Search
- Page Path
- HOME > Search
- Effects of an arteriovenous fistula stenosis prevention program in patients receiving hemodialysis
- Haegyeong Lee, Gyuli Baek, Eunju Lee
- Osong Public Health Res Perspect. 2023;14(4):279-290. Published online August 9, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0101
- 1,266 View
- 143 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 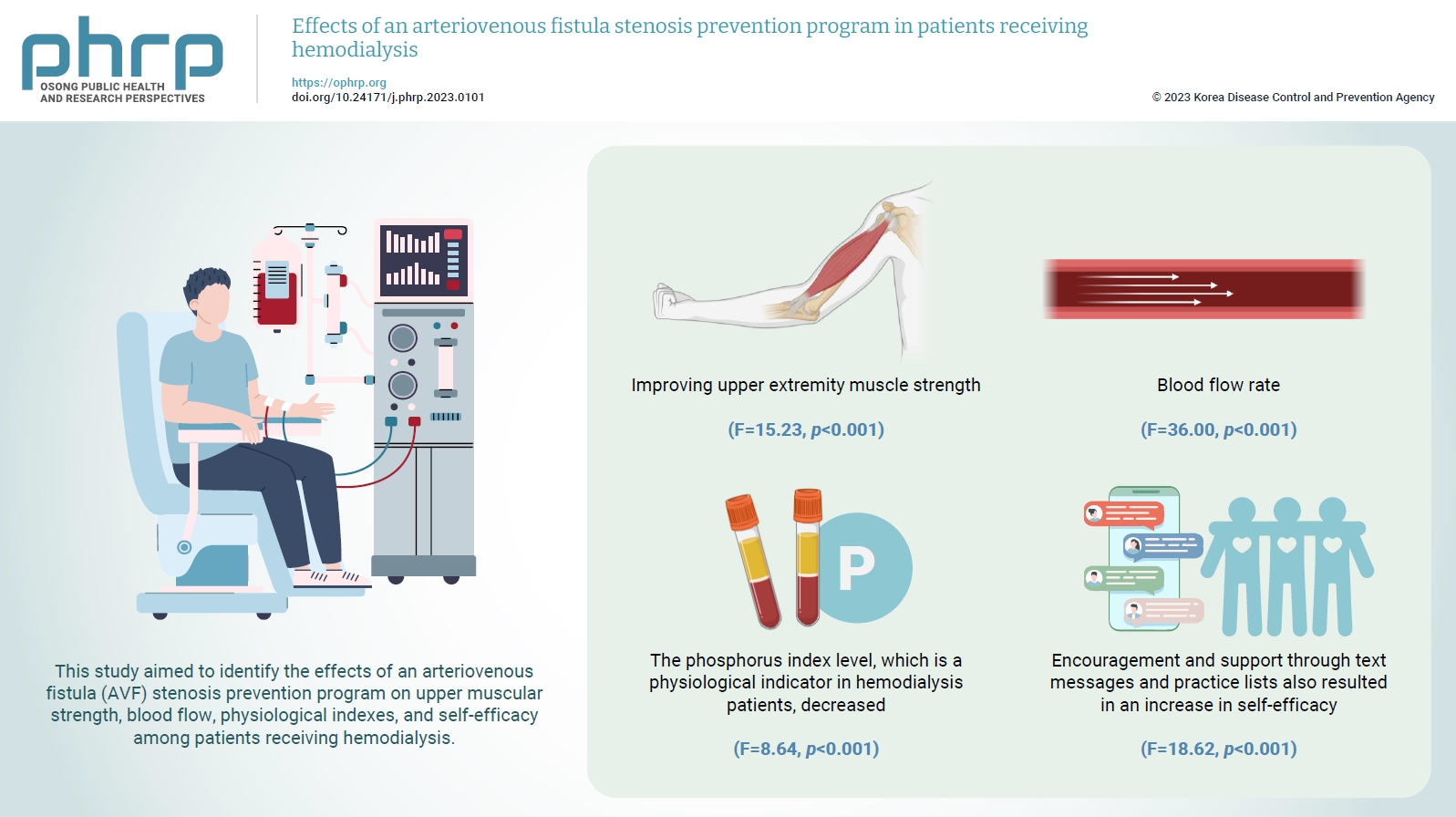
- Objectives
To increase the efficiency of hemodialysis, an appropriate vascular pathway must be created, and its function must be maintained. This study aimed to identify the effects of an arteriovenous fistula (AVF) stenosis prevention program on upper muscular strength, blood flow, physiological indexes, and self-efficacy among patients receiving hemodialysis.
Methods
The participants were patients receiving hemodialysis at Keimyung University Dongsan Medical Center in Daegu, Republic of Korea. They were divided into experimental and control groups based on the day of the week they received hemodialysis at the outpatient department and included 25 participants each. The study was conducted for 8 weeks.
Results
The AVF stenosis prevention program was effective in improving upper extremity muscle strength (F=15.23, p<0.001) and blood flow rate (F=36.00, p<0.001). As a result of the program, the phosphorus index level, which is a physiological indicator in hemodialysis patients, decreased (F=8.64, p<0.001). Encouragement and support through text messages and practice lists also resulted in an increase in self-efficacy (F=18.62, p<0.001).
Conclusion
The AVF stenosis prevention program in this study resulted in an increase in upper extremity muscle strength through grip strength exercises and was effective in preventing AVF stenosis by increasing the blood flow rate.
