Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 13(3); 2022 > Article
-
Original Article
Changes in the pattern and disease burden of acute respiratory viral infections before and during the COVID-19 pandemic -
Chungmin Park1
 , Donghan Lee2
, Donghan Lee2 , Bryan Inho Kim1
, Bryan Inho Kim1 , Sujin Park3
, Sujin Park3 , Gyehee Lee3
, Gyehee Lee3 , Sangwoo Tak1
, Sangwoo Tak1
-
Osong Public Health and Research Perspectives 2022;13(3):203-211.
DOI: https://doi.org/10.24171/j.phrp.2022.0144
Published online: June 30, 2022
1Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Korea
2Gyeongnam Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency, Busan, Korea
3Division of Infectious Disease Control, Bureau of Infectious Disease Policy, Korea Disease Control and Prevention Agency, Cheongju, Korea
- Corresponding author: Sangwoo Tak Division of Risk Assessment, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, 187 Osongsaengmyeong 2-ro, Osong-eup, Heungdeok-gu, Cheongju 28159, Korea E-mail: taksw@korea.kr
© 2022 Korea Disease Control and Prevention Agency.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- We conducted a comparative analysis of the differences in the incidence of 8 acute respiratory viruses and the changes in their patterns before and during the coronavirus disease 2019 (COVID-19) pandemic.
-
Methods
- Three sentinel surveillance systems of the Korea Disease Control and Prevention Agency and data from the Health Insurance Review and Assessment Service were analyzed. The average numbers of reported cases and the related hospital admissions and outpatient data were compared between April 2018–2019 and 2020–2021. Changes in the disease burden and medical expenditures between these 2 time periods were evaluated.
-
Results
- During the COVID-19 pandemic, the number of reported cases of all acute respiratory viral infections, except for human bocavirus, decreased significantly. Data from the Health Insurance Review and Assessment Service also showed decreases in the actual amount of medical service usage and a marked reduction in medical expenditures.
-
Conclusion
- Non-pharmacological interventions in response to COVID-19 showed preventive effects on the transmission of other respiratory viruses, as well as COVID-19. Although COVID-19 had a tremendous impact on society as a whole, with high social costs, there were also positive effects, such as a reduction in the incidence of acute respiratory viral infections.
- Since the first coronavirus disease 2019 (COVID-19) case was reported on January 20, 2020, Korea sequentially extended the crisis response level in its response against the spread of COVID-19. It emphasized adherence to precautions for personal hygiene, including wearing a mask, and initiated society-wide measures such as social distancing. As part of these efforts, surface disinfection was also emphasized in healthcare facilities and all other areas [1]. The transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the virus that causes COVID-19) and acute respiratory viruses occurs mainly through respiratory droplets via close contact, direct contact with infected people, or indirect contact with contaminated objects or surfaces [2]. Hence, the aforementioned preventive measures could affect the spread of both SARS-CoV-2 and other respiratory viruses, such as influenza. A major example of this effect is the early end of 2019–2020 seasonal influenza epidemic in Korea. The incidence of respiratory infections has markedly decreased compared with the pre-COVID-19 period [3−5]. In addition, the average positivity rate of the 8 acute respiratory infections (influenza and 7 acute respiratory infections) analyzed by the Korea Influenza and Respiratory Viruses Surveillance System (KINRESS) decreased from 54.7% and 62.0% between 2010 and 2019 to 39.1% and 38.7% in 2020, respectively [6,7]. The decrease in the direct disease burden of these 8 acute respiratory viral infections and the subsequent reduction in medical expenses were measured in this study. Although the sentinel surveillance system monitors the occurrence of these 8 acute respiratory viral infections, the reduction in the number of reported cases in the sentinel surveillance system cannot be used as a direct index of measuring medical expenditures or the disease burden due to differences between diseases in severity and the standards of medical expenses. This study aimed to compare the incidence of acute respiratory viral infections and the associated disease burdens. We comprehensively analyzed sentinel surveillance data from 3 surveillance systems: the KINRESS, Acute Respiratory Infection Surveillance System (ARI), and the Severe Acute Respiratory Infection Surveillance System (SARI) established by the Korea Disease Control and Prevention Agency (KDCA; Cheongju, Korea), as well as data on medical service utilization and expenditures from the Health Insurance Review and Assessment Service (HIRA).
