Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 14(1); 2023 > Article
-
Original Article
Association between face covering policies and the incidence of coronavirus disease 2019 in European countries -
Sookhyun Kim
 , Jiyoung Oh
, Jiyoung Oh , Sangwoo Tak
, Sangwoo Tak
-
Osong Public Health and Research Perspectives 2023;14(1):31-39.
DOI: https://doi.org/10.24171/j.phrp.2022.0287
Published online: February 1, 2023
Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Korea
- Corresponding author: Sangwoo Tak Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Korea E-mail: taksw@korea.kr
© 2023 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
- 2,032 Views
- 73 Download
Abstract
-
Objectives
- This study was conducted to determine the impact of the strengthening or relaxation of face covering mandates on the subsequent national case incidence of coronavirus disease 2019 (COVID-19) in Europe as the full vaccination rate was increasing.
-
Methods
- European countries in which case incidence increased for 3 consecutive weeks were monitored and analyzed using COVID-19 incidence data shared by the World Health Organization (WHO). The epidemic trend of COVID-19 in Europe was compared with that of countries elsewhere in the world based on WHO weekly epidemiological reports from June 20 to October 30, 2021. In addition, this study provided insight into the impact of government mask mandates on COVID-19 incidence in Europe by measuring the index scores of those facial covering policies before and after mandate relaxation or strengthening. The effects of the vaccination rate and the speed of vaccination on COVID-19 incidence were also analyzed.
-
Results
- The incidence of COVID-19 after the relaxation of face covering mandates was significantly higher than before relaxation. However, no significant difference was observed in vaccination rate between countries with increased and decreased incidence. Instead, rapid vaccination delayed the resurgence in incidence.
-
Conclusion
- The findings suggest that face covering policies in conjunction with rapid vaccination efforts are essential to help mitigate the spread of COVID-19.
- The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for coronavirus disease 2019 (COVID-19) first identified in Wuhan, China in December 2019, led to a global pandemic [1]. By October 2021, the COVID-19 pandemic was in its second year in Europe, which had again become the center of the global epidemic. Although over 2.8 million COVID-19 cases were reported in the week of October 4–10, 2021, the weekly number of new cases reported globally had continued to decline since late August 2021 after increasing for nearly 2 months since mid-June 2021 [2]. While the incidence of COVID-19 cases was decreasing globally, Europe had experienced a plateau in incidence starting at the end of July 2021; then, in the third week of September, the number of new cases began to increase, with European countries accounting for most of those with increased incidence for the third consecutive week [2,3]. Over half of the European countries (42 of 61, 68.9%) exhibited an increase in the number of new cases during the week of October 18–24, accounting for more than half (57%) of the weekly new cases worldwide and making Europe the only world region reporting an increase in cases [4]. According to some studies, the spread of COVID-19 increased not only in Russia and eastern Europe, where vaccine coverage is significantly lower than elsewhere, but also in European countries with high vaccination rates that implemented “living with COVID-19” strategies (most notably, removing some requirements for facial coverings) [5,6].
- Although vaccinated individuals appear to be well protected against serious symptoms [7], vaccination has little effect on the disruption of the infection chain necessary to restrain the epidemic [8]. Moreover, achieving high coverage is difficult given the complexity of large-scale vaccine production, distribution, and uptake [7]. This indicates a need to continue with non-pharmacological interventions (NPIs), such as physical distancing and wearing face coverings, as long as a substantial proportion of individuals remain unvaccinated [9,10]. As the emergence of variants and the weakening of immunity can also reduce vaccine effectiveness [7,8], the prevention of new infections is limited even in countries with high vaccination rates. One study on the resurgence of COVID-19 in a highly vaccinated healthcare workforce emphasized that the rapid reintroduction of NPIs, including the wearing of face coverings indoors, can counter the rapid spread of a new viral variant [11]. Moreover, many children have not yet been vaccinated, and young children are not required to wear face coverings in numerous countries [12]. This suggests that government countermeasures, such as the compulsory wearing of face coverings even for vaccinated adults, are required. Many countries have increased compliance with mask-wearing by strengthening mandates in various settings [13]. An analysis showed that these laws and regulations were effective in raising compliance with mask-wearing and delaying the spread of COVID-19 [14,15]. In many studies on the impact of face coverings on virus transmission, the period of mandatory masking has been used for analysis [16]. At the start of the 2021–2022 school year, in the 2 largest counties of the United States (US) state of Arizona, schools with a face covering mandate were 3.5 times less likely to experience a school-related COVID-19 outbreak than schools without one [17].
