Articles
- Page Path
- HOME > Osong Public Health Res Perspect > Volume 6(6); 2015 > Article
-
Original Article
Epidemiological Characterization of Skin Fungal Infections Between the Years 2006 and 2010 in Korea - Sang-Ha Kima, Seung-Hak Chob, Seung-Ki Younc, Je-Seop Parka, Jong Tae Choid, Young-Seok Bake, Young-Bin Yua, Young Kwon Kima
-
Osong Public Health and Research Perspectives 2015;6(6):341-345.
DOI: https://doi.org/10.1016/j.phrp.2015.10.012
Published online: November 10, 2015
aDepartment of Biomedical Laboratory Science, College of Medical Sciences, Konyang University, Daejeon, Korea
bDivision of Enteric Diseases, Center for Infectious Diseases, Korea National Institute of Health, Cheongju, Korea
cDivision of Quarantine Support, Korea Centers for Disease Control and Prevention, Cheongju, Korea
dDepartment of Biomedical Laboratory Science, Kyungdong University, Wonju, Korea
eDepartment of Emergency Medical Service, College of Medical Sciences, Konyang University, Daejeon, Korea
- ∗Corresponding author. ykkim3245@konyang.ac.kr
Copyright © 2015 Korea Centers for Disease Control and Prevention. Published by Elsevier Korea LLC. All rights reserved.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abstract
-
Objectives
- The purpose of this study was to build and provide a basic database of skin fungal infections for the effective management of skin fungal infections in the future.
-
Methods
- We collected health insurance data between the years 2006 and 2010 from the Health Insurance Corporation (Seoul, Korea) and analyzed the data to determine the prevalence and treatment management of skin fungal infections.
-
Results
- Skin fungal infections were divided into two groups: namely dermatophytosis and other superficial mycoses. Dermatophytosis showed a higher prevalence (16,035,399 cases) than the other superficial mycoses (794,847 cases) within the study period. The prevalence rate decreased consecutively by 0.01% to 0.19% every year. The prevalence according to region showed that Jeolla-do had a high prevalence distribution. The prevalences in men and women were similar (7.01% vs. 6.26%). It is interesting to note that adults from the 50–79-year age group showed a higher prevalence than children and young adults. The average convalescence time (days) of dermatophytosis was longer than that of other superficial mycoses. The total medical expenses were also much higher in dermatophytosis than in the other superficial mycoses.
-
Conclusion
- This study provides useful data for study trends of skin fungal infections.
- Fungal infections of the skin, hair, and nails are a common public health problem worldwide. However, a population-based survey reported that they are rarely managed [1]. The prevalence of skin fungal infections is expected to reach 20–25% of the world's population, and its incidence continues to increase 2, 3 and accounts for 10–20% of all dermatologic outpatients in South Korea [4]. This increase may be a result of usage of antibiotics and immunosuppressive drugs [5].
- Skin fungal infections are caused mainly by dermatophytes such as Trichophyton, Microsporum, and Epidermophyton that can invade the stratum corneum and keratinized tissues 6, 7. Skin fungal infections are less frequently caused by nondermatophyte fungi (e.g., Malassezia in tinea versicolor) [7].
- Dermatophytoses are referred to as tinea infections and can be classified according to the body site involved [8]. These infections are typically acquired directly from contact with infected humans or animals or indirectly from exposure to contaminated soil or fomites.
- The lipophilic yeast Malassezia is a normal microflora of the human skin that may be pathogenic under certain conditions. Malassezia species cause the most human skin infections, and is the most common cause of dandruff, seborrhoeic dermatitis, folliculitis, papillomatosis, and tinea (pityriasis) versicolor 9, 10, 11, 12, 13. However, the exact species implicated still remains unclear [14].
- The prevalence of skin fungal infection differs by social, geographic, economical status, and life environment. According to Korean research studies on skin fungal infections (trichophytosis), 5.2% of total outpatients had trichophytosis in the survey of Yonsei University Severance Hospital, Seoul, Korea from 1937 to 1946 [15]. Skin infections are known to spread not only in the patient but also to the patient's family members.
- Skin fungal infections induced by fungal agents may have side effects caused by antifungal reagents and increases medical fees and social costs if not treated quickly in the early stage. However, research on the nationwide developmental distribution and epidemiological characteristics of skin fungal infections is rare. Therefore, this study aimed to build a basic database for effective fungal infection control by examining age, sex, year, distribution, and prevalence by region, medical care institution, and treatment costs over 5 years, from 2006 to 2010, by using the database of the Health Insurance Corporation (Seoul, Korea) to research the epidemiological characteristics of skin fungal infections.