Introduction
- Definition
- The KINRESS is a surveillance system that monitors acute respiratory viral infections in outpatients visiting over 52 primary clinics designated as sentinel sites. The national surveillance of ARI involves monitoring trends in the incidence of acute respiratory infections, including influenza, in admitted patients and outpatients of 214 hospitals with over 200 beds. The national SARI surveillance system monitors patients with severe disease admitted to 42 medical institutions of the general hospital level who meet the SARI case definition (history of fever of 38.0°C or higher and cough with symptom onset within 10 days before hospitalization). The ARI and SARI have reports on viral respiratory infections confirmed by tests conducted in hospital laboratories. Meanwhile, in the KINRESS, the Public Health and Environment Research Institute, conducts polymerase chain reaction (PCR) tests on samples collected from sentinel sites. The results are reported to the KDCA for analysis at the national level. The SARI surveillance system was originally implemented at 13 hospitals for 8 months of the year. As COVID-19 spreads, the system was expanded to 42 hospitals and has been operated throughout the year. In this study, expenditures were converted from Korean won (KRW) to US dollars (USD) with the exchange rate of 1,200 KRW for 1 USD.
- Data Source
- In this study, the numbers of weekly cases of the 8 acute respiratory viruses reported via these 3 surveillance systems (KINRESS, ARI, and SARI) were collected for analysis: adenovirus (ADV), human bocavirus (HBoV), human coronavirus (HCoV), human metapneumovirus (HMPV), human rhinovirus (HRV), human parainfluenza virus (HPIV), respiratory syncytial virus (RSV), and influenza virus (IFV). The data filed as the main diagnoses in the HIRA between January 2018 and April 2021 according to the date of medical service covered by national mandatory health insurance were used to calculate the number of treatment cases per infection that corresponded to the disease codes for the main diagnoses: ADV (J120, B970), HBoV (J1280, J2080, J2180), HCoV (B972), HMPV (J123, J211), HRV (J206), HPIV (J122, J204), RSV (J121, J205J J210, B974), and IFV (J09, J10, J11). Claims by pharmacies and oriental medicine clinics were excluded. Data on 7 viruses (excluding HBoV) were downloaded from the healthcare big data hub website (https://opendata.hira.or.kr/home.do), which is managed by the HIRA, whereas data on HBoV were provided by the HIRA.
- Study Design
- A retrospective, ecological study design was used to analyze changes in the incidence of various respiratory infections before and during the COVID-19 pandemic. We comprehensively analyzed sentinel surveillance data from 3 surveillance systems: KINRESS, ARI, SARI established by the Korea Centers for Disease Control and Prevention (Cheongju, Korea). The surveillance systems analyzed in this study are at the national level, covering all 17 metropolitan cities and provinces and offering national coverage. The number of cases was defined as the number of symptomatic patients who visited the sentinel sites and were confirmed with the viral respiratory infections through PCR. The data reported from week 1 of 2018 to week 16 of 2021 were aggregated by week and used for analysis. To compare trends in viral respiratory infections from each surveillance system (KINRESS, ARI, and SARI) before and during the COVID-19 pandemic (starting on January 20, 2020), the number of average weekly cases from 2018 to 2019 (24 months) and those from January 2020 to April 23, 2021 (16 months) was compared using the independent sample t-test. The reduction rate was determined from the means of the weekly averages between the 2 time periods. The disease burden of the 8 acute respiratory viral infections was measured using the monthly average number of patients during 2018–2019 (24 months) before the COVID-19 pandemic and January 2020–April 2021 (16 months) during the COVID-19 pandemic after organizing the data, which were previously categorized by disease codes of the main diagnosis and by type of infection. The reduction in disease burden was measured using the difference in the number of patients between the pre-COVID-19 period and during the COVID-19 pandemic. Direct medical expenditures were measured as the total medical care costs, defined as the sum of health insurance coverage and copays, from the 16-month periods of January 2018 to April 2019 (16 months) and January 2020 to April 2021 (16 months).
- Statistical Analysis
- Statistical analyzes were conducted using Excel 2013 (Microsoft Corp., Redmond, WA, USA) and IBM SPSS ver. 28.0 (IBM Corp., Armonk, NY, USA). The independent-samples t-test was used.
- IRB Approval
- The requirement for informed consent was exempted by the Institutional Review Board (IRB) of the KDCA (IRB-2021-06-03-PE-A) as there was no personal information in the study.