- As vaccination rates improve, demand is increasing to relax COVID-19 guidelines, despite most of the populations in question remaining susceptible [18]. In 2021, the rate of mask-wearing declined significantly worldwide, including in countries with low vaccination rates [16]. However, due to the risk of another wave of infections, the appropriate time to lift quarantine restrictions remains uncertain [18]. Recent mathematical modeling indicates that if NPIs are relaxed too early—before immunity has been fully established—a large outbreak may occur, resulting in hospitalization and death [1]. Although an abrupt weakening of NPIs may result in a similar number of deaths as a prolonged infection wave under a gradual relaxation of NPIs, a more extended infection period with a smaller outbreak provides a much greater chance for future interventions to be effective and reduces stress on the health care system [1].
- Given the ongoing epidemic, we must evaluate the effectiveness of mask-wearing after some immunization progress has been achieved [19]. Although evidence for the effective impact of face coverings on COVID-19 transmission has accumulated at the individual level, the additional benefit of national mandates is less certain. We focused on the impact of the legal requirement to wear a face covering on the national weekly case incidence of the disease by analyzing the strength of government masking policies in European countries. In this study, we aimed to analyze the association between the strength of face covering mandates and national COVID-19 case incidence by quantifying the government policy indicators of such mandates and the trend of vaccination rates in European countries. In addition, we attempted to assess whether the protective effect of vaccination and masking mandates could reduce COVID-19 case incidence at the national level.
Introduction
- The study targeted 25 European countries with an increase in COVID-19 cases for 3 consecutive weeks between September 19 and October 30, 2021 (Russia, Ukraine, Romania, Bulgaria, Republic of Moldova, Georgia, Belarus, Poland, Czech Republic, Austria, Denmark, Lithuania, Estonia, Latvia, the Netherlands, Belgium, Greece, France, Germany, Portugal, Azerbaijan, Norway, Turkey, Hungary, and Ireland) and 10 countries with a decrease or no increase in cases for 3 consecutive weeks (Italy, Spain, Sweden, Switzerland, Slovenia, Albania, Serbia, Bosnia and Herzegovina, Croatia, and Cyprus). The number of weekly confirmed cases by country was calculated based on the new daily COVID-19 incidence data shared by the WHO, and countries in which the number of cases increased for 3 consecutive weeks were monitored. In addition, WHO weekly epidemiological reporting was used to compare the trend of the COVID-19 outbreak between Europe and other world regions. The data collection period was from June 20, 2021 (when the number of new cases and countries with increasing COVID-19 cases for 3 consecutive weeks began to increase simultaneously) to October 30, 2021, before the first case of the Omicron variant was reported in Europe.
- The government response regarding mandatory masking was quantified using the facial coverings section corresponding to the health system among the 23 policy indicators of governmental COVID-19 response. These indicators were presented by the Oxford COVID-19 Government Response Tracker of the Blavatnik School of Government at Oxford University in the United Kingdom. Based on rules regarding the use of facial coverings outside the home, government policies were scored as 0 (no policy), 1 (recommended), 2 (required in some specified shared/public spaces outside the home with other people present or some situations in which social distancing was not possible), 3 (required in all shared/public spaces outside the home with other people present or all situations in which social distancing was not possible), or 4 (required outside the home at all times regardless of location or presence of other people). We calculated the average vaccination rate over 2 weeks to investigate any difference in incidence or case growth rate based on the rate of fully vaccinated people by country. A US Centers for Disease Control and Prevention (CDC) study indicated that about 2 weeks are required after vaccination for the body to produce antibodies that protect against infection. That study also showed that the risk of infection is reduced by 90% following the second dose of vaccine [20]. In the present study, national vaccination rates were classified as 0 (<40%), 1 (≥40% and <60%), or 2 (≥60%) based on the number of fully vaccinated people provided by Our World in Data. Incidence refers to the number of weekly new COVID-19 cases per 100,000 people in each country.