Introduction
- 2.1 Data collection and study design
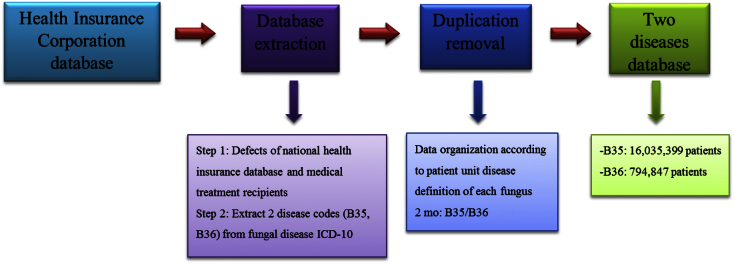
- The individuals of the research were health insurance recipients over 5 years, from January 1, 2006 to December 30, 2010. The only information on skin fungal infection was extracted from all cases of fungal infections and collected data, and was divided into dermatophytosis (Korea International Classification of Diseases: B35) and other superficial mycoses (B36).
- In cases of skin fungal infection, in order to avoid duplication, a new case was defined when new treatment was administered for 2 months after the last treatment date (Figure 1). The collected data were analyzed by using the SPSS version 20.0 software (SPSS Inc., Chicago, IL, USA) after entering into an Excel sheet with encoding.
- 2.2 Epidemiological investigations
- In order to determine the significance of skin fungal infections that cause diseases, we performed an epidemiological analysis of variables such as seasonal and regional prevalences and age- and gender-specific patterns of the prevalences of dermatophytosis and other superficial mycoses.
- 2.3 Calculation of convalescence days and medical treatments for therapy
- The convalescence days of the in- and outpatients for skin fungal infections and superficial mycosis were calculated for the previous 5 years. Medical care costs were calculated by classifying into personal and insurance charges from the insurance items in the Health Insurance Corporation database. No insurance charge items were excluded from the medical care costs.
Materials and methods
- Among the skin fungal infections, dermatophytosis showed a higher prevalence (16,035,399 cases) than the other superficial mycoses (794,847 cases) between the years 2006 and 2010. Here, we describe the epidemiological characterization of and medical treatments for patients infected with skin fungal infections during the past 5 years in South Korea.
- 3.1 Epidemiological characterization of skin fungal infections
- As shown in Table 1, the prevalence rate of dermatophytosis, according to resident population, consecutively decreased by 0.01% to 0.19% from the years 2006 to 2010. The regional prevalence was highest in Jeollanam-do at 7.98% and the lowest in Incheon at 5.96%.
- The prevalences of the other superficial mycoses also decreased gradually every year. The yearly prevalence based on registered population information showed a 0.01% decrease in prevalence rate, the rate being 0.35% by resident population in 2006 and 0.31% in 2010. The regional prevalence showed that Jeonbuk (0.41%) had the highest prevalence and Jeju (0.26%) had the lowest prevalence (Table 1).
- As shown in Table 2, the prevalences in men and women were similar; although in men it was slightly higher than that in women (7.01% vs. 6.26%). Age-specific patterns were observed in the occurrence of skin fungal infections, with a high prevalence rate in older adults, especially in people from the 50–79-years age group, but a low prevalence rate in children and young adults (Table 2).
- 3.2 Medical treatments of patients by skin fungal infections
- The average convalescence time (days) of dermatophytosis was longer than that of other superficial mycoses. The average convalescence time of dermatophytosis was 26.9 days for inpatients and 2.51 days for outpatients. The average convalescence time of the other superficial mycoses was 19.9 days for inpatients and 1.80 days for outpatients (Table 3).
- The total medical costs of dermatophytosis were higher than those of the other superficial mycoses. The total medical cost for inpatients and outpatients was 5,332 hundred million won, 441 hundred million won for hospitalization, and 4,891 hundred million won for outpatient medical costs. Of the total medical costs for the other superficial mycoses, 9 hundred million won was for inpatients and 175 hundred million won was for outpatients (Table 3).