- The COVID-19 pandemic and healthcare utilization in Iran: evidence from an interrupted time series analysis
- Monireh Mahmoodpour-Azari, Satar Rezaei, Nasim Badiee, Mohammad Hajizadeh, Ali Mohammadi, Ali Kazemi-Karyani, Shahin Soltani, Mehdi Khezeli
- Osong Public Health Res Perspect. 2023;14(3):180-187. Published online June 22, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0041
- 1,383 View
- 67 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 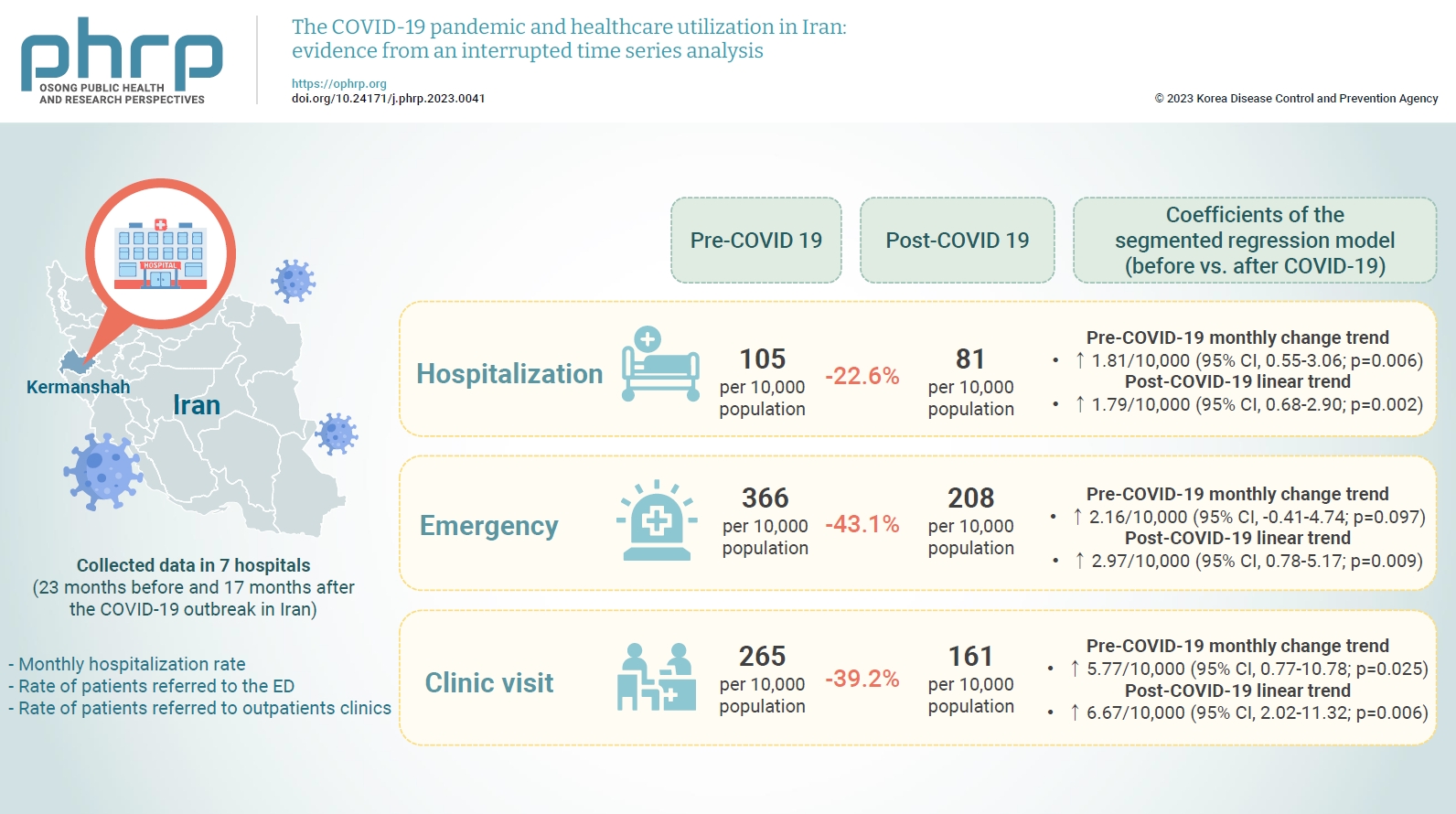
- Objectives
This study aimed to examine the effect of the coronavirus disease 2019 (COVID-19) outbreak on the hospitalization rate, emergency department (ED) visits, and outpatient clinic visits in western Iran.
Methods
We collected data on the monthly hospitalization rate, rate of patients referred to the ED, and rate of patients referred to outpatient clinics for a period of 40 months (23 months before and 17 months after the COVID-19 outbreak in Iran) from all 7 public hospitals in the city of Kermanshah. An interrupted time series analysis was conducted to examine the impact of COVID-19 on the outcome variables in this study.
Results
A statistically significant decrease of 38.11 hospitalizations per 10,000 population (95% confidence interval [CI], 24.93–51.29) was observed in the first month of the COVID-19 outbreak. The corresponding reductions in ED visits and outpatient visits per 10,000 population were 191.65 (95% CI, 166.63–216.66) and 168.57 (95% CI, 126.41–210.73), respectively. After the initial reduction, significant monthly increases in the hospitalization rate (an increase of 1.81 per 10,000 population), ED visits (an increase of 2.16 per 10,000 population), and outpatient clinic visits (an increase of 5.77 per 10,000 population) were observed during the COVID-19 pandemic.
