Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 7(2); 2016 > Article
-
Original Article
Rapid Detection of Rifampicin- and Isoniazid-ResistantMycobacterium tuberculosis using TaqMan Allelic Discrimination - Davood Darban-Sarokhalila, Mohammad J. Nasirib, Abbas A.I. Fooladic, Parvin Heidariehd, Mohammad M. Feizabadie
-
Osong Public Health and Research Perspectives 2016;7(2):127-130.
DOI: https://doi.org/10.1016/j.phrp.2016.01.003
Published online: April 6, 2016
aDepartment of Microbiology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
bDepartment of Microbiology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
cApplied Microbiology Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
dDepartment of Microbiology, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran
eDepartment of Microbiology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
- ∗Corresponding author. mfeizabadi@tums.ac.ir
• Received: November 24, 2015 • Revised: December 27, 2015 • Accepted: January 6, 2016
Copyright © 2016 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- Multidrug-resistant tuberculosis (MDR-TB) is a global problem that many countries are challenged with. Rapid and accurate detection of MDR-TB is critical for appropriate treatment and controlling of TB. The aim of the present study was to evaluate the TaqMan allelic discrimination without minor groove binder (MGB) as a rapid, efficient, and low-cost method for detection of drug resistant strains of Mycobacterium tuberculosis.
-
Methods
- A total of 112 M. tuberculosis isolates from cases with diagnosed TB were subjected to drug susceptibility testing (DST), using the proportion method. Resistant isolates were tested for characterization of mutations in the rpoB and KatG genes by TaqMan genotyping.
-
Results
- Of 112 M. tuberculosis isolates for which DST was performed, three, one, and two isolates were MDR, rifampin (RIF) resistant, and isoniazid (INH) resistant, respectively. According to the threshold cycle (Ct) and curve pattern of mutants, TaqMan probes detect all of the mutations in the analyzed genes (katG 315, AGC→ACC, rpoB 531, TCG→TTG, and rpoB 531, TCG→TGG).
-
Conclusion
- The present study suggests that drug-resistant strains of M. tuberculosis can be detected by pattern’s curve or Ct with TaqMan probes without MGB in real-time polymerase chain reaction (PCR).
- Multidrug-resistant tuberculosis (MDR-TB) is a global problem that many countries are challenged with. MDR-TB is caused by strains of Mycobacterium tuberculosis resistant to at least isoniazid (INH) and rifampin (RIF), the main first-line anti-TB drugs [1]. Rapid and accurate detection of MDR isolates is critical for appropriate treatment and controlling of TB 2, 3, 4. The culture method is still the “gold standard” among other drug susceptibility testing methods of M. tuberculosis isolates. However, this method is time consuming and takes several weeks to be completed. In recent years, several molecular methods have been developed for detection of mutations in rpoB and katG genes that cause resistance to INH and RIF 5, 6, 7. Of these methods, Cepheid Xpert MTB/RIF kit and the line probe assays have been commercialized 8, 9. They give users the opportunity to detect the resistant mutants rapidly, but at very high cost. Therefore, it is not possible, particularly in developing countries, to apply these methods extensively. Thus, researches have been concentrated to introduce the in-house methods to reduce the cost.
- TaqMan allelic discrimination is a new technique for detection of mutations. In this method, mutations even single nucleotide polymorphisms (SNP) are detected using TaqMan probe with Minor Groove Binder (MGB) and AmpliTaq Gold DNA polymerase. The efficiency of probe hybridization reduces whenever there are mismatches between a probe and allele. Moreover, AmpliTaq Gold DNA polymerase is more likely to displace the mismatched probe rather than cleave it to release reporter dye. Recently, Wada et al [10] used TaqMan minor groove binder (MGB) probes for detection of mutations in rpoB, katG, and embB genes of M. tuberculosis.
- In this study, we designed the primers and probes for 81-bp hot spot of the rpoB gene and codon 315 of katG gene. Unlike most researches that used the TaqMan allelic discrimination, we did not use the MGB for designing of probes.
- Our main purpose was to evaluate TaqMan allelic discrimination without minor groove binder (MGB) for rapid detection of drug-resistant strains of M. tuberculosis.
