Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 13(4); 2022 > Article
-
Original Article
Characteristics of COVID-19 outbreaks and risk factors for transmission at an army training center in South Korea from June to August 2021 -
U Jin Cho1
 , Seongjin Wang1
, Seongjin Wang1 , Seonju Yi1
, Seonju Yi1 , Yeon Hwa Choi2
, Yeon Hwa Choi2 , Eun-Young Kim2
, Eun-Young Kim2 , Jin A Kim2
, Jin A Kim2 , Sanghwan Bae3
, Sanghwan Bae3 , Jungyeon Yu3
, Jungyeon Yu3 , Jangkyu Choi4
, Jangkyu Choi4 , Young-Joon Park1
, Young-Joon Park1
-
Osong Public Health and Research Perspectives 2022;13(4):262-272.
DOI: https://doi.org/10.24171/j.phrp.2022.0149
Published online: July 27, 2022
1Epidemiological Investigation Team, Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, Cheongju, Korea
2Division of Infectious Disease Response, Chungcheong Regional Center, Korea Disease Control and Prevention Agency, Daejeon, Korea
3Indoor Air Quality Research Center, Korea Institute of Civil Engineering and Building Technology, Goyang, Korea
4Gyeryongdae District Hospital, Republic of Korea Army Headquarters, Korea Army, Gyeryong, Korea
- Corresponding author: Young-Joon Park Epidemiological Investigation Team, Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Korea E-mail: pahmun@korea.kr
© 2022 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- It is crucial to establish the characteristics of coronavirus disease 2019 (COVID-19) outbreaks at army training centers to develop preventive measures. Therefore, this study aimed to determine the COVID-19 transmission patterns and risk factors in a sequence of outbreaks at an army training center from June to August 2021.
-
Methods
- This study included 1,324 trainees at an army training center where outbreaks occurred from June to August 2021. The outbreak was qualitatively analyzed according to the period, attack rate, demographic characteristics, vaccination history, and living areas. An aerodynamic experiment was performed to evaluate aerosol transmission in living areas.
-
Results
- Three outbreaks occurred at the army training center from June to August 2021. The first, second, and third outbreaks lasted for 32, 17, and 24 days, and the attack rates were 12.8%, 18.1%, and 8.9%, respectively. Confirmed cases were distributed in all age groups. Recruits and the unvaccinated were at higher risk for COVID-19. The aerodynamic experiment verified the possibility of aerosol transmission within the same living area.
-
Conclusion
- COVID-19 transmission at army training centers should be minimized through quarantine and post-admission testing during the latency period as part of integrated measures that include facility ventilation, vaccination, indoor mask-wearing, and social distancing.
- Coronavirus disease 2019 (COVID-19) is an infectious respiratory disease that can be transmitted from person to person and was first reported in China in December 2019 [1]. As of February 27, 2022, the global cumulative number of infected people was 400,003,300 and the number of deaths was 5,900,000. The number of infected people in South Korea was 139,626 as of February 2022 [2]. The first confirmed patient in South Korea was reported on January 20, 2020, after which the crisis alert level according to the number of confirmed patients increased from “alert” on January 27, 2020, to “severe” on February 23, 2020 [3]. Even 2 years after the initial outbreak, policies related to COVID-19 are still being implemented [4,5].
- Contact transmission of COVID-19 through respiratory droplets containing the virus is possible, and aerosol transmission in a closed environment has also been reported [6]. The most frequently reported COVID-19 symptoms are fever, dry cough, and fatigue, while other symptoms include loss of taste and olfactory senses, muscle pain, sore throat, nasal discharge or congestion, headache, eye inflammation, diarrhea, and skin irritation [7].
- Vaccinations in South Korea began on February 26, 2021. As of March 12, 2022, the number of first-dose vaccinated individuals was 44,903,107, accounting for 87.5% of the total population; the number of second-dose vaccinated individuals was 44,428,431, corresponding to 86.6% of the total population; and the number of third-dose vaccinated individuals was 32,064,014, accounting for 62.5% of the total population [8]. The main mode of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission is through respiratory droplets from an infected individual [9]. In South Korea, cases of COVID-19 have been reported during the outbreak in military facilities cohabited by younger adults [10].
- According to a recent report, the incidence of COVID-19 has been prominent in regions characterized by a “three-C” environment (concentrated, closed, and congested). Notably, the COVID-19 outbreak in the United States aircraft carrier Roosevelt resulted in approximately 26.6% of individuals testing positive, and the attack rate during the recent outbreak in the Cheonghae unit on board the ROKS Munmu the Great (DDH 976) was more than 80% [11]. Outbreaks have also been reported in facilities such as a Belgian army training center in Nigeria, underscoring the risk for the transmission of COVID-19 among army trainees in collective facilities [12,13].