Materials and Methods
- The weekly incidence and the overall pattern of the 8 acute respiratory viruses based on each surveillance system before and during the COVID-19 pandemic were analyzed. In the KINRESS, HBoV showed no differences in the COVID-19 period (5.3 weekly cases on average) from the pre-COVID-19 period (5.3 weekly cases on average) (Table 1). However, the reports of all the other viruses decreased significantly in all surveillance systems. In the KINRESS, HPIV showed the largest decrease (97.6%), whereas HRV showed the smallest decrease (44.0%). Likewise, in the ARI, HPIV showed the largest decrease (95.2%), and HCoV showed the smallest decrease (55.4%). In the SARI, HPIV and HMPV showed the largest decreases (94.9% and 94.5%), respectively, and HBoV showed the smallest decrease (41.6%). HPIV and HMPV showed the greatest reductions in all surveillance systems, and the remaining 6 viruses showed reduced reporting rates overall.
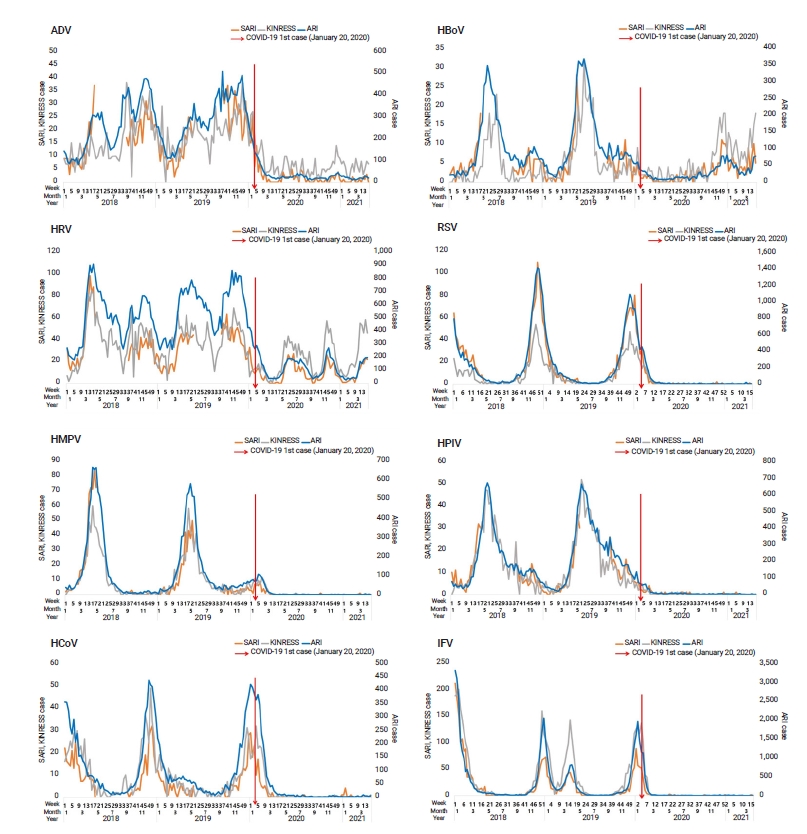
- Among the 8 acute respiratory viruses in the surveillance systems (KINRESS, ARI, and SARI), 5 (HMPV, HCoV, RSV, HPIV, and IFV) showed almost no significant seasonal increase since week 13 of 2020, which is after the start of the COVID-19 pandemic (Figure 1). However, ADV, HBoV, and HRV continued to be reported, although the numbers in the COVID-19 period had decreased compared with the pre-COVID-19 period. Before the COVID-19 pandemic, ADV had no apparent seasonal trend, although its spread tended to somewhat decrease in later winter (February to March) in 2018 and 2019, whereas the other viral pathogens displayed clear seasonal trends. The number of HRV cases tended to increase in spring and fall and somewhat decrease in summer (August 2018 and 2019) and late winter (February 2018–March 2019). The number of HMPV infection cases started increasing in spring (March), peaked in May, and lasted until early summer (July). The number of HPIV infection cases started increasing in spring (March), peaked in June, and lasted until winter (January), with a somewhat low number of cases between February and March. RSV, HCoV, and IFV showed the highest incidence during the winter (November to February), and the number of IFV infection cases increased again in the spring of 2019 (March to May), which showed the second seasonal peak of IFV. The number of HBoV infection cases tended to increase between spring and early fall (April to September).