Introduction
- 2.1 Setting
- This study was performed at the Tehran University of Medical Sciences. A total of 112 isolates of M. tuberculosis cultured from TB patients were included in this survey.
- 2.2 Drug susceptibility testing (DST)
- Drug resistant isolates were identified among 112 isolates using proportion method on Lowenstein–Jensen (LJ) media [11].
- 2.3 DNA extraction
- DNA was extracted from the bacterial colonies according to the method of van Soolingen et al [12]. A commercial DNA extraction kit (Invitek, Germany) was used for extraction of DNA from clinical specimens. The optical density of extracted DNA from standard strain and clinical specimens was determined at 260 nm using NanoDrop 1000 (Thermo Scientific, USA).
- 2.4 TaqMan analysis
- TaqMan probes and primers for detection of mutations in rpoB and katG genes were designed using the Primer Express program (Applied Biosystems, Foster City, CA, USA) and were synthesized by Metabion (Martinsried, Germany). The primers and probes of rpoB gene were F: 5′-TCACACCGCAGACGTTGATC-3′, R: 5′-CGTAGTGCGACGGGTGC-3′, P1: 5′-FAM-CAGCTGAGCCAATTCATGGACCAGA-BHQ-1-3′ (Tm = 67.2), and P2: 5′-VIC-CACAAGCGCCGACTGTCGGC-BHQ-1-3′ (Tm = 68.1). The primers and probe of katG gene were F: 5′-GGGCTTGGGCTGGAAGA-3′, R: 5′-GGAAACTGTTGTCCCATTTCG-3′, and P: 5′-FAM-ACGCGATCACCAGCGGCA-BHQ-1-3′ (Tm = 65.0).
- The PCR reaction mixture was 1 × reaction buffer [50 mM KCl, 10 mM Tris-HCl (pH 9.0), 2 mM MgCl2], 2.5 mM of dNTPs, 2 U Taq DNA-polymerase (miTaq, Metabion, Martinsried, Germany), and 20 pmol each of primers in total volume of 50 μL. Amplification was performed in a Mastercycler Gradient (Eppendorf, Germany) using the following program: initial denaturation at 95°C for 10 minutes and 35 cycles of denaturation at 94°C for 25 seconds, annealing at 60°C for 30 seconds, and extension at 72°C for 30 seconds, and the final extension at 72°C for 5 minutes. After amplification, PCR products were sequenced.
- The mixture of real-time PCR reaction was done using TaqMan Genotyping Master Mix (Applied Biosystems) and the mentioned primers and probes. The real-time PCR apparatus (Bioer, Hangzhou, and P.R., China) was programmed as follows: initial denaturation at 94°C for 10 minutes followed by 40 cycles of 94°C for 25 seconds, 60°C for 55 seconds. To obtain reproducibility of reaction, the amplification was run in triplicate on DNA obtained from H37Rv strain, mycobacterial isolates, and clinical samples. All samples were run with the DNA obtained from H37Rv strain. Human white blood cell DNA and beta actin gene were used as external and internal controls, respectively [13]. Diluted DNA of H37Rv was used for the evaluation of the sensitivity. Specificity of the reaction was evaluated on DNA from other mycobacteria and potentially pathogenic bacteria in the respiratory tract and human cells that was used in the previous study [14].
Materials and methods
- Of 112 isolates, three, one, and two were MDR, RIF resistant and INH resistant, respectively. The results of sequencing of rpoB and katG genes are shown in Table 1. Fig. 1 shows the analysis of DNA from mycobacteria with TaqMan probes. As described above, AmpliTaq Gold DNA polymerase could detect the mismatches between a probe and allele even SNP. According the figure, the pattern curve of H37Rv strain is different from the mutants. Moreover, the luminescence intensity or threshold cycle (Ct) was higher when mutations were present in the genes. The difference of curve patterns can differentiate the susceptible and resistance isolates. Therefore real-time PCR detected the all of the mutations in rpoB and katG genes.
- With the exception of M. tuberculosis complex (M. bovis, M. bovis, BCG, M. africanum, and M. microti), no luminescence was found. The results of PCR in serial dilutions demonstrated high efficiency of the technique as it detected 10 pg of M. tuberculosis DNA.