- An example of the COVID-19 outbreak in a military facility was the one that occurred in an army training center from June to August, 2021 in Chungcheongnam-do (South Chungcheong Province), South Korea. Established in 1951, the center comprised a total of 7 regiments and had released 9 million new recruits by 2020. The trainees at the center were allocated to the same squad if they were residents of the same region. In mid-2021, admission to the army training center required 2 polymerase chain reaction (PCR) tests on day 1 and day 10. Until the confirmation of a negative result on the second PCR test, the trainees are quarantined in their assigned living area and are allowed to use only this space to prevent contact with anyone outside the living area. The trainees received their education and consumed their meals inside their living areas and also wore a mask at all times except while sleeping. Every morning, the body temperature of the trainees was checked, and any abnormalities in smell and taste were reported; these measures continued even after the confirmation of a negative result on the second PCR test. The training program at the center involved the trainees receiving a weekly training session at each different regiment for 5 weeks. During week 1 of admission, the trainees were allowed to consume their meals and participate in training within the living area, as well as using the washrooms and shower rooms of the living area. During week 2, trainees were allowed to have their meals at the troop’s canteen. During week 3, outdoor training sessions began, and the range of activity increased for the trainees (i.e., from squad to troop to regiment).
- Three outbreaks occurred from June to August 2021 at the army training center. The first outbreak occurred from June 22 to July 22, with 123 confirmed patients; the second outbreak occurred from July 12 to July 20, with 21 confirmed patients; and the third outbreak occurred from July 31 to August 18, with 22 confirmed patients. The first 2 outbreaks happened at similar times, but were considered as separate outbreaks because these occurred in completely separate cohorts of trainees. The locations of the first and second outbreaks were quite far (10 minutes by car). Vaccines are also a risk factor that affects transmission in an outbreak. Vaccination status was defined by using the terms “unvaccinated,” “first dose,” and “second dose.” People were classified as unvaccinated if they had not been vaccinated at all, or if they were within 14 days of receiving their first injection. People were defined as having received their first or second dose if 14 days had elapsed after the corresponding injection. The BNT162b2 mRNA vaccine (Pfizer-BioNTech), ChAdOx1 nCoV-19 (AZD1222) vaccine (AstraZeneca) and Ad26 vaccine (Janssen) were used. Some were inoculated with both mRNA and viral virus vector vaccines. In June to August 2021, the Delta variant was dominant in Korea. The Delta variant was first confirmed in April 2021, followed by 322 cases (10.7%) in June and 3,507 cases (50.3%) in July, showing the increasing trend during this time period [14].
- This study was conducted to identify the risk factors for COVID-19 transmission at the army training center and to provide insights into the management of outbreaks at military centers. The circumstances associated with COVID-19 incidence during similar periods were evaluated, and the source of infection and mode of transmission were analyzed. To prevent further transmission, periodic testing and preventive measures were undertaken. In addition, the characteristics of the facilities were analyzed through an on-site risk assessment. SARS-CoV-2 transmission was characterized, and the possibility of aerosol transmission was verified through aerodynamic experiments conducted at each facility.
Introduction
- Outbreak Recognition
- The study participants were trainees and support staff members who cohabited the same floor of the living area as the confirmed patients during each of the 3 outbreaks that occurred from June to August 2021.
- Case Definition and Epidemiological Investigations
- A confirmed patient was defined as an individual whose sample collected from the upper airways was positive for SARS-CoV-2 genetic material according to the diagnostic criteria, irrespective of clinical features, using PCR detection kits during the study period at the army training center (first outbreak: June 22 to July 22; second outbreak: July 12 to July 20; and third outbreak: July 31 to August 18) [15]. An index patient was defined as the individual with the earliest date of a confirmed diagnosis during an outbreak. A symptomatic patient was an individual who presented with symptoms. The estimated date of exposure was the time during which a patient was presumed to have been exposed to the virus from a confirmed patient during an outbreak. A basic epidemiological survey was used to evaluate demographic characteristics, the date of onset of symptoms, the attack rate, the exposure period, and vaccination status. To determine the date of onset of symptoms, the use of health facilities in the past was examined, which was re-assessed based on the history of exposure and military medical records. An aerodynamic experiment was performed to verify the potential of aerosol transmission in living areas an aerodynamic experiment and to help develop preventive measures against future outbreaks.