Conclusion
Our study showed that the utilization of outpatient and inpatient services in hospitals and clinics significantly declined after the COVID-19 outbreak, and use of these services did not return to pre-outbreak levels as of June 2021.
- Epidemiological, imaging, laboratory, and clinical characteristics and factors related to mortality in patients with COVID-19: a single-center study
- Zohreh Azarkar, Hamid Salehiniya, Toba Kazemi, Hamid Abbaszadeh
- Osong Public Health Res Perspect. 2021;12(3):169-176. Published online May 26, 2021
- DOI: https://doi.org/10.24171/j.phrp.2021.0012
- 5,728 View
- 120 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Coronavirus disease 2019 (COVID-19) is a novel pandemic. Considerable differences in disease severity and the mortality rate have been observed in different parts of the world. The present study investigated the characteristics and outcomes of patients hospitalized with COVID-19 in Iran.
Methods
We established a retrospective cohort to study hospitalized COVID-19 patients in Iran. Epidemiological, imaging, laboratory, and clinical characteristics and outcomes were recorded from medical documents. The chi-square test, t-test, and logistic regression models were used to analyze the data. A p<0.05 was considered to indicate statistical significance.
Results
In total, 364 cases (207 males and 157 females) were analyzed. The most common symptoms were cough, fever, and dyspnea. Multifocal bilateral ground-glass opacities with peripheral distribution were the predominant imaging finding. The mean age of patients was 54.28±18.81 years. The mean age of patients who died was 71.50±14.60 years. The mortality rate was 17.6%. The total proportion of patients with a comorbidity was 47.5%, and 84.4% of patients who died had a comorbidity. Sex, history of diabetes mellitus, and dyslipidemia were not significantly associated with mortality (p>0.05). However, mortality showed significant relationships with body mass index; age; history of hypertension, chronic kidney disease (CKD), ischemic heart disease, cerebrovascular accident (CVA), pulmonary disease, and cancer; and abnormal high-resolution computed tomography (HRCT) findings (p<0.05 for all). Cancer had the highest odds ratio.
Conclusion
Comorbidities (especially cancer, CKD, and CVA), severe obesity, old age, and abnormal HRCT findings affected the health outcomes of patients hospitalized with COVID-19. -
Citations
Citations to this article as recorded by- Obesity as a Risk Factor for Complications and Mortality in Individuals with SARS-CoV-2: A Systematic Review
Marielle Priscila de Paula Silva-Lalucci, Déborah Cristina de Souza Marques, Pablo Valdés-Badilla, Leonardo Vidal Andreato, Braulio Henrique Magnani Branco
Nutrients.2024; 16(4): 543. CrossRef - Effects of SARS-CoV-2 infections in patients with cancer on mortality, ICU admission and incidence: a systematic review with meta-analysis involving 709,908 participants and 31,732 cancer patients
Mehmet Emin Arayici, Nazlican Kipcak, Ufuktan Kayacik, Cansu Kelbat, Deniz Keskin, Muhammed Emin Kilicarslan, Ahmet Veli Kilinc, Sumeyye Kirgoz, Anil Kirilmaz, Melih Alihan Kizilkaya, Irem Gaye Kizmaz, Enes Berkin Kocak, Enver Kochan, Begum Kocpinar, Fatm
Journal of Cancer Research and Clinical Oncology.2023; 149(7): 2915. CrossRef - Risk Factors Associated with Severity and Death from COVID-19 in Iran: A Systematic Review and Meta-Analysis Study
Ahmad Mehri, Sahar Sotoodeh Ghorbani, Kosar Farhadi-Babadi, Elham Rahimi, Zahra Barati, Niloufar Taherpour, Neda Izadi, Fatemeh Shahbazi, Yaser Mokhayeri, Arash Seifi, Saeid Fallah, Rezvan Feyzi, Koorosh Etemed, Seyed Saeed Hashemi Nazari
Journal of Intensive Care Medicine.2023; 38(9): 825. CrossRef - The association between stroke and COVID-19-related mortality: a systematic review and meta-analysis based on adjusted effect estimates
Shuwen Li, Jiahao Ren, Hongjie Hou, Xueya Han, Jie Xu, Guangcai Duan, Yadong Wang, Haiyan Yang
Neurological Sciences.2022; 43(7): 4049. CrossRef - Mental health status of dentists during COVID‐19 pandemic: A systematic review and meta‐analysis
Hamid Salehiniya, Sare Hatamian, Hamid Abbaszadeh
Health Science Reports.2022;[Epub] CrossRef - Laboratory biomarker predictors for disease progression and outcome among Egyptian COVID-19 patients
Lamiaa A Fathalla, Lamyaa M Kamal, Omina Salaheldin, Mahmoud A Khalil, Mahmoud M Kamel, Hagar H Fahim, Youssef AS Abdel-Moneim, Jawaher A Abdulhakim, Ahmed S Abdel-Moneim, Yomna M El-Meligui
International Journal of Immunopathology and Pharm.2022; 36: 039463202210962. CrossRef - Obesity and Infection: What Have We Learned From the COVID-19 Pandemic
Emilia Vassilopoulou, Roxana Silvia Bumbacea, Aikaterini Konstantina Pappa, Athanasios N. Papadopoulos, Dragos Bumbacea
Frontiers in Nutrition.2022;[Epub] CrossRef
- Obesity as a Risk Factor for Complications and Mortality in Individuals with SARS-CoV-2: A Systematic Review
- Characteristics of Inpatients Who Survive Suicide Attempts
- Sang Mi Kim, Hyun-Sook Lee
- Osong Public Health Res Perspect. 2019;10(1):32-38. Published online February 28, 2019
- DOI: https://doi.org/10.24171/j.phrp.2019.10.1.07
- 5,463 View
- 155 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The purpose of this study was to analyze the characteristics and factors affecting the survival of inpatients admitted following a suicide attempt.