Results
- Real-time PCR system in combination with MGB probes has been applied to analyze single-nucleotide polymorphisms 10, 15. The MGB probes have been used in other studies for detection and distinction of one-base mismatches due to their high specificity and sensitivity [16], so it can be a powerful tool for control of drug-resistant M. tuberculosis. In this study, we developed a rapid, efficient, and low-cost real-time PCR-based system without MGB probes for detection of the mutations associated with INH and RIF resistance in M. tuberculosis.
- Despite our probes detecting all mutations in the mentioned regions of the katG and rpoB genes as little as 3 hours from the preparation of DNAs from clinical samples, our method had limitation in use because it could not identify MDR and XDR strains that genetically belonged to the Harrlem3 and Harrlem4 clusters in spoligotyping. Interestingly, there were no mutations in the 81-bp hot spot of the rpoB gene and codon 315 of katG gene of these strains as determined by DNA sequencing (data not shown). Therefore, the result of this study gives evidence that a single molecular method for detection of drug-resistant M. tuberculosis is not sufficient. In comparison with the conventional and commercial methods (i.e., line probes or Cepheid Xpert MTB/RIF kit) for detection of MDR-TB, our in-house technique was less time- and fund-consuming, with costs five times cheaper than commercial kits.
- Many studies used real-time PCR for detection of mutations in rpoB and katG genes 17, 18, 19, 20, 21 but, to our knowledge, this study is the first one that uses the TaqMan allelic discrimination without MGB. Our study suggests that drug-resistant M. tuberculosis can be detected by pattern's curve or Ct with TaqMan probes without MGB in real-time PCR. We evaluated our probes on limited resistant M. tuberculosis isolates (katG 315, AGC→ACC, rpoB 531, TCG→TTG and rpoB 531, TCG→TGG), and the mentioned mutations are the common mutations that cause RIF- and INH-resistant strains. However, for more confirmation, evaluation of other mutations in the 81-bp hot spot of the rpoB gene as well as more drug-resistant strains is needed.
Discussion
- All authors have no conflicts of interest to declare.
Conflicts of interest
-
Acknowledgements
- This work is a part of project 9627 supported by Tehran University of Medical Sciences.
Acknowledgments
- 1. Nasiri M.J., Dabiri H., Darban-Sarokhalil D.. Prevalence of drug-resistant tuberculosis in Iran: systematic review and meta-analysis. Am J Infect Control 42(11). 2014 Sep;1212−1218. PMID: 25242634.ArticlePubMed
- 2. Adékambi T., Colson P., Drancourt M.. rpoB-based identification of nonpigmented and late-pigmenting rapidly growing mycobacteria. J Clin Microbiol 41(12). 2003 Dec;5699−5708. PMID: 14662964.ArticlePubMed
- 3. Palomino J.C.. Molecular detection, identification, and drug resistance detection in Mycobacterium tuberculosis. FEMS Immunol Med Microbiol 56(2). 2009 Jul;103−111. PMID: 19416361.ArticlePubMed
- 4. Catanzaro A., Rodwell T.C., Catanzaro D.G.. Performance comparison of three rapid tests for the diagnosis of drug-resistant tuberculosis. PLoS One 10(8). 2015 Aug 31;e0136861PMID: 26322781.Article
- 5. Marín M., De Viedma D.G., Ruíz-Serrano M.J.. Rapid direct detection of multiple rifampin and isoniazid resistance mutations in Mycobacterium tuberculosis in respiratory samples by real-time PCR. Antimicrob Agents Chemother 48(11). 2004 Nov;4293−4300. PMID: 15504855.ArticlePubMed
- 6. Sali M., De Maio F., Caccuri F.. Multicenter evaluation of the Anyplex Plus MTB/NTM MDR-TB assay for rapid detection of Mycobacterium tuberculosis complex and multidrug-resistant isolates in pulmonary and extrapulmonary specimens. J Clin Microbiol 2015 Oct;pii: JCM.01904-15.
- 7. Mani V., Wang S., Inci F.. Emerging technologies for monitoring drug-resistant tuberculosis at the point-of-care. Adv Drug Deliv Rev 78:2014 Nov;105−117. PMID: 24882226.ArticlePubMed
- 8. Boehme C.C., Nabeta P., Hillemann D.. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med 363(11). 2010 Sep;1005−1015. PMID: 20825313.ArticlePubMed
- 9.