Results
- Skin fungal infections occur because of fungal agents invading the skin [6], causing superficial lesions with fungus parasitic on the stratum corneum of the skin, hair, nails, and toenails, and skin candidiasis. Skin fungal infection is a common disease in South Korea, affecting 10–20% of dermatology outpatients 16, 17. The World Health Organization estimates the global prevalence of dermatophytoses to be approaching 20% [18].
- Dermatophytes are the only fungal agents that have evolved a dependency on human or animal infection for survival. The infection may spread from person to person (anthropophilic), animal to person (zoophilic), or soil to person (geophilic) [19].
- The distribution of skin fungal infections and their causative agents vividly differ between geographical, climatic factor, and cultural requirements, and also show differences in changes in lifestyle, habit, sanitary thought, and socioeconomic status, as well as frequent interchange, trade, and human immigration 3, 20, 21.
- According to the retrospective analysis from 2005 to 2010 of Vena et al [22], the most prevalent clinical form was tinea ungium (39.2% of the total dermatophytoses) and Trichophyton rubrum was the most prevalent causative agent, implicated in 64% of the total cases. Epidemiological data showed gradual decreases in the prevalences of tinea cruris, tinea corporis, and tinea capitis infections over time. However, the prevalence rates of tinea pedis and tinea ungium have significantly increased.
- In South Korea, many lifestyle changes have occurred since the social changes after the liberation occurred in the past 60 years, which took 100–150 years in Europe and the United States [23]. The prevalences of many diseases have changed along with the lifestyle changes in South Korea. In particular, the isolation frequency of fungal species that cause skin fungal infection has largely changed. New fungal species have been transmitted from foreign countries, or the number of fungal species with high isolation frequency were reduced 4, 16, 17, 23, 24. However, no nationwide epidemiological research on skin fungal infections have been conducted that involve clinical mycological observation and causative organism identification in patients with skin fungal infection patients 25, 26.
- The aim of this study was to analyze the epidemiological characteristics of skin fungal infections that occurred between 2006 and 2010. We collected data from the Health Insurance Corporation and analyzed two groups, namely the dermatophytosis and other superficial mycosis groups, according to similarity of fungal infection pattern. The prevalence rate of dermatophytosis decreased slightly every year between the years 2006 and 2010, whereas the prevalence rate of the other superficial mycoses was 0.3% from 2006 to 2010. This decrease in the prevalence rate of dermatophytosis is thought to be caused by the change in the hygiene concern of people.
- Of the total medical care cost, the medical care cost for skin fungal infections was the highest at 918 hundred million won. The individual medical care cost in 2010 was 159,480 won. About 6.8% of the average population receives treatment of skin fungal infection. In particular, 0.8 in 10 people of the Korean population receives treatment for fungal infections every year, which indicates a high prevalence rate.
- For the prevalence rate according to age, the 60–70-years age group showed the highest prevalence rate, as the rate increased with age. Although data in relation to age and dermatophytosis have not yet been reported, with an aging society, epidemiological studies on chemotherapy and the increase in the incidence of metabolic diseases such as diabetes are needed. By contrast, superficial mycosis was shown to have the highest prevalence among the 20–30-years age group, with the tendency to decrease with age. Tattoo, nail art, nail care, degree of skin exposure, skin care, and so on, were thought to be influenced by the changes in sociocultural, economic, and living customs.
- The data collected from the database may not coincide 100% with clinical diagnoses for dermatophytoses and other superficial mycoses, but are greatly useful in judging changes in the prevalence of fungal infections. Yearly prevalence rates are analyzed according to socioeconomic changes. A retrospective research using data from the Health Insurance Corporation database has advantages of solving the limitation of space-time or cost, but long-term tracking observation of individual patients is difficult.
- Therefore, continuous surveillance of changes in prevalence, region of infectious disease, and epidemiological pattern over different periods is possible for pathogens of fungal infections occurring in high prevalences in South Korea. Accurate prediction of prevalence is also possible using this data collection.
Discussion
- All authors have no conflicts of interest to declare.
Conflicts of interest
-
Acknowledgements
- This work was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention (Fund code No. 2012-E2400200).
Acknowledgments
-
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License (http://creativecommons.org/licenses/by-nc-nd/4.0) which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
Article information
- 1. dos Santos M.M., Amaral S., Harmen S.P.. The prevalence of common skin infections in four districts in Tomor-Leste: a cross sectional survey. BMC Infect Dis 10:2010 Mar;61PMID: 20219136.ArticlePubMed
- 2. Male O.. The significance of mycology in medicine. Edited by Hawksworth D.L.: Frontiers in Mycology. 1990. CAB International; Wallingford: pp 131−156.