- We analyzed the correlations among the incidence or growth rate in COVID-19 cases, the strengthening or relaxation of face covering policies, and the vaccination rate. Regarding face coverings, we investigated whether the mandates were relaxed at least once along with the index scores of those facial covering policies during the 7 weeks immediately prior to the start of the increase in cases. One study showed that new COVID-19 cases peaked 45 days after the lifting of masking mandates [21]. Thus, changes in face covering policies and the associated index scores were observed for 7 weeks. In addition, the t-test was conducted for the incidence and the case growth rate before and after the mandatory wearing of face coverings was eased or strengthened. The index scores of the facial covering policies and vaccination rates were also analyzed using t-testing for the 25 countries in which the incidence increased for 3 consecutive weeks and the 10 countries in which incidence decreased or did not increase during that period. In a further analysis, we examined the time for 26 countries to reach 40% fully vaccinated by October 30, 2021, along with the amount of time taken for the re-increase in COVID-19 incidence after the 40% vaccination threshold. The basis for the vaccination threshold of 40% was the global COVID-19 vaccination strategy and time-bound coverage target announced by the WHO [22]. The WHO warned that the risk of emergent vaccine-resistant variants may continue if the 40% vaccination target cannot be reached [23]. The International Monetary Fund staff also proposed that at least 40% of the population in all countries should be vaccinated by the end of 2021 to bring the pandemic under control [24]. Thirteen countries (Latvia, France, Portugal, Azerbaijan, Norway, Turkey, Italy, Spain, Sweden, Switzerland, Serbia, Croatia, and Cyprus) began to see a resurgence in incidence within 3 months of achieving 40% vaccination coverage. The other 13 countries, which displayed no increase in disease incidence within 3 months of achieving 40% vaccination coverage, were Poland, Czech Republic, Austria, Denmark, Lithuania, Estonia, Netherlands, Belgium, Greece, Germany, Hungary, Ireland, and Slovenia. Of the 13 countries in which 13 weeks or more elapsed before a re-increase in incidence after a vaccination rate of 40% was achieved, 11 countries (accounting for approximately 42% of the total countries) took 13 weeks, while the rest of the 13 countries took more than 13 weeks. Accordingly, the speed of vaccination was compared between countries reaching 40% before and after 3 months. For countries with 2 or more re-increase periods after achieving 40% vaccination coverage, the re-increase period was defined from the week of the interval including the week with the highest incidence. Analysis of variance was used to evaluate the significance of differences in the average incidence or the case growth rate in the 25 countries according to the average vaccination rate for 2 weeks immediately before the increase in cases for 3 consecutive weeks.
- Statistical Analysis
- All statistical analyses were conducted using Rex ver. 3.6.3 excel-based software (Rexsoft Co.; http://rexsoft.org).
Materials and Methods
- To identify trends in COVID-19 cases, we followed the CDC criteria to monitor weekly changes in the number of cases over a 4-week period by country. The CDC has provided a line graph on a monthly basis to visualize trends in the number of US COVID-19 cases [25]. The average incidence among the 25 countries where the COVID-19 case incidence increased for 3 consecutive weeks was significantly higher than that of the 10 countries where the number of cases decreased or did not increase during that period (Table 1). The correlation between the average incidence or weekly case growth rate per 100,000 population over 4 weeks for countries in which the incidence increased for 3 consecutive weeks and countries that relaxed the mandatory mask-wearing criteria at least once in the 7 weeks immediately before the increase was positive (r=0.339, 0.388) (Tables 2, 3). However, negative correlations (r=−0.204, −0.260) were found between the average incidence during the 4 weeks of increase and the average vaccination rate for the 2 weeks immediately before the increase and during the 4 weeks of increase, respectively (Table 2). Negative correlations were also found individually (r=−0.165, −0.298) between the average case growth rate during the 4 weeks of increase and the average vaccination rate for the 2 weeks immediately before the increase and during the 4 weeks of increase, respectively (Table 3). In addition, the COVID-19 incidence during the 4 weeks after relaxation of mask mandates was significantly higher than that during the 4 weeks before relaxation (Table 4). This finding showed that the implementation of face covering mandates was necessary to prevent the spread of COVID-19 at the national level. The incidence rate in the 2 weeks after reinforcement of mandatory masking policies was higher than in the 2 weeks before reinforcement, while the case growth rate was lower in the 2 weeks after strengthening of masking policies; however, neither change was statistically significant (Table 5). In contrast, no significant difference in average vaccination rate was observed in the 2 weeks immediately before the increase or decrease in incidence between countries with increasing and decreasing incidence (Table 6).