Methods A total of 3,095 cases retrieved from the Korean National Hospital Discharge In-depth Injury Survey data (from 2011 to 2015) were grouped according to survival and death and analyzed using descriptive statistics chi-square and logistic regression analysis.
Results The following factors had statistically significant risks on reducing survival: female (OR = 2.352,
p < 0.001), 40–59 years old (OR = 0.606,p = 0.014), over 60 years old (OR = 0.186,p < 0.001), poisoning (OR = 0.474,p = 0.009), hanging (OR = 0.031,p < 0.001), jumping (OR = 0.144,p < 0.001), conflicts with family (OR = 2.851,p < 0.001), physical diseases (OR = 1.687,p = 0.046), mental health problems (OR = 2.693,p < 0.001), financial problems (OR = 3.314,p = 0.002), 2014 (OR = 2.498,p = < 0.001) and 2015 (OR = 2.942,p = 0.005).Conclusion The survival group that had a history of attempted suicide (high-risk suicide group), should be further characterized. It is necessary to identify the suicide methods and risk factors for suicide prevention management policies and to continuously expand the management policy according to these characteristics.
-
Citations
Citations to this article as recorded by- Factors Affecting Inpatients’ Mortality through Intentional Self-Harm at In-Hospitals in South Korea
Sulki Choi, Sangmi Kim, Hyunsook Lee
International Journal of Environmental Research an.2023; 20(4): 3095. CrossRef - The economic burden of adolescent internet addiction: A Korean health cost case study
Robert W. Mead, Edward Nall
The Social Science Journal.2023; : 1. CrossRef - Loss to follow-up in a population-wide brief contact intervention to prevent suicide attempts - The VigilanS program, France
Larissa Djembi Fossi, Christophe Debien, Anne-Laure Demarty, Guillaume Vaiva, Antoine Messiah, Xenia Gonda
PLOS ONE.2022; 17(3): e0263379. CrossRef
- Factors Affecting Inpatients’ Mortality through Intentional Self-Harm at In-Hospitals in South Korea
- Factors Related to Healthcare Service Quality in Long-term Care Hospitals in South Korea: A Mixed-methods Study
- Minsung Sohn, Mankyu Choi
- Osong Public Health Res Perspect. 2017;8(5):332-341. Published online October 31, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.5.07
- 3,995 View
- 31 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives The environment of long-term care hospitals (LTCHs) is critical to the management of the quality of their services and to patient safety, as highlighted by international studies. However, there is a lack of evidence on this topic in South Korea. This study aimed to examine the factors affecting healthcare quality in LTCHs and to explore the effectiveness of their quality management.
Methods This study used a mixed methods approach with quantitative data collected in a national survey and qualitative data from semi-structured interviews with practice-based managers. The samples included 725 nationally representative LTCHs in South Korea for the quantitative analysis and 15 administrators for the in-depth interviews.
Results A higher installation rate of patient-safety and hygiene-related facilities and staff with longer-tenures, especially nurses, were more likely to have better healthcare quality and education for both employees and patients.
Conclusion The need for patient-safety- and hygiene-related facilities in LTCHs that serve older adults reflects their vulnerability to certain adverse events (e.g., infections). Consistent and skillful nursing care to improve the quality of LTCHs can be achieved by developing relevant educational programs for staff and patients, thereby strengthening the relationships between them.
-
Citations
Citations to this article as recorded by- Improving Preparedness for and Response to Coronavirus Disease 19 (COVID-19) in Long-Term Care Hospitals in Korea
Tark Kim
Infection & Chemotherapy.2020; 52(2): 133. CrossRef - Identifying Potentially Avoidable Emergency Department Visits of Long-Term Care Hospital Residents in Korea: A Multicenter Retrospective Cohort Study
Keon Kim, Dong Hoon Lee, Ho Young Yune, Jung Hee Wee, Duk Ho Kim, Eui Chung Kim, Jee Yong Lim, Seung Pil Choi
BioMed Research International.2019; 2019: 1. CrossRef
- Improving Preparedness for and Response to Coronavirus Disease 19 (COVID-19) in Long-Term Care Hospitals in Korea
- Analysis of Hospital Volume and Factors Influencing Economic Outcomes in Cancer Surgery: Results from a Population-based Study in Korea
- Jung-A Lee, So-Young Kim, Keeho Park, Eun-Cheol Park, Jong-Hyock Park
- Osong Public Health Res Perspect. 2017;8(1):34-46. Published online February 28, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.1.05
- 4,075 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives To evaluate associations between hospital volume, costs, and length of stay (LOS), and clinical and demographic outcome factors for five types of cancer resection. The main dependent variables were cost and LOS; the primary independent variable was volume.
Methods Data were obtained from claims submitted to the Korean National Health Insurance scheme. We identified patients who underwent the following surgical procedures: pneumonectomy, colectomy, mastectomy, cystectomy, and esophagectomy. Hospital volumes were divided into quartiles.