- 3. Ameen M.. Epidemiology of superficial fungal infections. Clin Dermatol 28:2010 Mar;197−201. PMID: 20347663.ArticlePubMed
- 4. Suh S.B.. Dermatophytosis and its causative agents in Korea. Korean J Med Mycol 1:1996 Dec;1−10.
- 5. Kannan P., Janaki C., Selvi G.S.. Prevalence of dermatophytes and other fungal agents isolated from clinical samples. Ind J Med Microbiol 24(3). 2006 Jul;212−215.Article
- 6. Kwon-Chung K.J., Bennett J.E.. Medical mycology. 1992. Lea & Febigger; Philadelphia: pp 105−161.
- 7. Hainer B.L.. Dermatophyte infections. Am Fam Physician 67(1). 2003 Jan;101−109. PMID: 12537173.PubMed
- 8.
- 9. Gemmer C.M., DeAngelis Y.M., Theelen B.. Fast, noninvasive method for molecular detection and differentiation of Malassezia yeast species on human skin and application of the method to dandruff microbiology. J Clin Microbiol 40:2002 Sep;3350−3357. PMID: 12202578.ArticlePubMed
- 10. Shokohi T., Afshar P., Barzgar A.. Distribution of Malassezia species in patients with pityriasis versicolor in Northern Iran. Indian J Med Microbiol 27(4). 2009 Oct-Dec;321−324. PMID: 19736400.ArticlePubMed
- 11. Prohic A., Ozegovic L.. Malassezia species isolated from lesional and non-lesional skin in patients with pityriasis versicolor. Mycoses 50(1). 2007 Jan;58−63. PMID: 17302750.ArticlePubMed
- 12. Difonzo E.M., Faggi E., Bassi A.. Malassezia skin diseases in humans. G Ital Dermatol Venereol 148(6). 2013 Dec;609−619. PMID: 24442041.PubMed
- 13. Gupta A.K., Batra R., Bluhm R.. Skin diseases associated with Malassezia species. J Am Acad Dermatol 51(5). 2004 Nov;785−798. PMID: 15523360.ArticlePubMed
- 14. Crespo-Erchiga V., Gómez-Moyano E., Crespo M.. Pityriasis versicolor and the yeast of genus Malassezia. Actas Dermosifiliogr 99:2008 Dec;764−771. PMID: 19091214.ArticlePubMed
- 15. Yang J.H.. Statistical observation of skin fungal disease for last 10 years. Korean Dermatol & Urol Society Newsletter 1:1949 Jan;10−17.
- 16. Jang S.J., Ahn K.J.. Superficial dermatomycosis and the causative agents in Korea. Korean J Med Mycol 9:2004 Aug;91−99.
- 17. Kim K.H.. Changing patterns of dermatophytosis and its causative agents according to social and economic developments in Korea. Korean J Med Mycol 11:2006 Mar;1−12.
- 18. Marques S.A., Robles A.M., Tortorano A.M.. Mycoses associated with AIDS in the third world. Med Mycology 38(1). 2000 Nov;269−279.Article
- 19. Achterman R.R., White T.C.. Dermatophyte virulence factors: Identifying and analyzing genes that may contribute to chronic or acute skin infections. Int J Microbiol 2012 Oct;ID 358305:8.Article
- 20. Lee D.K., Moon C.K., Koh J.K.. Clinical and mycological studies on superficial fungal infection. Korean J Med Mycol 11(2). 2006 Jun;54−63.
- 21. Havlickova B., Czaika V.A., Friedrich M.. Epidemiological trends in skin mycoses worldwide. Mycoses 51(Suppl.4). 2008 Sep;2−15. PMID: 18783559.ArticlePubMed
- 22. Vena G.A., Chieco P., Posa F.. Epidemiology of dermatophytoses: retrospective analysis from 2005 to 2010 and comparison with previous data from 1975. New Microbiologica 35:2012 Apr;207−213. PMID: 22707134.PubMed
- 23. Kim K.H.. Superficial cutaneous mycoses in Korea. Hanyang Med Rev 26(4). 2006 Oct;4−14.
- 24. Kim K.H., Jun J.B., Yoo H.J.. Superficial and cutaneous mycoses in Korean. Dermatology Society Publishing Committee. Dermatology revised. Ryo Moon Gak 4:2001;310−340.