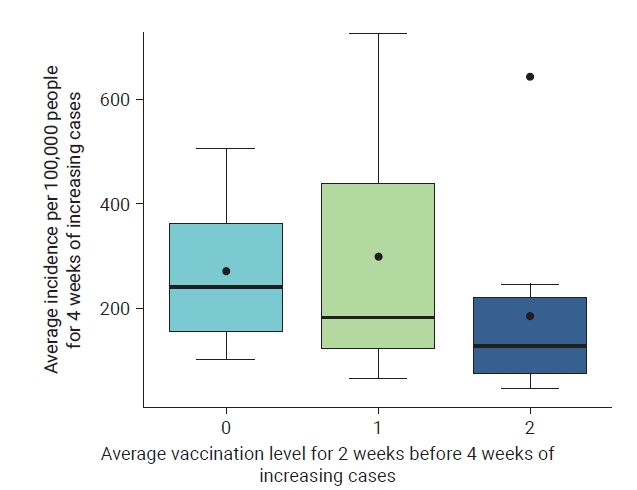
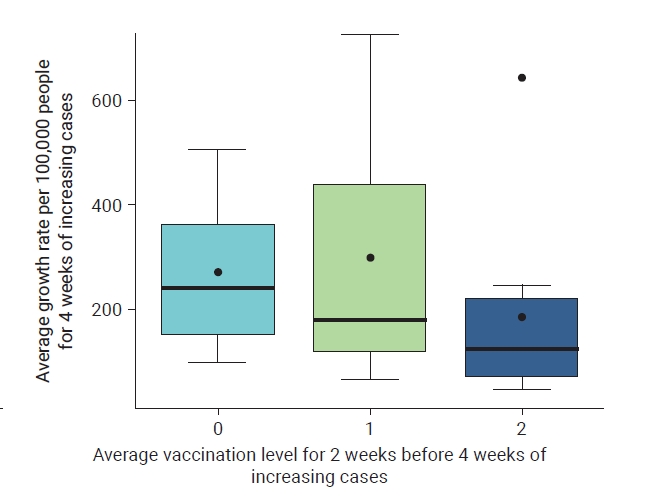
- In addition, countries with an average vaccination rate of 60% or higher for the 2 weeks immediately prior to the 4-week increase showed decreases in the average incidence and case growth rate during the increase compared to countries with vaccination rates at or above 40% and less than 60%, but this was not statistically significant (Figures 1, 2). Furthermore, by analyzing the time taken for the re-increase in incidence after reaching the 40% vaccination threshold and the time to reach a fully vaccinated rate of 40%, we concluded that countries in which the incidence began to increase again after 3 months took significantly less time to reach 40% vaccination than countries where the incidence began to re-increase within 3 months (Table 7).
Results
- This study showed the impact of face covering mandates and vaccination coverage on the incidence of COVID-19 in 35 European countries from June 20 to October 30, 2021. The average COVID-19 case incidence in countries where incidence increased for 3 consecutive weeks was significantly higher than in countries where cases decreased or did not increase during that period (Table 1). Furthermore, relaxation of face covering mandates was associated with an increase in the incidence of COVID-19 (Tables 2–4). Six US states (North Dakota, Iowa, Montana, Texas, Wyoming, and Arkansas) lifted face covering mandates between January and March 2021. As indicated by an event study analysis, daily new cases began to increase within 9 to 15 days after the mandates were lifted, followed by the highest increase (12 cases per 100,000 people) on day 45 [20]. This result implies that policies mandating mask-wearing in public needed to be strengthened, given that some states demanded or initiated the lifting of face covering obligations around that time [21]. We also found an increase in incidence and a decrease in the case growth rate after 2 weeks of reinforcement of face covering mandates, but neither finding was statistically significant (Table 5). The enforcement of mask-wearing may take longer than desired because behavior change reinforcement must disrupt current habits and simultaneously encourage a new and unfamiliar set of behaviors [26]. According to Layyy et al. [27], it takes 18 to 254 days for a person to form a new habit and an average of 66 days for a new behavior to become automatic. COVID-19 incidence may continue to increase in the early stages of strengthening of face covering mandates. Given the decrease in the case growth rate, however, the incidence could also decline over time. One study [28] showed that strengthening of face covering mandates in most or all shared or public places between August 2020 and January 2021 in 114 regions of 8 European countries reduced the reproduction number by 12% (95% confidence interval [CI], 7%–17%). Before the onset of the second wave of infection, these countries had implemented policies that mandated face coverings in only some public places. Thus, the advantage of wearing a face covering is expected to be realized when strengthened masking mandates are implemented [28]. Similarly, a 2% decrease in the growth rate of daily cases, constituting a significant difference, was observed at ≥21 days after masking became compulsory in a natural experiment including 15 US states [14]. In another study, the effectiveness of wearing a face covering was tested using mathematical modeling tools, with the results showing that public masking could considerably slow the spread of COVID-19 and prevent further outbreaks of the disease [29]. These findings demonstrate that face coverings are effective in protecting non-infected face-covering wearers from acquiring the disease and preventing infected wearers from transmitting the disease to others [13,16,30–32]. Therefore, governments must strongly encourage the use of face coverings in various public places using regulations [13].