- The monthly average number of cases of these 8 viruses in Korea during the same periods showed the following results: the number of HPIV infection cases decreased by 600.6 (93.9%) from 639.6 in 2018–2019 to 39.0 in January 2020 to April 2021, showing the largest reduction, followed by HMPV cases, with a decrease of 554.1 (91.7%) from 604.3 in 2018–2019 to 50.2 in January 2020 to April 2021. The number of ADV cases decreased by 286.9 (85.2%) from 336.9 in 2018–2019 to 49.9 in January 2020 to April 2021, and the number of RSV cases decreased by 1,627.0 (75.9%) from 2,143.9 in 2018–2019 to 516.9 in January 2020 to April 2021. The number of IFV cases decreased by 74.7% from 206,252.0 in 2018–2019 to 52,103.4 in January 2020 to April 2021. The numbers of HRV cases decreased by 440.6 (56.0%) from 787.2 in 2018–2019 to 346.6 in January 2020 to April 2021, the number of HBoV cases decreased by 166.4 (38.3%) from 434.5 in 2018–2019 to 268.1 in January 2020 to April 2021, and the number of HCoV cases increased by 3.6 (450.0%) from 0.8 in 2018–2019 to 4.4 in January 2020 to April 2021.
- The largest reduction in admission was found for HPIV (96.6%), followed in descending order by HMPV (92.4%), ADV (87.0%), RSV (81.6%), IFV (71.9%), HCoV (55.9%), HRV (33.9%), and HBoV (13.7%). For outpatient care, the largest reduction was found for HMPV (90.4%), followed by HPIV (89.7%), ADV (81.4%), IFV (75.0%), RSV (70.3%), HBoV (52.4%), and HCoV (55.0%) (Table 2). However, the number of HCoV infection cases increased from 0.1 in 2018–2019 to 4.1 in January 2020 to April 2021, showing a 1,675.0% increase.
- The direct medical expenditures for the 8 acute respiratory virus infections were 335,191,696.4 USD in 2018 to April 2019 and 83,857,157.8 USD in January 2020 to April 2021, showing a 75.0% decrease (Figure 2). Among them, IFV accounted for 89.6% of the total medical expenditures (300,402,640.8 USD) in January 2018 to April 2019 and for 89.2% of the total medical expenditures (74,822,896.7 USD) in January 2020 to April 2021. The high incidence of IFV explains why it accounted for approximately 90% of the total medical expenditures for the 8 viruses.
Results
- This study measured the reduction in the disease burden and medical expenditures observed after the implementation of social distancing, adherence to hygiene precautions, and surface disinfection during the response to the COVID-19 pandemic. We found that acute respiratory infections decreased significantly during the response to COVID-19, whereas most acute respiratory viruses displayed clear seasonal trends before the COVID-19 pandemic [6]. Significant reductions were also found for hospital visits and the observations made by the SARI, which is a system based on admitted patients. The direct medical costs of the 8 acute respiratory virus infections also decreased from 75% to 90% depending on the viral infections, reflecting the reduced number of cases of all 8 viral infections.
- A study by Jang et al. [7] on the factors determining medical expenses and length of stay for admitted patients with COVID-19 in Korea reported that the average medical cost for COVID-19 cases was 1,193.7 USD based on HIRA data. The total number of COVID-19 cases in Korea between January 2020 and April 2021 was 122,634, and the direct medical costs for COVID-19 during this time were 146,388,205.8 USD. During this time, the medical expenditures for the 8 acute respiratory virus infections were 83,857,157.5 USD, and the medical expenditures for IFV infections were 74,822,896.7 USD. The direct medical costs for COVID-19 were higher than those of the other infections, which had decreased by 75% from the previous years, but were much lower than the medical expenditures from January 2018 to April 2019, including the costs for IFV infections. However, these costs for COVID-19 exclude direct costs paid by the national treasury, such as expenses for free diagnostic tests operated by public health centers; therefore, these figures do not fully represent the direct costs of COVID-19.
- Outbreaks of most respiratory virus infections have markedly decreased since the onset of the COVID-19 pandemic due to intensive preventive measures such as social distancing, adherence to precautions for personal hygiene (wearing a mask and washing hands regularly), and disinfection. Among the 8 viruses analyzed in this study, 5 (HMPV, HCoV, RSV, HPIV, and IFV) had almost no associated cases. The other 3 viruses (ADV, HBoV, and HRV) continued to spread, but with fewer infections than in previous years. Our study results showed similar patterns to those reported in previous studies [8,9]. The surveillance of influenza-like illness (ILI) in Taiwan showed a rapid decrease from week 5 in 2020, after preventive measures against COVID-19 were implemented [6], and a record-low number of influenza cases was reported in February since the implementation of the national healthcare service in 1996 [6]. Wearing a mask is effective not only against COVID-19, but also against the spread of other viruses transmitted by droplets [10,11]. In a randomized controlled study, coronavirus was detected in 30% to 40% of participants who did not wear a mask, but not in those who wore a mask [10]. Although wearing a mask during the non-epidemic season did not show a statistically significant decrease in the number of acute respiratory viral infections, it was still a critical measure to reduce viral transmission during the COVID-19 pandemic [11,12].
