-to-day dynamics of experience: cortisol associations in a population-based sample of older adults. Proc Natl Acad Sci U S A 2006;103:17058−63.ArticlePubMedPMC
- 27. Hansel A, Hong S, Camara RJ, et al. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci Biobehav Rev 2010;35:115−21.ArticlePubMed
- 28. Nazarinasab M, Motamedfar A, Moqadam AE. Investigating mental health in patients with osteoarthritis and its relationship with some clinical and demographic factors. Reumatologia 2017;55:183−8.ArticlePubMedPMCPDF
- 29. Bergantin LB. A link among schizophrenia, diabetes, and asthma: role of Ca2+cAMP signaling. Brain Circ 2020;6:145−51.ArticlePubMedPMC
- 30. Vissers PA, Falzon L, van de Poll-Franse LV, et al. The impact of having both cancer and diabetes on patient-reported outcomes: a systematic review and directions for future research. J Cancer Surviv 2016;10:406−15.ArticlePubMedPDF
- 31. Espinoza D, Sanchez PA, Junia C. Diabetes mellitus: an unrecognized complication in the management of patients with mental illness. Cureus 2020;12:e8444.ArticlePubMedPMC
- 32. Rajan S, Krishna A, Muliyala KP, et al. Comorbidity of anxiety and depression with hypertension, diabetes, and cardiovascular disease: a selective systematic review from India. EMJ Diabet 2022;10:83−94.Article
- 33. Akhaury K, Chaware S. Relation between diabetes and psychiatric disorders. Cureus 2022;14:e30733.ArticlePubMedPMC
- 34. Holt RI, de Groot M, Golden SH. Diabetes and depression. Curr Diab Rep 2014;14:491. ArticlePubMedPMCPDF
- 35. Ngo VK, Rubinstein A, Ganju V, et al. Grand challenges: integrating mental health care into the non-communicable disease agenda. PLoS Med 2013;10:e1001443.ArticlePubMedPMC
- 36. Guerrero Fernandez de Alba I, Gimeno-Miguel A, Poblador-Plou B, et al. Association between mental health comorbidity and health outcomes in type 2 diabetes mellitus patients. Sci Rep 2020;10:19583. ArticlePubMedPMCPDF
References
Figure & Data
References
Citations

- Correction to “The risk associated with psychiatric disturbances in patients with diabetes in Indonesia (2018): a cross-sectional observational study” [Osong Public Health Res Perspect 2023;14(5):368–78]
Siti Isfandari, Betty Roosihermiatie, Sulistyowati Tuminah, Laurentia Konadi Mihardja
Osong Public Health and Research Perspectives.2023; 14(6): 530. CrossRef


 Cite
Cite