Results Independent predictors of high costs and long LOS included old age, low health insurance contribution, non-metropolitan residents, emergency admission, Charlson score > 2, public hospital ownership, and teaching hospitals. After adjusting for relevant factors, there was an inverse relationship between volume and costs/LOS. The highest volume hospitals had the lowest procedure costs and LOS. However, this was not observed for cystectomy.
Conclusion Our findings suggest an association between patient and clinical factors and greater costs and LOS per surgical oncologic procedure, with the exception of cystectomy. Yet, there were no clear associations between hospitals’ cost of care and risk-adjusted mortality.
-
Citations
Citations to this article as recorded by- Impact of hospital volume on failure to rescue for complications requiring reoperation after elective colorectal surgery: multicentre propensity score–matched cohort study
Marie T Grönroos-Korhonen, Laura E Koskenvuo, Panu J Mentula, Taina P Nykänen, Selja K Koskensalo, Ari K Leppäniemi, Ville J Sallinen
BJS Open.2024;[Epub] CrossRef - Volume-outcome relationships in laryngeal trauma processes of care: a retrospective cohort study
David Forner, Christopher W. Noel, Matthew P. Guttman, Barbara Haas, Danny Enepekides, Matthew H. Rigby, S. Mark Taylor, Avery B. Nathens, Antoine Eskander
European Journal of Trauma and Emergency Surgery.2022; 48(5): 4131. CrossRef - Association between Stroke Quality Assessments and Mortality within 30 Days among Patients Who Underwent Hemorrhagic Stroke Surgeries in South Korea
Mi-Na Lee, Wonjeong Jeong, Sung-In Jang, Sohee Park, Eun-Cheol Park
Cerebrovascular Diseases.2022; 51(1): 82. CrossRef - Impact of surgeon and hospital factors on length of stay after colorectal surgery systematic review
Zubair Bayat, Keegan Guidolin, Basheer Elsolh, Charmaine De Castro, Erin Kennedy, Anand Govindarajan
BJS Open.2022;[Epub] CrossRef - Crucial areas of the economic analysis of public cancer care
D. A. Andreev, K. I. Polyakova, A. A. Zavyalov, T. N. Ermolaeva, A. G. Fisun, A. D. Ermolaeva, V. A. Dubovtseva, T. E. Maksimova
FARMAKOEKONOMIKA. Modern Pharmacoeconomic and Phar.2020; 12(4): 310. CrossRef - Initial Diagnosis of Colorectal Cancer through Colonoscopy or Emergent Surgery-Clinicopathological Features that Support Early Screening
Konstantinos A Paschos, A Chatzigeorgiadis
Hellenic Journal of Surgery.2020; 92(2): 51. CrossRef - What Matters in the Performance of a Medial Institution?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2017; 8(1): 1. CrossRef
- Impact of hospital volume on failure to rescue for complications requiring reoperation after elective colorectal surgery: multicentre propensity score–matched cohort study
- Knowledge Management Enablers and Process in Hospital Organizations
- Hyun-Sook Lee
- Osong Public Health Res Perspect. 2017;8(1):26-33. Published online February 28, 2017
- DOI: https://doi.org/10.24171/j.phrp.2017.8.1.04
- 4,907 View
- 118 Download
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives This research aimed to investigate the effects of knowledge management enablers, such as organizational structure, leadership, learning, information technology systems, trust, and collaboration, on the knowledge management process of creation, storage, sharing, and application.
Methods Using data from self-administered questionnaires in four Korean tertiary hospitals, this survey investigated the main organizational factors affecting the knowledge management process in these organizations. A total of 779 questionnaires were analyzed using SPSS 18.0 and AMOS 18.0.
Results The results showed that organizational factors affect the knowledge management process differently in each hospital organization.
Conclusion From a managerial perspective, the implications of these factors for developing organizational strategies that encourage and foster the knowledge management process are discussed.
-
Citations
Citations to this article as recorded by- Knowledge management effects and performance in health care: a systematic literature review
Ritva Kosklin, Johanna Lammintakanen, Tuula Kivinen
Knowledge Management Research & Practice.2023; 21(4): 738. CrossRef - Knowledge Sharing through Social Media Platforms in the Silicon Age
Muhammad Yaqub, Abdullah Alsabban
Sustainability.2023; 15(8): 6765. CrossRef - Success factors for evidence-based healthcare practice adoption
Lovemore Motsi, Bester Chimbo
SA Journal of Information Management.2023;[Epub] CrossRef - Leadership, healthcare and knowledge management
Guilherme Agnolin, Lúcia Worma, Édis Mafra Lapolli, Cristiano José Castro de Almeida Cunha
International Journal for Innovation Education and.2022; 10(10): 61. CrossRef - Alignment of knowledge management process with clinical process to support evidence based decision in healthcare improvements: The case of selected Ethiopian hospitals
Mniyichel Belay, Amare Desta, Steve Smithson, Million Meshesha
Knowledge and Process Management.2021; 28(1): 3. CrossRef - Knowledge management enablers affecting patient care: The perspective of registered nurses in South West Nigeria
Olateju J. Ajanaku, Stephen Mutula
SA Journal of Information Management.2021;[Epub] CrossRef - A gestão do conhecimento em contexto hospitalar: uma scoping review
Andreia Mesquita, Diana Santos, Vítor Raposo
Revista de Investigação & Inovação em Saúde.2021;[Epub] CrossRef - Structural Equation Modeling to Explore the Relationship Between Organizational Culture Dimensions and Implementation of Knowledge Management in Teaching Hospitals
Ahmad Rahbar, Amir Ashkan Nasiripour, Mahmood Mahmoodi-Majdabadi
Health Scope.2020;[Epub] CrossRef - Improvement of Innovation Ability of Hospital Managers and Construction of Competitive Strategy
Li Han, Jing Li, Wenfeng Chen
International Journal of Circuits, Systems and Sig.2020; 14: 751. CrossRef - Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations
Ion Popa, Simona Ștefan
International Journal of Environmental Research an.2019; 16(7): 1114. CrossRef - Implementation of Knowledge Management in Chinese Hospitals
Qiao-yuan Yan, Fei Xiang, Xiao-xu Shi, Qin Zhu
Current Medical Science.2018; 38(2): 372. CrossRef
- Knowledge management effects and performance in health care: a systematic literature review
- Evaluating Service Quality from Patients' Perceptions: Application of Importance–performance Analysis Method
- Rafat Mohebifar, Hana Hasani, Ameneh Barikani, Sima Rafiei
- Osong Public Health Res Perspect. 2016;7(4):233-238. Published online August 31, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.05.002
- 3,395 View
- 18 Download
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Providing high service quality is one of the main functions of health systems. Measuring service quality is the basic prerequisite for improving quality. The aim of this study was to evaluate the quality of service in teaching hospitals using importance–performance analysis matrix.