- 10. Wada T., Maeda S., Tamaru A.. Dual-probe assay for rapid detection of drug-resistant Mycobacterium tuberculosis by real-time PCR. J Clin Microbiol 42(11). 2004 Nov;5277−5285. PMID: 15528726.ArticlePubMed
- 11. Nasiri M.J., Rezaei F., Zamani S.. Drug resistance pattern of Mycobacterium tuberculosis isolates from patients of five provinces of Iran. Asian Pac J Trop Med 7(3). 2014 Mar;193−196. PMID: 24507638.ArticlePubMed
- 12. van Soolingen D., De Haas P.E., Hermans P.W.. DNA fingerprinting of Mycobacterium tuberculosis. Methods Enzymol 235:1994;196−205. PMID: 8057895.ArticlePubMed
- 13. Mehndiratta M., Palanichamy J.K., Ramalingam P.. Fluorescence acquisition during hybridization phase in quantitative real-time PCR improves specificity and signal-to-noise ratio. Biotechniques 45(6). 2008 Dec;625−626. PMID: 19238793.ArticlePubMed
- 14. Darban-Sarokhalil D., Fooladi A., Bameri Z.. Cytochrome CYP141: a new target for direct detection of Mycobacterium tuberculosis from clinical specimens. Acta Microbiol Immunol Hung 58(3). 2011 Sep;211−217. PMID: 21983322.ArticlePubMed
- 15. van Doorn H.R., Claas E.C., Templeton K.E.. Detection of a point mutation associated with high-level isoniazid resistance in Mycobacterium tuberculosis by using real-time PCR technology with 3′-minor groove binder-DNA probes. J Clin Microbiol 41(10). 2003 Oct;4630−4635. PMID: 14532194.ArticlePubMed
- 16. Kutyavin I.V., Afonina I.A., Mills A.. 3′-Minor groove binder-DNA probes increase sequence specificity at PCR extension temperatures. Nucleic Acids Res 28(2). 2000 Jan 15;655−661. PMID: 10606668.Article
- 17. de Viedma D.G., Infantes MdSD., Lasala F.. New real-time PCR able to detect in a single tube multiple rifampin resistance mutations and high-level isoniazid resistance mutations in Mycobacterium tuberculosis. J Clin Microbiol 40(3). 2002 Mar;988−995. PMID: 11880428.ArticlePubMed
- 18. Ramirez M.V., Cowart K.C., Campbell P.J.. Rapid detection of multidrug-resistant Mycobacterium tuberculosis by use of real-time PCR and high-resolution melt analysis. J Clin Microbiol 48(11). 2010 Nov;4003−4009. PMID: 20810777.ArticlePubMed
- 19. Haeili M., Fooladi A., Bostanabad S.. Rapid screening of rpoB and katG mutations in Mycobacterium tuberculosis isolates by high-resolution melting curve analysis. Indian J Med Microbiol 32(4). 2014 Oct–Dec;398−403. PMID: 25297024.ArticlePubMed
- 20. Choi G.E., Lee S.M., Yi J.. High-resolution melting curve analysis for rapid detection of rifampin and isoniazid resistance in Mycobacterium tuberculosis clinical isolates. J Clin Microbiol 48(11). 2010 Nov;3893−3898. PMID: 20844231.ArticlePubMed
- 21. Park S.-H., Kim C.-K., Jeong H.-R.. Evaluation and comparison of molecular and conventional diagnostic tests for detecting tuberculosis in Korea, 2013. Osong Public Health Res Perspect 5(Suppl.). 2014 Dec;S3−S7. PMID: 25861577.ArticlePubMed
References
Figure 1The curve patterns of H37Rv strain, negative control and Mycobacterium tuberculosis mutants with and without katG 315, AGC→ACC mutation.