- The infection and transmission of respiratory viruses can be prevented by precautions for personal hygiene such as washing hands [13,14]. Social distancing is another way to prevent transmission of the virus by limiting the population’s social contacts [15].
- In line with previous studies, the reduction in the number of cases of respiratory viruses in Korea since 2020 likely occurred due to non-pharmaceutical interventions such as social distancing and adherence to precautions for personal hygiene (wearing a mask and hand sanitization) initiated due to the COVID-19 pandemic [16,17]. The precautions and preventive measures implemented to reduce the spread of COVID-19 were not only effective for COVID-19, but also for other respiratory infections. This led to a decrease in the number of patients and a reduction in the actual disease burden (e.g., direct medical costs).
- Five viruses (HCoV, HPIV, HMPV, RSV, and IFV) showed extremely low number of cases after week 13 of 2020. Of note, these are enveloped viruses. HCoV is a positive-sense single-stranded RNA virus, and the remaining 4 viruses are negative-sense single-stranded RNA viruses. They are enveloped single-stranded RNA viruses, similar to SARS-CoV-2 [18]. The 3 viruses (ADV, HBoV, and HRV) that continued to be reported even during the COVID-19 pandemic are non-enveloped viruses [19]. ADV is a non-enveloped double-stranded DNA virus [20], HBoV is a non-enveloped single-stranded DNA virus [21], and HRV is a non-enveloped single-stranded RNA virus [22].
- Enveloped viruses are known to be easily inactivated by heat, dryness, detergent, and lipid solvents, unlike non-enveloped viruses [23]. Enveloped viruses are normally resistant to various environmental factors; therefore, they can survive longer in the external environment. Moreover, as they are resistant to acids and bile, they are the main cause of gastrointestinal infections [24]. Several studies have reported the inactivation of enveloped and non-enveloped viruses. Lipophilic disinfectants are mainly used to inactivate enveloped viruses, whereas glutaraldehyde or sodium hypochlorite is more effective at inactivating non-enveloped viruses [25]. The hand sanitizers widely used against COVID-19 are mainly composed of ethanol, which is effective against SARS-CoV-2, an enveloped virus. However, they are not as effective against the non-enveloped viruses [26]. For disinfecting against enveloped viruses, the use of 0.05% to 0.1% sodium hypochlorite or grade 4-ammonium salt disinfectant for 5 minutes or longer is recommended. For non-enveloped viruses, disinfection with 0.1% sodium hypochlorite disinfectant for over 5 minutes is recommended. Furthermore, sodium hypochlorite at 6,000 ppm is needed to disinfect against ADV, a non-enveloped virus [27]. Several studies have been conducted on SARS-CoV-2, an enveloped virus, regarding its survival period and disinfection [28,29]. Of note, despite sealing the diluent bottle, leaving any disinfectant at room temperature for 30 days leads to a 50% decrease in the available chlorine content. As the disinfecting effect is the strongest shortly after production, it is desirable to use disinfectants immediately after production at the manufacturing site [30].
- Although there are several ways to prevent virus transmission, the changes in the overall patterns of each virus in our study suggest the need to use different disinfectants according to the characteristics of the viruses, such as the presence or absence of an envelope. Therefore, further studies in hospital settings are required to measure the effects of different disinfectants on the spread of different respiratory viruses in healthcare facilities. Additional studies are needed on the social gains and losses that resulted from the COVID-19 pandemic in various areas. Our study results could be adopted by other studies, as we clearly documented changes in the incidence patterns and disease burden of other viral diseases due to the COVID-19 pandemic.
- This study has some limitations. First, unlike the surveillance system in which all the pathogens confirmed by diagnostic tests are reported, the main diagnosis codes from the HIRA data are filed for insurance claims and thus can be different from patients’ actual diagnoses [31]. In outpatient care, patients with ILI can be reported using common diagnosis codes instead of more detailed diagnosis codes when numerous patients are treated within a short period of time. Hence, since the main diagnosis codes from the HIRA data alone cannot verify whether a specific infection has been confirmed, the frequency of a specific disease code may not represent the total incidence of that pathogen in Korea. The increase in the number of HCoV cases after the COVID-19 pandemic in outpatients reported using the main diagnosis codes could be explained by the above reason. The total costs of direct medical expenditures include health insurance coverage and copays, while excluding non-payment items. Actual medical expenditures are likely to be higher than the reported amounts, and the medical costs presented herein are very likely underestimated.