- In contrast, as seen in Table 6, no significant difference was present in vaccination rates between countries with increasing and decreasing incidence, which indicates that the increase or decrease in COVID-19 incidence may have little correlation with the level of vaccination. In fact, a national-level study revealed no perceptible relationship between the fully vaccinated percentage of the population and new COVID-19 cases across 68 countries [33]. Iceland and Portugal, where more than 75% of the population had been fully vaccinated, had more COVID-19 cases per 1 million people than countries such as Vietnam and South Africa, where about 10% of the population had been fully vaccinated. In the US, 2947 counties also showed no significant decline in COVID-19 cases as the percentage of fully vaccinated population increased [33]. The US CDC identified 4 of the 5 counties with the highest percentage of fully vaccinated population (84.3%–99.9%) as high-transmission counties [33]. Conversely, counties with less than 20% of the population fully vaccinated accounted for 26.3% of the 57 counties classified by the CDC as low-transmission counties. This suggests that NPIs, such as masking, should be implemented as vaccination rate increases [33]. From the end of June 2021, the number of European countries demanding or implementing the relaxation or lifting of face covering mandates has increased [6]. Perhaps people can wear less face coverings with the relief after COVID-19 vaccination [21]. However, a sizable proportion of Europe was vulnerable to infection in July 2021. At that time, just 35% of adults in the Europe and European Economies Area (including Iceland and Norway) were fully vaccinated, and Russia and other former Soviet Union countries had barely reached a 10% vaccination completion rate [6]. In addition, European civil officials appeared reluctant to adopt a culture of mask-wearing, which in Asian countries after the influenza epidemics of 1918, 1957, and 1968 and the SARS-CoV-1 outbreak in 2002 has been prevalent as an effective measure for epidemic containment [6]. The European Centers for Disease Control and Prevention has issued a risk assessment urging strict adherence to public health measures that have previously worked to control the effects of different variants [34]. The WHO has urged “extreme caution” for countries considering lifting COVID-19 restrictions, warning that high vaccination rates will not prevent the growing transmission of the virus [35]. Furthermore, the virus is still evolving and changing, and it is unclear to what extent vaccination provides protection against becoming infected or spreading the virus to others [35]. A recent study re-emphasized the difficulty of controlling the COVID-19 pandemic with vaccination alone [7]. This study also showed that the incidence of the disease increases again upon the cessation of masking when a certain range of vaccination rate has been achieved [7]. This is because reaching a certain vaccination level does not immediately stop the spread of the virus. Alternatively, wearing a face covering could prevent further COVID-19 cases until transmission finally begins to wane after 2 to 10 weeks [7]. Simulation outcomes of another study also suggested that eliminating NPIs (such as movement restriction and mask-wearing) while COVID-19 vaccines are being delivered may considerably increase infections, hospitalizations, and deaths compared to a situation in which NPIs are maintained [36]. These results emphasized that the 2 strategies of increasing the vaccination rate and adhering to sustainable NPIs (such as masking) should be combined to safely return to pre-COVID-19 pandemic conditions [36]. This combination is potentially synergistic because vaccination protects against the disease while face coverings interfere with virus transmission using a physical barrier to any coronavirus variant [8].
- In addition, as shown in Figures 1 and 2, the number of new COVID-19 cases per 100,000 people increased until the countries achieved a vaccination rate of 60% of their total populations, but decreased after reaching 60% vaccination coverage. This result resembles that of a study in which the number of new cases per million people and the reproductive rate of COVID-19 slowly decreased as the vaccination rate increased, with a marked decrease when the vaccination rate exceeded 60% [37]. However, as of August 20, 2021, COVID-19 vaccination rates had not reached 60% on any continent, meaning that the vaccination rates were too low to prevent disease transmission [37]. In addition, this study showed that the faster a certain vaccination level was reached, the longer it took for the incidence to re-increase (Table 7). The results indicate that a rapid rise in the COVID-19 vaccination rate attenuates the intensity of the epidemic, extending the time to prepare for a resurgence. A scenario analysis by Wang et al. [38] in 2022 showed that accelerating the vaccination speed in the early stages of a vaccination campaign can reduce infections and increase vaccine effectiveness. In a scenario involving a doubled speed of vaccination, the vaccine effectiveness increased to 77.5% (95% CI, 29.2%–93.6%), averting an additional 1.71 million cases. By contrast, when the vaccination speed was halved, predicted vaccination effectiveness declined to 43.7% (95% CI, 9.34%–70.2%), with 2.55 million more infections. Therefore, the speed of vaccination from the beginning of the vaccination campaign is crucial, given the spread of new COVID-19 variants and the need for booster shots [38]. The simulation model of another study showed that reaching 80% vaccination while maintaining masking could avoid 7.66 million SARS-CoV-2 cases [7]. However, achieving this same range 2 months later could prevent 8.57 million cases. These results emphasize the need for continued adherence to masking in addition to the rapid implementation of vaccination.