- 25. Hong J.K.. A supplementary study on Tinea capitis in Taegu City. Annals Dermatol 2:1962 Dec;139−150.
- 26. Lee S.K., Choi J.S., Kim K.H.. A clinical and mycological Study of tinea pedis. Annals Dermatol 33:1995 Oct;1029−1037.
References
Figure & Data
References
Citations

- Amphotericin B-loaded natural latex dressing for treating Candida albicans wound infections using Galleria mellonella model
Rondinelli Donizetti Herculano, Camila Eugênia dos Reis, Silvia Maria Batista de Souza, Giovana Sant'Ana Pegorin Brasil, Mateus Scontri, Satoru Kawakita, Bruna Gregatti Carvalho, Camila Calderan Bebber, Yanjin Su, Ana Paula de Sousa Abreu, Marvin M Mecwan
Journal of Controlled Release.2024; 365: 744. CrossRef - Microsurgical Debridement for Persistent Ulcers Due to Rare Fungus Infection: Case Report and Literature Review
Yu-Wen Tsui, Chia-Yu Tsai, Hung-Chi Chen
Archives of Plastic Surgery.2024; 51(01): 135. CrossRef - Prevalence and antifungal drug resistance of dermatophytes in the clinical samples from Pakistan
Bakhtawar Usman, Abdul Rehman, Iffat Naz, Muhammad Anees
Acta Microbiologica et Immunologica Hungarica.2021;[Epub] CrossRef - Discovery of a novel and selective fungicide that targets fungal cell wall to treat dermatomycoses: 1,3‐bis(3,4‐dichlorophenoxy)propan‐2‐aminium chloride
Daiane Flores Dalla Lana, Stefânia Neiva Lavorato, Laura Minussi Giuliani, Letícia Cruz, William Lopes, Marilene Henning Vainstein, Igor Camargo Fontana, Aline Rigon Zimmer, Murillo de Araújo Freitas, Saulo Fernandes de Andrade, Ricardo José Alves, Alexan
Mycoses.2020; 63(2): 197. CrossRef - Voriconazole-natural latex dressings for treating infected Candida spp. skin ulcers
Thainá V da Silva, Natan R de Barros, Caroline B Costa-Orlandi, Jean L Tanaka, Lincoln G Moro, Giovana S Pegorin, Kassandra SM Oliveira, Maria JS Mendes-Gianinni, Ana M Fusco-Almeida, Rondinelli D Herculano
Future Microbiology.2020; 15(15): 1439. CrossRef - The Pathogenesis of Fungal-Related Diseases and Allergies in the African Population: The State of the Evidence and Knowledge Gaps
Lorraine Tsitsi Pfavayi, Elopy Nimele Sibanda, Francisca Mutapi
International Archives of Allergy and Immunology.2020; 181(4): 257. CrossRef - Medicinal Importance of Azo and Hippuric Acid Derivatives
Tehreem Tahir, Muhammad Ashfaq, Humna Asghar, Mirza I. Shahzad, Rukhsana Tabassum, Areeba Ashfaq
Mini-Reviews in Medicinal Chemistry.2019; 19(9): 708. CrossRef - Evaluation of antifungal activity of blended cinnamon oil and usnic acid nanoemulsion using candidiasis and dermatophytosis models
Peeyush kumar, P.W. Ramteke, Avinash C. Pandey, Himanshu Pandey
Biocatalysis and Agricultural Biotechnology.2019; 18: 101062. CrossRef - A novel approach for skin infections: Controlled release topical mats of poly(lactic acid)/poly(ethylene succinate) blends containing Voriconazole
Neslihan Üstündağ Okur, Maria Filippousi, Mehmet Evren Okur, Şule Ayla, Emre Şefik Çağlar, Ayşegül Yoltaş, Panoraia I. Siafaka
Journal of Drug Delivery Science and Technology.2018; 46: 74. CrossRef - Serious fungal infections in Korea
K. Huh, Y. E. Ha, D. W. Denning, K. R. Peck
European Journal of Clinical Microbiology & Infect.2017; 36(6): 957. CrossRef - Epidemiology of Fungal Infections in Patients Admitted via Emergency Department in Korea (2011~2013)
서영우, 장태창, 박준수
Korean Journal of Medical Mycology.2016; 21(4): 111. CrossRef


 PubReader
PubReader Cite
Cite