Discussion
- Non-pharmaceutical interventions implemented due to COVID-19, such as social distancing, adherence to precautions for personal hygiene, and wearing a mask, as well as intensified disinfection in various settings, had positive effects on preventing the spread of not only COVID-19, but also other respiratory infections. As a result, there were significant reductions in the direct and indirect disease burden, as well as in medical expenditures for acute respiratory viral infections.
Conclusion
-
Ethics Approval
The requirement to obtain informed consent was exempted by the Institutional Review Board (IRB) of Korea Disease Control and Prevention Agency (IRB-2021-06-03-PE-A) as there was no personal information in the study.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
-
Authors’ Contributions
Conceptualization: DL, ST; Data curation: SP, CP; Formal analysis: CP; Methodology: CP, ST; Project administration: CP; Resources: CP; Visualization: CP, SP, GL; Writing–original draft: CP; Writing–review & editing: all authors.
-
Additional Contributions
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Korea Disease Control and Prevention Agency or the institutions with which the authors are affiliated.
Article information

| Virus |
KINRESS |
ARI |
SARI |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 2018–2019 (n=104) | 2020–(n=68) | Difference(%)a) | 2018–2019 (n=104) | 2020–(n=68) | Difference (%)a) | 2018–2019 (n=72) | 2020– (n=68) | Difference(%)a) | |
| ADV | 17.2±8.0 | 6.7±5.0 | 60.0*** | 276.8±114.4 | 38.2±46.5 | 86.2*** | 17.6±9.2 | 2.4±4.4 | 86.5*** |
| HBoV | 5.3±6.5 | 5.3±5.0 | 0.4 | 114.2±95.1 | 29.7±20.9 | 74.0*** | 4.9±4.6 | 2.8±2.8 | 41.6** |
| HRV | 38.9±17.7 | 21.8±15.5 | 44.0*** | 534.1±187.3 | 128.0±89.0 | 76.0*** | 35.6±18.5 | 9.5±8.3 | 73.3*** |
| HMPV | 11.4±14.7 | 1.2±3.0 | 89.6*** | 134.6±179.4 | 11.6±27.7 | 91.4*** | 12.5±20.4 | 0.7±1.8 | 94.5*** |
| RSV | 9.7±12.5 | 2.7±7.0 | 44.0*** | 270.4±354.1 | 65.1±176.9 | 75.9*** | 26.5±26.0 | 4.1±13.0 | 84.4*** |
| HCoV | 10.0±12.5 | 2.7±7.0 | 72.2*** | 110.2±114.8 | 49.2±113.9 | 55.4*** | 8.5±7.8 | 2.0±5.4 | 77.0*** |
| HPIV | 14.5±13.2 | 0.4±1.0 | 97.6*** | 224.9±175.8 | 10.8±22.8 | 95.2*** | 10.1±8.7 | 0.5±1.1 | 94.9*** |
| IFV | 35.9±49.7 | 10.3±32.7 | 71.3*** | 361.4±615.5 | 125.3±392.7 | 65.3** | 29.5±41.2 | 4.9±15.7 | 83.6*** |
Data are presented as mean±standard deviation. 2018–2019: before COVID-19, 2020–: during COVID-19. KINRESS, ARI 2018–2019 (n=104; 52 weeks in each year), 2020–April 24, 2021 (n=68; 52 weeks in 2020+16 weeks in 2021), SARI 2018–2019 (n=72; operated for about 8 months during the influenza epidemic before the COVID-19 outbreak, no data during weeks 19–35 of 2018 and weeks 22–36 of 2019).
COVID-19, coronavirus disease 2019; KINRESS, Korea Influenza and Respiratory Viruses Surveillance System; ARI, Acute Respiratory Infection Surveillance System; SARI, Severe Acute Respiratory Infection Surveillance System; ADV, adenovirus; HBoV, human bocavirus; HRV, human rhinovirus; HMPV, metapneumovirus; RSV, respiratory syncytial virus; HCoV, human coronavirus; HPIV, parainfluenza virus; IFV, influenza virus.
a) {(2018–2019)–(2020–)}/(2018–2019)×100.