- This study has several limitations. During the re-spreading of COVID-19 in Europe, a confirmed European case of the Omicron variant was reported, limiting the extension of the study period. Moreover, it was difficult to measure the independent impact of mandatory masking because European countries implemented multi-layered infection prevention and control measures, and this study examined COVID-19 incidence only at the national level. Lastly, of the 25 European countries selected for the study, Eastern European countries accounted for 44% (11 countries), or nearly half. This is due to limitations on the availability of the index scores of masking policies and vaccination rate. Thus, assessing the effectiveness of face covering mandates in Europe with more data from other European countries may help generalize our findings.
Discussion
- The hasty easing or lifting of face covering mandates along with increasing vaccination rates has resulted in a resurgence of COVID-19 infection in European countries. Not all countries on the same continent can vaccinate with equal speed, and the effects of masking at the national level may depend on government mandates. Hence, we strongly recommend policymakers proceed cautiously regarding the adjustment of face covering mandates to avoid a resurgence of COVID-19 incidence. Further control of the COVID-19 epidemic at the national level should allow for an effective vaccination campaign. It would also be wise to appropriately plan for effective and sustainable face covering mandates until the vaccination rate reaches a certain level.
Conclusion
-
Ethics Approval
Ethical approval was not required for this study on human participants because the data were accessed from the WHO, Our World in Data, and the Oxford COVID-19 Government Response Tracker (a publicly available database).
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are publicly available.
-
Authors’ Contributions
Conceptualization: ST; Data curation: SK, JO; Formal analysis: SK; Methodology: SK, ST, JO; Project administration: SK; Resources: SK, JO; Visualization: SK; Writing–original draft: SK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Additional Contributions
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Korea Disease Control and Prevention Agency or the institutions with which the authors are affiliated.
Article information
| Group | No. of countries | Incidence* | Index scores of facial covering policies | Vaccination rate |
|---|---|---|---|---|
| Total | 35 | 219.8±199.4 (23.1–898.5) | 2.2±0.8 (0.0–4.0) | 1.2±0.8 (0.0–2.0) |
| High incidencea) | 25 | 244.1±211.6 (27.6–898.5) | 2.2±0.8 (0.0–4.0) | 1.2±0.8 (0.0–2.0) |
| Low incidenceb) | 10 | 158.9±150.7 (23.1–562.8) | 2.2±0.9 (0.0–3.0) | 1.3±0.8 (0.0–2.0) |
| Variable | Average incidence per 100,000 population for 4 weeksa) |
|---|---|
| Average incidence per 100,000 population for 4 weeksa) | 1 |
| Relaxation of mandatory face covering policies at least once for 7 weeksb) | 0.339 |
| Average index scores of facial covering policies | |
| For 7 weeksb) | 0.103 |
| For 4 weeksa) | 0.309 |
| Average vaccination rate | |
| For 2 weeksb | −0.204 |
| For 4 weeksa) | −0.261 |
| Variable | Average growth rate of cases per 100,000 population for 4 weeksa) |
|---|---|
| Average growth rate of cases per 100,000 population for 4 weeksa) | 1 |
| Relaxation of mandatory face covering policies at least once for 7 weeksb) | 388 |
| Average index scores of facial covering policies | |
| For 7 weeksb) | −0.041 |
| For 4 weeksa) | 0.121 |
| Average vaccination rate | |
| For 2 weeksb) | −0.165 |
| For 4 weeksa) | −0.298 |
| Group | No. of countries |
Mean±SD |
Mean difference (95% CI) | |
|---|---|---|---|---|
| Pre | Post | |||
| 4 Weeks* | 11 | 97.0±61.4 | 140.1±132.3 | −43.1 (−84.4 to −1.9) |
| 2 Weeks | 13 | 91.9±59.4 | 129.5±123.3 | −37.6 (−93.7 to 18.4) |
| Variable | No. of countries |
Mean±SD |
Mean difference (95% CI) | |
|---|---|---|---|---|
| Pre | Post | |||
| Incidence | 9 | 173.9±225.1 | 263.1±272.0 | −89.2 (−187.1 to 8.7) |
| Growth rate of cases | 9 | 53.4±67.7 | 9.2±91.6 | 44.3 (−70.3 to 158.8) |
| Variable | High-incidence countries (n=25)a) | Low-incidence countries (n=10)b) |
|---|---|---|
| Average index scores of facial covering policies for 7 weeksc) | 2.5±0.7 | 2.1±0.8 |
| Average vaccination rate for 2 weeksc) | 1.1±0.9 | 1.2±0.8 |
Data are presented as mean±standard deviation.