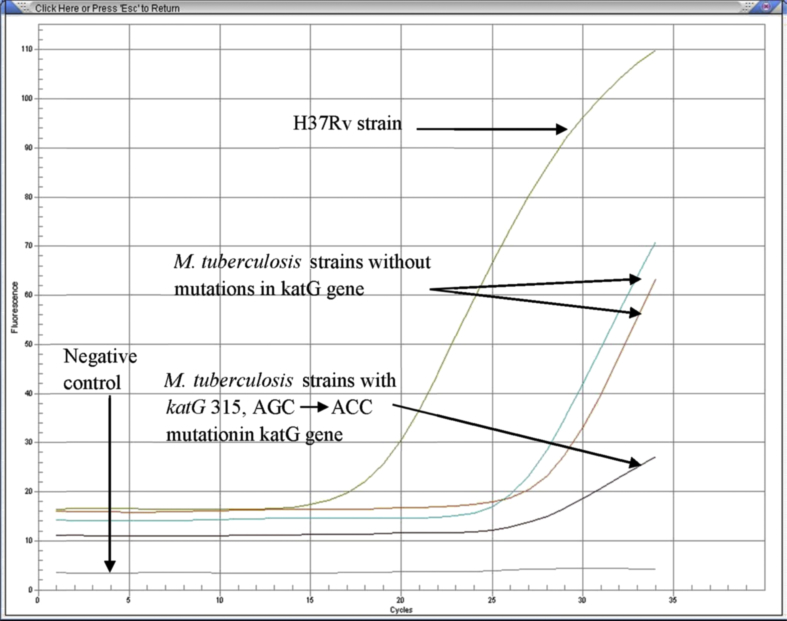
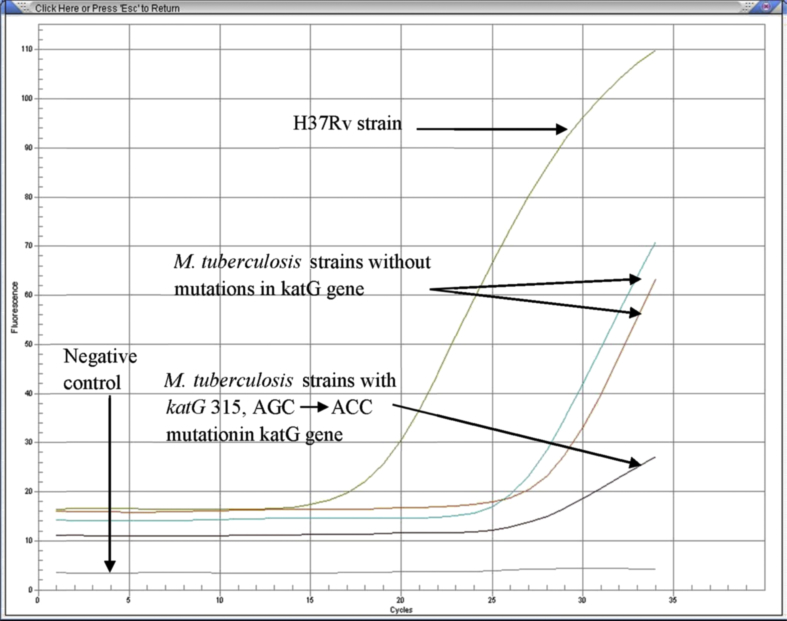
Figure & Data
References
Citations
Citations to this article as recorded by 

- Drug resistance and the genotypic characteristics of rpoB and katG in rifampicin- and/or isoniazid-resistant Mycobacterium tuberculosis isolates in central Vietnam
Thi Binh Nguyen Nguyen, Thi Kieu Diem Nguyen, Van Hue Trương, Thi Tuyet Ngoc Tran, van Bao Thang Phan, Thi Tuyen Nguyen, Hoang Bach Nguyen, Viet Quynh Tram Ngo, Van Tuan Mai, Paola Molicotti
Osong Public Health and Research Perspectives.2023; 14(5): 347. CrossRef - The Value of the inhA Mutation Detection in Predicting Ethionamide Resistance Using Melting Curve Technology
Yanhua Song, Guirong Wang, Qiang Li, Rongmei Liu, Liping Ma, Qi Li, Mengqiu Gao
Infection and Drug Resistance.2021; Volume 14: 329. CrossRef


 PubReader
PubReader Cite
Cite