- Data Collection and Analysis
- To determine the source of infection, the military medical records of the confirmed patients were examined to examine the date of onset of symptoms, which was used to construct an epidemic curve and describe the outbreak characteristics and estimated date of exposure. The vaccination statuses of the confirmed patients and of those who came in close contact with these patients were checked, and the preventive impacts were assessed by analyzing the relevant effects among those who were unvaccinated, those who had received the first dose, and those who had received the second dose. An aerodynamic experiment was performed to verify the possibility of aerosol transmission. Jamovi 1.6.23 (Newcastle, New South Wales, Australia) was used for the statistical analysis. The attack rates of the outbreaks were analyzed and compared with the outbreak characteristics to determine risk factors for infection and examine variations in the attack rate according to the participants’ vaccination status. The data of this study were collected with cooperation of the military as part of the COVID-19 response at collective facilities; hence, informed consent from the study participants was not required. The aerodynamic experiment was conducted to identify the characteristics of air circulation in the army training center. The air flow was visualized when droplet-like particles were generated and sprayed, and droplet-like particle concentrations were measured according to air flow and space. In this experiment, measurements were made of airflow, contaminant diffusion, and particle concentration by using a smoke generator, an oil droplet generator, and an indoor air quality sensor.
- IRB/IACUC Approval
- This study was approved by the Institutional Review Board of the Republic of Korea Armed Forces Medical Command (No: AFMC-202204-HR-021-01) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained for publication of this study and accompanying images.
Materials and Methods
- Outbreak Recognition
- The exposure period of the first outbreak was from June 22 to July 22, 2021. The index patient was identified in the living area with the highest number of confirmed patients. As no additional confirmed patients were reported in the respective regiments after the second PCR test, outdoor training sessions commenced, and quarantine measures were implemented. Due to delayed diagnoses, the scale of the exposure had increased and confirmed patients were reported in buildings other than the building of initial concern. The second outbreak occurred from July 12 to July 20, resulting in 21 confirmed patients. The index patient was presumed to have been in contact with an infected person in the local community. The results of the second PCR tests of all the trainees indicated that the confirmed patients were in the same platoon and squad. The third outbreak occurred from July 31 to August 18. The index patient was identified based on the onset of symptoms on day 5 of admission; although the patient’s living area was quarantined, no further preventive measures were implemented because of the negative results of the trainees’ second PCR tests. Due to limited physical distancing, additional transmission occurred among individuals in the same living area.
- COVID-19 Prevention Management for the Army Trainees
- During the first outbreak, the admitted trainees spent 14 days (2 weeks) in each assigned living area with 2 periodic PCR tests on days 1 and 7 of admission, and they were provided special management until a negative result was received for the second PCR test. The trainees who experienced potential symptoms underwent additional PCR tests. Furthermore, contact and communication were prohibited, and trainees from the same region were allocated to the same squad to ensure efficient management. Similarly, during the second outbreak, the confirmed patients underwent 2 periodic PCR tests on days 1 and 7 of admission, and the trainees were given special management in their assigned living areas until a negative result was obtained in the second PCR test. Additional PCR tests for trainees experiencing potential symptoms were performed. During the third outbreak, 2 periodic PCR tests (on days 1 and 10 of admission) were performed and the trainees were provided special management in their assigned living areas until a negative result was received for the second PCR test result.
- General Characteristics of the Outbreak at the Army Training Center
- General characteristics of the outbreak are detailed in Table 1. In the first outbreak, 123 trainees (12.8%) among 960 male and 2 female trainees had a confirmed COVID-19 diagnosis. In terms of age stratification, 121 trainees aged <25 years (13.1%), and 2 trainees aged ≥25 years (5.6%) were diagnosed. In the second outbreak, 21 trainees (18.6%) among 113 male and 3 female trainees had a confirmed COVID-19 diagnosis; this included 19 trainees aged <25 years (20.2%), and 2 trainees aged ≥25 years (9.1%). In the third outbreak, 22 trainees (9.0%) among 244 male and 2 female trainees had a confirmed COVID-19 diagnosis; this included 22 trainees aged <25 years (9.4%) and no trainees aged ≥25 years.
- In all 3 outbreaks, neither officers nor sergeants had a confirmed COVID-19 diagnosis, and all the confirmed patients were trainees. The attack rates were 12.8%, 18.1%, and 8.9% in the first, second, and third outbreaks, respectively. The numbers of unvaccinated, people who got first dose, and second dose individuals were 904 (94.0%), 57 (5.9%), and 1 (0.1%), respectively, in the first outbreak; 88 (75.9%), 20 (17.2%), and 8 (6.9%), respectively, in the second outbreak; and 218 (88.6%), 3 (1.2%), and 25 (10.2%), respectively, in the third outbreak. Regarding the living area, confirmed patients were found in all sectors of both the first and second floors in the first outbreak but only in a single sector of the first floor in the second and third outbreaks (Table 1).
- The clinical symptoms reported by confirmed patients are presented in Table 2. The initial symptoms based on the survey results were sore throat (60.4%), fever (57.5%), cough (56.6%), and headache (52.8%) in the first outbreak; fever (80.0%), sore throat (46.7%), and headache (33.3%) in the second outbreak; and phlegm production (63.2%), cough (42.1%), fever (31.6%), and labored breathing (26.3%) in the third outbreak (Table 2).