a) Three consecutive weeks of increasing incidence (between September 19 and October 30, 2021);
b) Three consecutive weeks of decreasing or no increase in incidence (between September 19 and October 30, 2021);
c) Shortly prior to 3 consecutive weeks of increasing or decreasing incidence.
| Variable | Before 3 mo (n=13) | After 3 mo (n=13) | p |
|---|---|---|---|
| Time to reach 40% fully vaccinated (wk)a) | 29.9±3.7 | 26.9±2.0 | <0.05 |
- 1. Moore S, Hill EM, Tildesley MJ, et al. Vaccination and non-pharmaceutical interventions for COVID-19: a mathematical modelling study. Lancet Infect Dis 2021;21:793−802.ArticlePubMedPMC
- 2. World Health Organization (WHO). COVID-19 weekly epidemiological update, edition 61, 13 October 2021 [Internet]. WHO; 2021 [cited 2021 Dec 13]. Available from: https://apps.who.int/iris/handle/10665/346574.
- 3. World Health Organization (WHO). WHO coronavirus (COVID-19) dashboard [Internet]. WHO; 2021 [cited 2021 Dec 17]. Available from: https://covid19.who.int/data.
- 4. World Health Organization (WHO). COVID-19 weekly epidemiological update, edition 63, 26 October 2021 [Internet]. WHO; 2021 [cited 2021 Dec 26]. Available from: https://apps.who.int/iris/handle/10665/347449.
- 5. Mathieu E, Ritchie H, Rodés-Guirao L, et al. Coronavirus pandemic (COVID-19) [Internet]. OurWorldInData.org; 2020 [cited 2023 Jan 11]. Available from: https://ourworldindata.org/covid-vaccinations.
- 6. Europe must open with extreme caution this summer. Lancet Reg Health Eur 2021;6:100176. ArticlePubMedPMC
- 7. Bartsch SM, O'Shea KJ, Chin KL, et al. Maintaining face mask use before and after achieving different COVID-19 vaccination coverage levels: a modelling study. Lancet Public Health 2022;7:e356−65.ArticlePubMedPMC
- 8. Brüssow H, Zuber S. Can a combination of vaccination and face mask wearing contain the COVID-19 pandemic? Microb Biotechnol 2022;15:721−37.ArticlePubMedPDF
- 9. Paltiel AD, Schwartz JL, Zheng A, et al. Clinical outcomes of a COVID-19 vaccine: implementation over efficacy. Health Aff (Millwood) 2021;40:42−52.ArticlePubMed
- 10. Saad-Roy CM, Wagner CE, Baker RE, et al. Immune life history, vaccination, and the dynamics of SARS-CoV-2 over the next 5 years. Science 2020;370:811−8.ArticlePubMedPMC
- 11. Keehner J, Horton LE, Binkin NJ, et al. Resurgence of SARS-CoV-2 Infection in a Highly Vaccinated Health System Workforce. N Engl J Med 2021;385:1330−2.ArticlePubMed
- 12. Joi P. Can we stop wearing masks after being vaccinated? [Internet]. GAVI Vaccines work; 2021 [cited 2021 Dec 10]. Available from: https://www.gavi.org/vaccineswork/can-we-stop-wearing-masks-after-being-vaccinated.
- 13. Howard J, Huang A, Li Z, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A 2020;118:e2014564118.Article
- 14. Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff (Millwood) 2020;39:1419−25.ArticlePubMed
- 15. Hatzius J, Struyven D, Rosenbery I. Face masks and GDP [Internet]. Goldman Sachs. 2020;[cited 2021 Dec 15]. Available from: https://www.goldmansachs.com/insights/pages/face-masks-and-gdp.html.
- 16. Leech G, Rogers-Smith C, Monrad JT, et al. Mask wearing in community settings reduces SARS-CoV-2 transmission. Proc Natl Acad Sci U S A 2022;119:e2119266119.ArticlePubMedPMC
- 17. Jehn M, McCullough JM, Dale AP, et al. Association between K-12 school mask policies and school-associated COVID-19 outbreaks: Maricopa and Pima Counties, Arizona, July-August 2021. MMWR Morb Mortal Wkly Rep 2021;70:1372−3.ArticlePubMedPMC
- 18. Bauer S, Contreras S, Dehning J, et al. Relaxing restrictions at the pace of vaccination increases freedom and guards against further COVID-19 waves. PLoS Comput Biol 2021;17:e1009288.ArticlePubMedPMC
- 19. Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ 2021;375:e068302.ArticlePubMed
- 20. Centers for Disease Control and Prevention (CDC). CDC real-world study confirms protective benefits of mRNA COVID-19 vaccines [Internet]. CDC; 2021 [cited 2021 Dec 11]. Available from: https://www.cdc.gov/media/releases/2021/p0329-COVID-19-Vaccines.html.