** p<0.01,
*** p<0.001.
| Pathogens |
Total (admission+outpatient) |
Admissions |
Outpatient visits |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018–2019 Monthly average | 2020– Monthly average | Differencea) | Difference (%)b) | 2018–2019 Monthly average | 2020–Monthly average | Differencea) | Difference (%)b) | 2018–2019 Monthly average | 2020–Monthly average | Differencea) | Difference (%)b) | |
| ADV | 336.9 | 49.9 | 286.9 | 85.2 | 227.6 | 29.6 | 198.0 | 87.0 | 109.3 | 20.3 | 88.9 | 81.4 |
| HBoV | 434.5 | 268.1 | 166.4 | 38.3 | 158.5 | 136.9 | 21.7 | 13.7 | 276.0 | 131.3 | 144.8 | 52.4 |
| HRV | 787.2 | 346.6 | 440.6 | 56.0 | 162.4 | 107.3 | 55.1 | 33.9 | 624.8 | 239.3 | 385.5 | 61.7 |
| HMPV | 604.3 | 50.2 | 554.1 | 91.7 | 386.6 | 29.4 | 357.3 | 92.4 | 217.7 | 20.8 | 196.9 | 90.4 |
| RSV | 2,143.9 | 516.9 | 1,627.0 | 75.9 | 1054.8 | 193.9 | 860.9 | 81.6 | 1,089.1 | 322.9 | 766.2 | 70.3 |
| HCoV | 0.8 | 4.4 | –3.6 | –450.0 | 0.7 | 0.3 | 0.4 | 55.9 | 0.3 | 4.4 | –4.2 | –1,675.0 |
| HPIV | 639.6 | 39 | 600.6 | 93.9 | 389.6 | 13.3 | 376.3 | 96.6 | 250 | 25.7 | 224.3 | 89.7 |
| IFV | 206,252 | 52,103 | 154,149 | 74.7 | 15,784 | 4,439 | 11,345 | 71.9 | 190,468 | 47,665 | 142,804 | 75.0 |
2018–2019: before-COVID-19, 2020–: during COVID-19. 2018–2019 (n=24; 12 months in each year), 2020–2021.4.24 (n=16; 12 months in 2020+4 months in 2021). The number of infection cases of the 8 viral acute respiratory viruses was obtained according to the Health Insurance Review and Assessment Service with residential and columnar disease diagnostic codes.
COVID-19, coronavirus disease 2019; ADV, adenovirus; HBoV, human bocavirus; HRV, human rhinovirus; HMPV, metapneumovirus; RSV, respiratory syncytial virus; HCoV, human coronavirus; HPIV, parainfluenza virus; IFV, influenza virus.
a) Difference: absolute difference.
b) Difference (%): relative change {(2018–2019)–(2020–)}/(2018–2019)×100.
- 1. Jeong SY, Lee GH, Park SJ, et al. Results of the national respiratory infectious disease surveillance, 2020. Public Health Wkly Rep 2021;14:1145−9. Korean.
- 2. World Health Organization (WHO). Operational considerations for case management of COVID-19 in health facility and community: interim guidance [Internet]. Geneva: WHO; 2020 [cited 2022 Mar 15]. Available from: https://www.who.int/publications/i/item/10665-331492.
- 3. Baek S, Park K, Lee E, et al. Results of the national infectious disease surveillance, from January to April 2020. Public Health Wkly Rep 2020;13:1498−502. Korean.
- 4. Lee H, Lee H, Song KH, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis 2021;73:e132−40.ArticlePubMedPMCPDF
- 5. Hsieh CC, Lin CH, Wang WYC, et al. The outcome and implications of public precautionary measures in Taiwan-declining respiratory disease cases in the COVID-19 pandemic. Int J Environ Res Public Health 2020;17:4877. ArticlePubMedPMC
- 6. Seasonality of respiratory viral infections. Annu Rev Virol 2020;7:83-101.
- 7. Jang SY, Seon JY, Yoon SJ, et al. Comorbidities and factors determining medical expenses and length of stay for admitted COVID-19 patients in Korea. Risk Manag Healthc Policy 2021;14:2021−33.ArticlePubMedPMCPDF
- 8. Yum S, Hong K, Sohn S, et al. Trends in viral respiratory infections during COVID-19 pandemic, South Korea. Emerg Infect Dis 2021;27:1685−8.ArticlePubMedPMC
- 9. Yum S, Hong K, Kim J, et al. Impact of the COVID-19 pandemic on other respiratory virus outbreaks [Preprint]. Posted 2020 Nov 18. Research Square. https://doi.org/10.21203/rs.3.rs-110941/v1.
- 10. Leung NH, Chu DK, Shiu EY, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 2020;26:676−80.ArticlePubMedPMCPDF
- 11. Jefferson T, Jones MA, Al-Ansari L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 1-Face masks, eye protection and person distancing: systematic review and meta-analysis [Preprint]. Posted 2020 Apr 7. medRxiv 2020.03.30.20047217. https://doi.org/10.1101/2020.03.30.20047217.