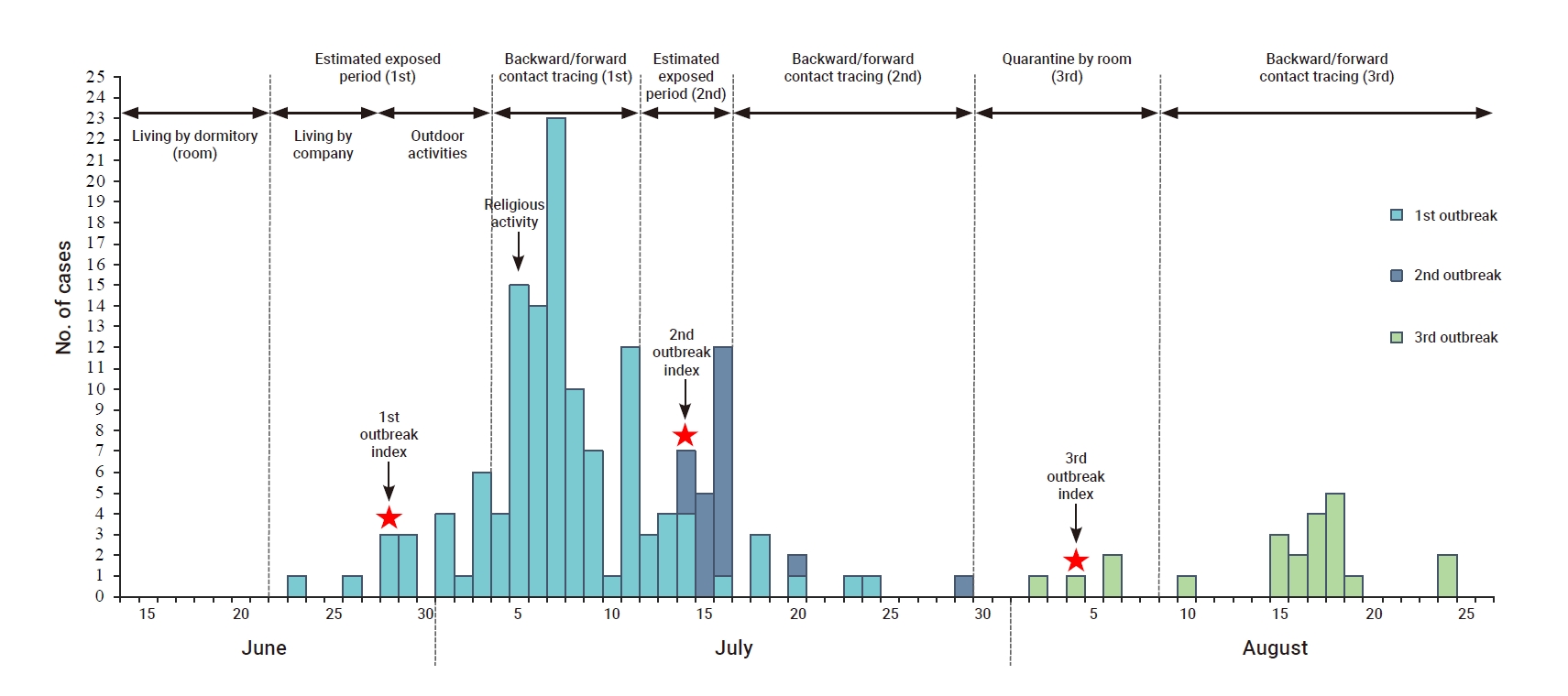
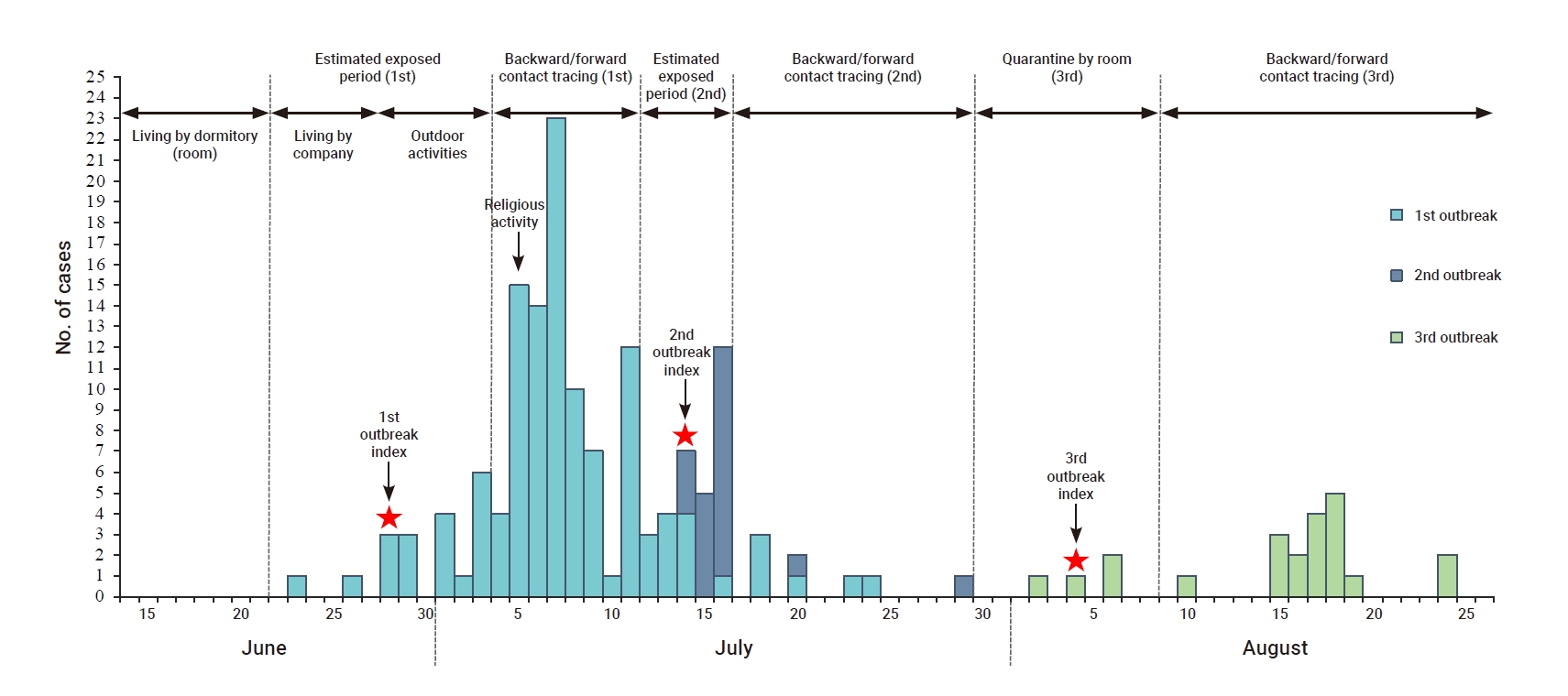
- Epidemic Curve
- Based on the date of onset of symptoms, the index patient in the first outbreak was a trainee in the third troop who presented with initial symptoms on June 28. Until day 7 of admission, the 2 PCR tests showed negative results. The trainee then presented with symptoms on day 14, and a positive PCR test result on day 22 led to the confirmed diagnosis. The index patient was quarantined for 8 days after the confirmed diagnosis, with reorganization of the trainee’s troop and a subsequent internal rearrangement. The scale of exposure increased as confirmed patients were also found in other troops and buildings. This may have been due to the inappropriate timing of the test of the suspected trainee without adjusting for the periodic test dates and relying solely on the 2 established periodic tests. In the second outbreak, the index patient showed initial symptoms on day 6 of admission and the second PCR test of all the trainees led to the confirmed diagnosis. Another confirmed patient was found in the same troop, and as the diagnosis was confirmed in the second PCR test, the scale of the exposure might have been reduced. In the third outbreak, the index patient showed initial symptoms on day 5 of admission, and 4 confirmed patients were found in the same living area on day 9. The close-contact individuals in the same living area were self-quarantined. On day 12, all trainees had negative results on the second PCR test; however, another symptomatic patient was found in a different living area on day 19, which prolonged the outbreak period (Figure 1).
- Risk Factors for Transmission at the Army Training Center
- Trainees were admitted to the army training center twice a week on Mondays and Thursdays. Due to the possibility of community-acquired infection and the COVID-19 latency period, PCR tests were performed on days 1 and 10 of admission. The number of admitted trainees exceeds the living area’s accommodation capacity for the troop, and the long hours of collective activities expose the trainees to an environment of spatial proximity.
- Sex- and rank-specific biases were noted among the COVID-19-confirmed patients at the army training center. Regarding vaccination status, the patients were all unvaccinated in the first and third outbreaks; therefore, it would be reasonable to say that vaccination helped not to be infected, but it was difficult to calculate values for this relationship, since very few of the infected individuals were vaccinated.