Methods
A descriptive–analytic study was conducted through a cross-sectional method in six academic hospitals of Qazvin, Iran, in 2012. A total of 360 patients contributed to the study. The sampling technique was stratified random sampling. Required data were collected based on a standard questionnaire (SERVQUAL). Data analysis was done through SPSS version 18 statistical software and importance–performance analysis matrix.
Results
The results showed a significant gap between importance and performance in all five dimensions of service quality (p < 0.05). In reviewing the gap, “reliability” (2.36) and “assurance” (2.24) dimensions had the highest quality gap and “responsiveness” had the lowest gap (1.97). Also, according to findings, reliability and assurance were in Quadrant (I), empathy was in Quadrant (II), and tangibles and responsiveness were in Quadrant (IV) of the importance–performance matrix.
Conclusion
The negative gap in all dimensions of quality shows that quality improvement is necessary in all dimensions. Using quality and diagnosis measurement instruments such as importance–performance analysis will help hospital managers with planning of service quality improvement and achieving long-term goals. -
Citations
Citations to this article as recorded by- A New Model to Consolidate Long-Term Intersectoral Partnerships in Humanitarian and Social Crises Management
Anderson Nunes da Silva, Marcele Elisa Fontana
Public Organization Review.2024; 24(1): 27. CrossRef - Evaluation of outpatient service quality: What do patients and providers think?
Pouria Farrokhi, Aidin Aryankhesal, Rafat Bagherzadeh, Asgar Aghaei Hashjin
International Journal of Healthcare Management.2023; 16(3): 394. CrossRef - Assessing the Challenges and Opportunities of Agricultural Information Systems to Enhance Farmers’ Capacity and Target Rice Production in Indonesia
Agung Budi Santoso, Setia Sari Girsang, Budi Raharjo, Arlyna Budi Pustika, Yanter Hutapea, Mahargono Kobarsih, Agus Suprihatin, Erpina Delina Manurung, Deddy Romulo Siagian, Sidiq Hanapi, Tommy Purba, Dorkas Parhusip, Sri Wahyuni Budiarti, Yeyen Prestyani
Sustainability.2023; 15(2): 1114. CrossRef - Patients’ views on health promotion and disease prevention services provided by healthcare workers in a South African tertiary hospital
Herbert I. Melariri, Chester Kalinda, Moses J. Chimbari
BMC Health Services Research.2023;[Epub] CrossRef - Telecommunication service quality analysis using integration of SIPA and modified Kano
Hanny Kanavika Rizky Munawar, Annisa Kesy Garside, Adhi Nugraha, Amelia Khoidir
Jurnal Sistem dan Manajemen Industri.2023; 7(1): 53. CrossRef - Identifying service quality gaps between patients and providers in a Native American outpatient clinic
Robert Dorsey, David Claudio, María A. Velázquez, Polly Petersen
BMC Health Services Research.2022;[Epub] CrossRef - Assessing the Utility and Patient Satisfaction of Virtual Retina Clinics During COVID-19 Pandemic
Leire Juaristi, Cristina Irigoyen, Jaione Chapartegui, Ane Guibelalde, Javier Mar
Clinical Ophthalmology.2022; Volume 16: 311. CrossRef - A social-media-based improvement index for urban renewal
Zhifang Wang, Hua Jie, Hongpeng Fu, Lu Wang, Hezhishi Jiang, Lu Ding, Yingjie Chen
Ecological Indicators.2022; 137: 108775. CrossRef - On the comparative use of social media data and survey data in prioritizing ecosystem services for cost-effective governance
Zhifang Wang, Hongpeng Fu, Yuqing Jian, Salman Qureshi, Hua Jie, Lu Wang
Ecosystem Services.2022; 56: 101446. CrossRef - Quality Assessment Methods of Hospital Services from the Viewpoint of Patients Based on Standard Assessment Models in Iran: A Narrative Review
Mehdi Rahimi, Fateme Solymani
Modern Care Journal.2022;[Epub] CrossRef - Responsiveness level and its effect on services quality from the viewpoints of the older adults hospitalized during COVID-19 pandemic
Ali Reza Yusefi, Esmat Rezabeigi Davarani, Salman Daneshi, Misagh Bastani, Gholamhossein Mehralian, Peivand Bastani
BMC Geriatrics.2022;[Epub] CrossRef - Ranking Hospital Hoteling Services from Patients’ Perspective Using Importance-Performance Analysis
Amir Karimkhany, Ehsan Zarei, Samira Arabi, Elahe Navvabi, Somayeh Anisi
Shiraz E-Medical Journal.2022;[Epub] CrossRef - Using the Kano model to associate the number of confirmed cases of COVID-19 in a population of 100,000 with case fatality rates: An observational study
Sheng-Yao Hsu, Tsair-Wei Chien, Yu-Tsen Yeh, Willy Chou