- 12. Greenhalgh T, Schmid MB, Czypionka T, et al. Face masks for the public during the covid-19 crisis. BMJ 2020;369:m1435. ArticlePubMed
- 13. World Health Organization (WHO). Interim recommendations on obligatory hand hygiene against transmission of COVID-19 [Internet]. Geneva: WHO; 2020 [cited 2022 Mar 15]. Available from: https://www.who. int/publications/m/item/interim recommendations on obligatory hand hygiene against transmission of covid-19.
- 14. Seo MR, Kim JW, Park EJ, et al. Recommendations for the management of patients with systemic rheumatic diseases during the coronavirus disease pandemic. Korean J Intern Med 2020;35:1317−32.ArticlePubMedPMCPDF
- 15. Choi S, Ki M. Analyzing the effects of social distancing on the COVID-19 pandemic in Korea using mathematical modeling. Epidemiol Health 2020;42:e2020064.ArticlePubMedPMC
- 16. Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ 2021;375:e068302.ArticlePubMed
- 17. Jehn M, Mac McCullough J, Dale AP, et al. Association between K-12 school mask policies and school-associated COVID-19 outbreaks: Maricopa and Pima Counties, Arizona, July-August 2021. MMWR Morb Mortal Wkly Rep 2021;70:1372−3.ArticlePubMedPMC
- 18. Sakudo A, Yamashiro R, Haritani M, et al. Inactivation of non-enveloped viruses and bacteria by an electrically charged disinfectant containing meso-structure nanoparticles via modification of the genome. Int J Nanomedicine 2020;15:1387−95.PubMedPMC
- 19. Ljubin-Sternak S, Mestrovic T, Luksic I, et al. Seasonal coronaviruses and other neglected respiratory viruses: a global perspective and a local snapshot. Front Public Health 2021;9:691163. ArticlePubMedPMC
- 20. Smith JG, Wiethoff CM, Stewart PL, et al. Adenovirus. In: Johnson JE, editor. Cell entry by non-enveloped viruses. Berlin: Springer Science & Business Media; 2010. p. 195-224.
- 21. Guido M, Tumolo MR, Verri T, et al. Human bocavirus: current knowledge and future challenges. World J Gastroenterol 2016;22:8684−97.ArticlePubMedPMC
- 22. Blaas D, Fuchs R. Mechanism of human rhinovirus infections. Mol Cell Pediatr 2016;3:21. ArticlePubMedPMCPDF
- 23. Castano N, Cordts SC, Kurosu Jalil M, et al. Fomite transmission, physicochemical origin of virus-surface interactions, and disinfection strategies for enveloped viruses with applications to SARS-CoV-2. ACS Omega 2021;6:6509−27.ArticlePubMedPMCPDF
- 24. Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol 2007;73:1687−96.ArticlePubMedPMCPDF
- 25. Lin Q, Lim JYC, Xue K, et al. Sanitizing agents for virus inactivation and disinfection. View (Beijing) 2020 May 24 [Epub];http://doi.org/10.1002/viw2.16.Article
- 26. Yoo JH. Review of disinfection and sterilization: back to the basics. Infect Chemother 2018;50:101−9.ArticlePubMedPMCPDF
- 27. Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev 2004;17:863−93.ArticlePubMedPMCPDF
- 28. Escudero D, Boga JA, Fernandez J, et al. SARS-CoV-2 analysis on environmental surfaces collected in an intensive care unit: keeping Ernest Shackleton's spirit. Intensive Care Med Exp 2020;8:68. ArticlePubMedPMC
- 29. Noh JY. Characteristics of viruses and the infection control. Korean J Healthc Assoc Infect Control Prev 2020;25:100−4. Korean.Article
- 30. Sattar SA. Microbicides and the environmental control of nosocomial viral infections. J Hosp Infect 2004;56 Suppl 2:S64−9.ArticlePubMedPMC
- 31. Kim JA, Yoon S, Kim LY, et al. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA Data. J Korean Med Sci 2017;32:718−28.ArticlePubMedPMCPDF
References
Figure & Data
References
Citations

- Machine learning forecasts for seasonal epidemic peaks: Lessons learnt from an atypical respiratory syncytial virus season
Roger A. Morbey, Daniel Todkill, Conall Watson, Alex J. Elliot, André Ricardo Ribas Freitas
PLOS ONE.2023; 18(9): e0291932. CrossRef


 PubReader
PubReader Cite
Cite