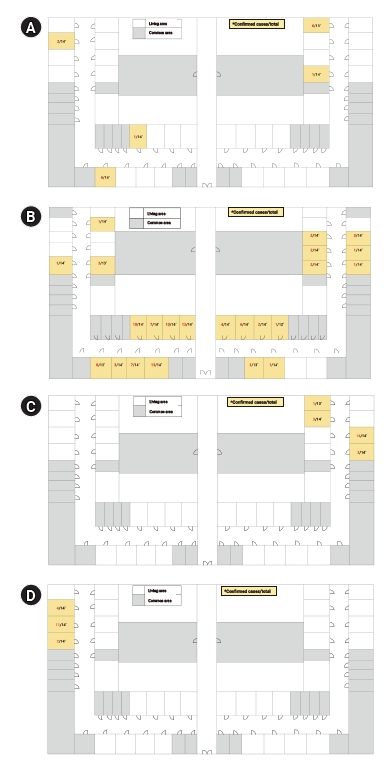
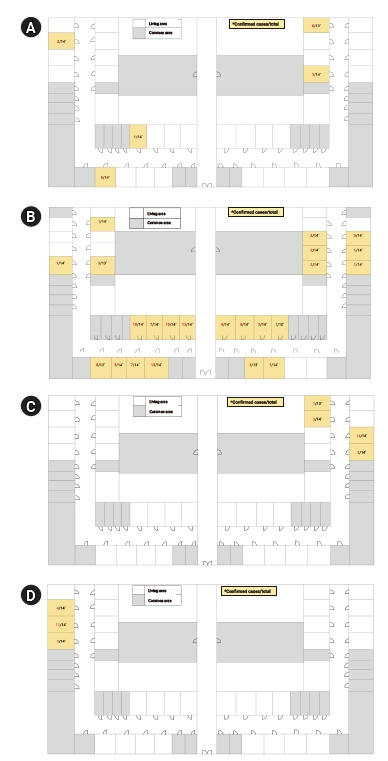
- South Korea’s summer, which lasts from mid-June to August, is the hottest time of the year. Temperatures may range between 23℃ and 30℃, but this is also the wettest time of the year, with the monsoon rains bringing half of the country’s annual rainfall during these months [16]. An aerodynamic experiment was performed where the second outbreak occurred, and the aerodynamic characteristics were analyzed to verify the possibility of aerosol transmission. In the living area, air conditioning and air purifying facilities were installed, but no specific ventilating facility was found (Figure 2). These were denoted as A and B for the first outbreak, C for the second outbreak, and D for the third outbreak. As shown in the left part of Figure 2C, 2 rooms were used. In room A, 5-μm particles, as aerosol-sized droplets, were sprayed for 3 minutes. At this time, both the outer windows of rooms A and B and the entrance door on the corridor were open. The outside wind speed was 0.4 to 2.5 m/s on a weak windy day, and the direction of the wind was coming in through the window of room A and going out through the corridor to room B. The experiment demonstrated that the particles generated in room A passed through the door and reached the center of the corridor after 2 minutes and reached the center of room B opposite the corridor after 5 minutes. Compared to the highest concentration in room A, the highest concentration in the corridor rose to 69.6% after 4 minutes and 6 seconds had elapsed, and the highest concentration in room B was 9.7% after 5 minutes and 14 seconds had elapsed. It was only after 15 minutes that the particle concentrations in room A, the corridor, and room B decreased to their initial concentration levels (Table 3). Therefore, it was concluded that infection through air propagation of aerosol droplets from the dormitory to another room was possible.
- Air dispersion was prevented by spatial separation in the corridor, with boundaries formed using vinyl screens. The investigation indicated that some natural ventilation was implemented, but due to the nature of trainees staying in the same space for a long time, the possibility of infection due to air diffusion was judged to be high. The experiment showed that when droplet-like particles were generated, the particles were dispersed to other living areas in large quantities, with partial dispersion to more distant areas as well. Although the investigation revealed that natural ventilation was present in certain areas, the potential of infection via aerosol transmission was high due to the characteristics of long-term cohabitation of trainees in a single or closed area. In the long term, complementing mechanical ventilation with natural ventilation in facilities is necessary to allow continuous ventilation.
Results
- The investigation of the 3 outbreaks at the army training center led to a revision of the COVID-19 prevention management guidelines for trainees after admission. Until the second outbreak, PCR tests were performed on days 1 and 10 of admission. However, a considerable number of confirmed patients were reported after the second PCR test in the first outbreak, resulting in the testing of all the trainees on days 1 and 12 of admission around the time of the third outbreak.
- In the first outbreak, no additional confirmed patients were reported until the trainees underwent their second PCR tests. Hence, the scale of the exposure increased and additional transmission occurred among several trainees. This was attributed to the inappropriate timing of the test of the suspected trainee and dependency on the 2 previously established periodic tests. In the second outbreak, the second PCR test results indicated that the scale of the outbreak might have been contained, as it occurred among trainees sharing the same living area as the index patient. In the third outbreak, additional transmission occurred in the same living area due to limited physical distancing among close contacts.
- The weekly daily living guidelines for the trainees after admission stated that PCR tests should be performed during the first and second weeks; therefore, lavatory and washroom use in each living area were differentiated and face-to-face contact was prevented through indoor education on the TV inside the living area. These measures were adopted to minimize contact with trainees from other squads. From the third week, trainees from 2 squads with negative results on the second PCR tests were allowed to share the lavatory and washroom and have meals at the canteen; they were also allowed to use the port exchange of each squad.