Medicine.2022; 101(37): e30648. CrossRef - Patient satisfaction with quality of care in public hospitals in Albania
Rezarta Kalaja, Marsida Krasniqi
Frontiers in Public Health.2022;[Epub] CrossRef - A Crisis in the Health System and Quality of Healthcare in Economically Developed Countries
Magdalena Biel, Katarzyna Grondys, Ane-Mari Androniceanu
International Journal of Environmental Research an.2022; 20(1): 469. CrossRef - An integrated approach for evaluating hospital service quality with linguistic preferences
Xiaobing Li, Zhen He
International Journal of Production Research.2021; 59(6): 1776. CrossRef - Rethinking health services operations to embrace patient experience of healthcare journey
Mahdi Mahdavi, Leila Doshmangir, Ebrahim Jaafaripooyan
The International Journal of Health Planning and M.2021; 36(6): 2020. CrossRef - A STUDY ON QUALITY OF SERVICES IN THE OUTPATIENT DEPARTMENT OF A MULTISPECIALTY TEACHING HOSPITAL
Nirmala Kumari, Keerthana Maria Pinto
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 117. CrossRef - Variation in compliance with safe surgery checklist in hospitals with different levels of patient safety culture
Saeed Asefzadeh, Sima Rafiei, Masoomeh Karimi
International Journal of Healthcare Management.2020; 13(sup1): 12. CrossRef - Assessment of Quality of Services Delivered to Iranian Patients with Cataract
Zahra Hashemi Dehaghi, Soad Mahfoozpour, Mahmoud Modiri, Fateme Alipour
Iranian Red Crescent Medical Journal.2020;[Epub] CrossRef - Gap between patient expectation and perception during pharmacist–patient communication at community pharmacy
Myeong Gyu Kim, Na Eun Lee, Hyun Soon Sohn
International Journal of Clinical Pharmacy.2020; 42(2): 677. CrossRef - Validating Service Quality (SERVQUAL) in Healthcare: Measuring Patient Satisfaction Using their Perceptions in Jordan
Mohammed Shaker Ibrahim
Journal of Information & Knowledge Management.2020; 19(01): 2040021. CrossRef - Evaluating the environmental protection strategy of a printed circuit board manufacturer using a T fuzzy importance performance analysis with Google Trends
Kuen-Suan Chen, Kuo-Ping Lin, Li-Ju Lin
Expert Systems with Applications.2020; 156: 113483. CrossRef - Methodologies for Determining the Service Quality of the Intercity Rail Service Based on Users’ Perceptions and Expectations in Thailand
Sajjakaj Jomnonkwao, Thanapong Champahom, Vatanavongs Ratanavaraha
Sustainability.2020; 12(10): 4259. CrossRef - Patients’ Views on Service Quality in Selected Iranian Hospitals: An Importance-Performance Analysis
Ehsan Zarei, Ali Bagheri, Abbas Daneshkohan, Soheila Khodakarim
Shiraz E-Medical Journal.2020;[Epub] CrossRef - Identification of quality gaps in healthcare services using the SERVQUAL instrument and importance-performance analysis in medical intensive care: a prospective study at a medical center in Taiwan
Shu-Ju Lu, Hsiu-O Kao, Bao-Lin Chang, Shu-Ing Gong, Shu-Mei Liu, Shih-Chi Ku, Jih-Shuin Jerng
BMC Health Services Research.2020;[Epub] CrossRef - Importance – Performance Analysis (IPA) of bus service attributes: A case study in a developing country
Javad Esmailpour, Kayvan Aghabayk, Mohammad Abrari Vajari, Chris De Gruyter
Transportation Research Part A: Policy and Practic.2020; 142: 129. CrossRef - The Effect of Quality Service Towards Outpatients Satisfaction at Poasia Community Health Centre
Adryan Fristiohady, La Ode Muhammad Fitrawan, Yusniati Dwi Pemudi, Ruslin Ruslin, Sunandar Ihsan, Ruslan Ruslan, La Ode Muhammad Julian Purnama
Borneo Journal of Pharmacy.2020; 3(4): 270. CrossRef - Gap of services quality expectation and perception based on SERVQUAL model in the selected hospital outpatient clinics affiliated with Iran University of Medical Sciences
asgar Aghaei Hashjin, Pouria Farrokhi, Aidin Aryankhesal
Journal of Health Administration.2020; 23(3): 55. CrossRef - An empirical study of willingness to renewable energy installation using importance-performance analysis: the case of Taiwan
Wei-Chuan Chen, Wen-Kuo Chen, Chien-Wen Chen, Chien-Cheng Lo
Journal of Industrial and Production Engineering.2019; 36(7): 451. CrossRef - Assessing management performance of the national forest park using impact range-performance analysis and impact-asymmetry analysis
Pin-Zheng Chen, Wan-Yu Liu
Forest Policy and Economics.2019; 104: 121. CrossRef - Do patients really perceive better quality of service in private hospitals than public hospitals in India?