- 21. Adjodah D, Dinakar K, Chinazzi M, et al. Association between COVID-19 outcomes and mask mandates, adherence, and attitudes. PLoS One 2021;16:e0252315.ArticlePubMedPMC
- 22. World Health Organization (WHO). Strategy to achieve global covid-19 vaccination by mid-2022 [Internet]. WHO; 2021 [cited 2022 Mar 28]. Available from: https://www.who.int/publications/m/item/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022.
- 23. Besheer M. WHO launches strategy to vaccinate 40% of world against COVID by end of 2021. Voice of America [Internet]. 2021 [cited 2022 Jan 11]. Available from: https://www.voanews.com/a/who-launches-strategy-to-vaccinate-40-of-world-by-end-of-2021-/6261489.html.
- 24. Agarwal R, Gopinath G. A proposal to end the COVID-19 pandemic [Internet]. International Monetary Fund; 2021 [cited 2023 Jan 11]. Available from: https://www.imf.org/en/Publications/Staff-Discussion-Notes/Issues/2021/05/19/A-Proposal-to-End-the-COVID-19-Pandemic-460263.
- 25. Centers for Disease Control and Prevention (CDC). COVID data tracker [Internet]. CDC. 2021;[cited 2021 Dec 15]. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
- 26. Call M. Why is behavior change so hard? [Internet]. Accelerate Learning Community; 2022 [cited 2022 Aug 15]. Available from: https://accelerate.uofuhealth.utah.edu/resilience/why-is-behavior-change-so-hard.
- 27. Layyy P, van Jaarsveld CH, Potts HW, et al. How are habits formed: modeling habit formation in the real world. Eur J Soc Psychol 2010;40:998−1009.Article
- 28. Sharma M, Mindermann S, Rogers-Smith C, et al. Understanding the effectiveness of government interventions against the resurgence of COVID-19 in Europe. Nat Commun 2021;12:5820. ArticlePubMedPMCPDF
- 29. Stutt RO, Retkute R, Bradley M, et al. A modelling framework to assess the likely effectiveness of facemasks in combination with 'lock-down' in managing the COVID-19 pandemic. Proc Math Phys Eng Sci 2020;476:20200376. ArticlePubMedPMCPDF
- 30. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020;395:1973−87.ArticlePubMedPMC
- 31. Peeples L. Face masks: what the data say. Nature 2020;586:186−9.ArticlePubMedPDF
- 32. European Centre for Disease Prevention and Control (ECDC). Using face masks in the community: reducing COVID-19 transmission from potentially asymptomatic or pre-symptomatic people through the use of face masks [Internet]. ECDC; 2020 [cited 2021 Oct 28]. Available from: https://www.ecdc.europa.eu/en/publications-data/using-face-masks-community-reducing-covid-19-transmission.
- 33. Subramanian SV, Kumar A. Increases in COVID-19 are unrelated to levels of vaccination across 68 countries and 2947 counties in the United States. Eur J Epidemiol 2021;36:1237−40.ArticlePubMedPMCPDF
- 34. European Centre for Disease Prevention and Control (ECDC). Rapid Risk Assessment: Assessing SARS-CoV-2 circulation, variants of concern, non-pharmaceutical interventions and vaccine rollout in the EU/EEA, 16th update [Internet]. ECDC; 2021 [cited 2021 Oct 28]. Available from: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-assessing-sars-cov-2-circulation-variants-concern.
- 35. World Health Organization (2021). COVID-19 Virtual Press conference. 7 July 2021 [Internet]. WHO; 2021 [cited 2021 Sep 25]. Available from: https://www.who.int/publications/m/item/covid-19-virtual-press-conference-transcript---7-july-2021.
- 36. Patel MD, Rosenstrom E, Ivy JS, et al. Association of simulated COVID-19 vaccination and nonpharmaceutical interventions with infections, hospitalizations, and mortality. JAMA Netw Open 2021;4:e2110782.ArticlePubMedPMC
- 37. Huang C, Yang L, Pan J, et al. Correlation between vaccine coverage and the COVID-19 pandemic throughout the world: based on real-world data. J Med Virol 2022;94:2181−7.ArticlePubMedPMCPDF
- 38. Wang R, Wang J, Hu T, et al. Population-level effectiveness of COVID-19 vaccination program in the United States: causal analysis based on structural nested mean model. Vaccines (Basel) 2022;10:726. ArticlePubMedPMC
References
Figure & Data
References
Citations



 Cite
Cite