- To prevent the spread of COVID-19 across troops, the admitted trainees undergo 2 PCR tests (on days 1 and 10 of admission). However, the COVID-19 latency period according to the World Health Organization is an average of 2–14 days (0–27 days including outliers), which is longer than 10 days. Nonetheless, based on the army training center guidelines, trainees who were isolated in the unit’s living area and those of the same platoon or troop begin to share lines of movement after confirmation of a negative result on the second PCR test, which increased the scope of contact and the consequent risk of COVID-19 infection. Hence, given the shared lines of movement, trainees should continue to comply with regulations of social distancing and personal hygiene. In addition, considering the COVID-19 latency period, it is crucial for trainees, sergeants, and officers to be aware that individuals can present with symptoms even after a confirmed negative result on the second PCR test. Therefore, strict reports on symptomatic individuals should be continued even after the second PCR test of all the admitted trainees, and immediate tests should be performed for such individuals to ensure the early recognition of confirmed patients.
- An aerodynamic experiment was performed to verify the possibility of aerosol transmission. As the second outbreak persisted, the experiment was performed after the living area was evacuated. The results of the experiment showed that some trainees who shared the same corridors and lavatories as others in the same living area were likely to have been exposed to the virus without face-to-face contact through aerosol transmission or contact transmission. Subsequently, all the trainees with confirmed negative results on the second PCR test were monitored to prevent the risk of infection, and as the trainees of both squads began sharing lavatories and washrooms and had meals at the canteen from the third week, the number of confirmed patients may have increased.
- In general, the military was more adherent to social distancing than the general public, and efforts were taken to ensure appropriate compliance with the guidelines of social distancing to minimize additional transmission. The trainees upon admission were supervised to ensure that they followed the weekly guidelines, which were in line with the infectious disease guidelines, at the army training center.
- The risk factors identified for SARS-CoV-2 transmission at the army training center were difficulty in maintaining a 1-m distance between each person in the living area and difficulty in opening and closing the windows during the summer and winter seasons even though doing so would allow natural ventilation. Based on the results of the aerodynamic experiment, transmission of infectious respiratory diseases may be a cause for concern at the army training center, as most living areas face the corridor. Thus, it may be appropriate to keep the entrance door closed at all times while keeping the external windows open, except when the weather is severely hot or cold. For old living areas that lack mechanical ventilation facilities, discharging internal contaminants to the exterior through fans or wall-attached circulators is recommended. Installing mechanical ventilation facilities is recommended as a mid- to long-term solution to enhance the air quality in living areas and to prevent the transmission of infectious respiratory diseases.
- As army training centers are characterized by the long-term cohabitation of younger adults, ensuring the maintenance of social distancing is critical. In addition to preventive measures such as mandatory testing, quarantining of individuals returning from leave, and wearing masks inside and outside living areas, early recognition of confirmed patients should be promoted by setting a more inclusive scope of close-contact individuals and performing immediate tests on individuals when they present with symptoms.
- As several people cohabit a limited space at an army training center, ensuring adequate social distancing is challenging and close contacts are inevitable. Thus, compliance with reinforced regulations within living areas is required. First, each living area should be ventilated 2 to 3 times per hour (for at least 10 minutes each time) on a regular basis. Second, a symptomatic individual should immediately be tested and quarantined upon detection. In this respect, individuals should wear masks and practice personal hygiene. More stringent quarantine and isolation are also necessary with the development of new variants of concern. Third, while all trainees undergo PCR tests on days 1 and 10 or 12 of admission, either a periodic test should be performed once more, or laboratory errors should be minimized to ensure continuous monitoring and prevent delayed diagnoses. Fourth, to minimize contact within living areas and with other squads, trainees should be educated on avoiding conversations during mealtimes. Finally, vaccination should be recommended to the trainees before admission.
Discussion
- This study is significant as it reflects the status of current facilities and ventilation at an army training center through an aerodynamic experiment, the analysis of PCR test results to verify epidemiological correlations, and an online questionnaire. Furthermore, the findings of this study may contribute to COVID-19 management strategies at army training centers where new trainees are regularly admitted by verifying the potential of aerosol transmission in cohabitation areas, such as living areas and chapels, within the base and by notifying the military centers of areas that require improvements in facilities and the frequency of natural ventilation.
Conclusion
-
Ethics Approval
This study was approved by the Institutional Review Board of the Republic of Korea Armed Forces Medical Command (No: AFMC-202204-HR-021-01) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained for publication of this study and accompanying images.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The data used in this study are protected under the Personal Information Protection Act.
-
Authors’ Contributions
Conceptualization: UJC, SW, SY; Data curation: UJC, SW; Formal analysis: UJC, SW, YHC, EYK, JAK; Investigation: UJC, SW, JC; Methodology: UJC, SW, YJP; Project administration: UJC, JC; Resources: UJC, SW, SB, JY; Software: UJC, SW, SY; Supervision: YJP; Validation: UJC, SW, YJP; Visualization: UJC, SW; Writing–original draft: UJC, SW; Writing–review & editing: all authors.
-
Additional Contributions
We thank the Republic of Korea Army Headquarters, including the army training center, for their efforts in responding to COVID-19 outbreaks.
Article information
- 1. World Health Organization (WHO). Novel Coronavirus (2019-nCoV): situation report, 1 [Internet]. Geneva: WHO; 2021 [cited 2020 Jan 21]. Available from: https://apps.who.int/iris/handle/10665/330760.
- 2. World Health Organization (WHO). Weekly epidemiological update on COVID-19-1 March 2022. Edition 81 [Internet]. Geneva: WHO; 2021 [cited 2022 Mar 1]. Available from: https://who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---1-march-2022.
- 3. Kim Y, Kim YY, Yeom H, et al. COVID-19 1-year outbreak report as of January 19, 2021 in the Republic of Korea. Public Health Wkly Rep 2021;14:472−81.
- 4. Gibson-Fall F. Military responses to COVID-19, emerging trends in global civil-military engagements. Rev Int Stud 2021;47:155−70.Article
- 5. Segal D, Rotschield J, Ankory R, et al. Measures to limit COVID-19 outbreak effects among military personnel: preliminary data. Mil Med 2020;185:e1624−31.ArticlePubMedPMCPDF
- 6. Li Y, Qian H, Hang J, et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build Environ 2021;196:107788. ArticlePubMedPMC
- 7. Yoo JH, Hong ST. The outbreak cases with the novel coronavirus suggest upgraded quarantine and isolation in Korea. J Korean Med Sci 2020;35:e62.ArticlePubMedPMCPDF
- 8. Korea Disease Control and Prevention Agency. The current statuses of COVID-19 outbreak and vaccination in South Korea (00:00, Sat. March 12) [Internet]. Cheongju: Korea Disease Control and Prevention Agency; 2022 [cited 2022 Mar 12]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=718969&cg_code=&act=view&nPage=15. Korean.
- 9. Park SY, Kim YM, Yi S, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis 2020;26:1666−70.ArticlePubMedPMC
- 10. Kim C, Kim YM, Heo N, et al. COVID-19 outbreak in a military unit in Korea. Epidemiol Health 2021;43:e2021065.ArticlePubMedPMC
- 11. Korea Disease Control and Prevention Agency. The result of the epidemiological study on the COVID-19 outbreak in the Cheonghae unit [Internet]. Cheongju: Korea Disease Control and Prevention Agency; 2021 [cited 2021 Aug 10]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=716455&cg_code=&act=view&nPage=1. Korean.
- 12. Pirnay JP, Selhorst P, Cochez C, et al. Study of a SARS-CoV-2 outbreak in a Belgian military education and training center in Maradi, Niger. Viruses 2020;12:949. ArticlePubMedPMC
- 13. Kasper MR, Geibe JR, Sears CL, et al. An outbreak of Covid-19 on an aircraft carrier. N Engl J Med 2020;383:2417−26.ArticlePubMedPMC
- 14. Kim IH, Park AK, Lee H, et al. July 2021 status and characteristics of the COVID-19 variant virus outbreak in the Republic of Korea. Public Health Wkly Rep 2021;14:3388−96.
- 15. Korea Disease Control and Prevention Agency. COVID-19 response guidelines (for local governments) (10-1 Edition) [Internet]. Cheongju: Korea Disease Control and Prevention Agency; 2021 [cited 2021 Nov 8]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019. Korean.
- 16. Selective Asia. When is the best time to visit South Korea? [Internet]. Brighton: Selective Asia; 2022 [cited 2022 June 20]. Available from: https://www.selectiveasia.com/south-korea-holidays/weather#:~:text=The%20brief%20summer%20lasts%20from,annual%20rainfall%20during%20these%20months.
References
Figure & Data
References
Citations

- COVID-19 outbreak in a religious village community in Republic of Korea and risk factors for transmission
Jiae Shim, Eunju Lee, Eunyoung Kim, Yeonhwa Choi, Giseok Kang, Bryan Inho Kim
Osong Public Health and Research Perspectives.2023; 14(2): 110. CrossRef - Epidemiological Characteristics of a COVID-19 Outbreak in a Psychiatric Hospital in Chung-buk
Se-Hyuk Jang, Young-Joon Park, Ji-Joo Lee, Woo-Jin Jung
Healthcare.2023; 11(16): 2332. CrossRef


 Cite
Cite