Swapnarag Swain
Benchmarking: An International Journal.2019; 26(2): 590. CrossRef - Percepción de los usuarios frente a la calidad de atención en salud del servicio de consulta externa según el modelo SERVQUAL
Angélica Viviana Boada-Niño, Adriana Mayeth Barbosa-López, Elisa Andrea Cobo-Mejía
Revista Investigación en Salud Universidad de Boya.2019; 6(1): 55. CrossRef - Application of the SERVQUAL model to evaluate the quality in the transportation service in Morelia, Mexico
Marco Alberto Valenzo-Jiménez, Daniel Adan Lazaro-López, Jaime Apolinar Martínez- Arroyo
DYNA.2019; 86(211): 64. CrossRef - Konya İlinde Bulunan Özel Hastanelerdeki Hizmet Kalitesinin Ölçülmesi: Akademik Personele Yönelik Araştırma
Büşra Güler, Saadettin Erhan Kesen
Selçuk Üniversitesi Sosyal Bilimler Meslek Yükseko.2019; 22(2): 526. CrossRef - A Study on Service Quality and Customer Satisfaction in Nigerian Healthcare Sector
Rajasekhara Mouly Potluri, Gift Angiating
Journal of Industrial Distribution & Business.2018; 9(12): 7. CrossRef - Analysis of customer satisfaction in hospital by using Importance-Performance Analysis (IPA) and Customer Satisfaction Index (CSI)
Vembri Noor Helia, Cahya Putra Abdurrahman, Fety Ilma Rahmillah, S. Ma’mun, H. Tamura, M.R.A. Purnomo
MATEC Web of Conferences.2018; 154: 01098. CrossRef - Evaluating health service quality: using importance performance analysis
Azar Izadi, Younes Jahani, Sima Rafiei, Ali Masoud, Leila Vali
International Journal of Health Care Quality Assur.2017; 30(7): 656. CrossRef - Societal perception toward transportation modes based on online (Go-Jek) In Malang City
D M Buamona
IOP Conference Series: Earth and Environmental Sci.2017; 70: 012007. CrossRef - The Role of Subjective Culture on Consumer Perception towards Service Quality Delivery
Tiara Turay
Journal of Business and Social Review in Emerging .2016; 2(2): 175. CrossRef
- A New Model to Consolidate Long-Term Intersectoral Partnerships in Humanitarian and Social Crises Management
- Assessment of Service Quality in Teaching Hospitals of Yazd University of Medical Sciences: Using Multi-criteria Decision Making Techniques
- Milad Shafii, Sima Rafiei, Fatemeh Abooee, Mohammad Amin Bahrami, Mojtaba Nouhi, Farhad Lotfi, Khatere Khanjankhani
- Osong Public Health Res Perspect. 2016;7(4):239-247. Published online August 31, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.05.001
- 3,414 View
- 18 Download
- 29 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Hospitals as integrated parts of the wide-ranging health care systems have dominant focus on health care provision to meet, maintain and promote people's health needs of a community. This study aimed to assess the service quality of teaching hospitals of Yazd University of Medical Sciences using Fuzzy Analytical Hierarchy Process (FAHP) and Technique for Order Preference by Similarity to Ideal Solution (TOPSIS).
Methods
A literature review and a qualitative method were used to obtain experts' viewpoints about the quality dimensions of hospital services to design a questionnaire. Then, using a self-made questionnaire, perceptions of 300 patients about the quality of delivered services were gathered. Finally, FAHP was applied to weigh each quality dimension and TOPSIS method to rank hospital wards.
Results
Six dimensions including responsiveness, assurance, security, tangibles, health communication and Patient orientation were identified as affecting aspects of hospital services quality among which, security and tangibles got the highest and lowest importance respectively (0.25406, 0.06883). Findings also revealed that in hospital A, orthopedics and ophthalmology wards obtained the highest score in terms of quality while cardiology department got the lowest ranking (0.954, 0.323). In hospital B, the highest and the lowest ranking was belonged to cardiology and surgical wards (0.895, 0.00) while in hospital C, surgical units were rated higher than internal wards (0.959, 0.851).
Conclusion
Findings emphasized that the security dimension got the lowest ranking among SERVQUAL facets in studied hospitals. This requires hospital executives to pay special attention to the issue of patients’ security and plan effectively for its promotion. -
Citations
Citations to this article as recorded by- Developing a comprehensive service quality model for online to offline e-commerce platforms using a hybrid model
QiGan Shao, James J. H. Liou, SungShun Weng, HongBo Jiang, Ting Shao, ZhenWen Lin
Electronic Commerce Research.2024;[Epub] CrossRef - A multicriteria decision‐making framework for assessing the performance of gynecobstetrics departments: a case study
Miguel Ortíz‐Barrios, Edward Gutiérrez‐Severiche, Dayana Cómbita‐Niño, Genett Jiménez‐Delgado, Alessio Ishizaka, Maria Barbati, Zulmeira Herrera‐Fontalvo
International Transactions in Operational Research.2023; 30(1): 328. CrossRef - Healthcare Facilities Redesign Using Multicriteria Decision-Making: Fuzzy TOPSIS and Graph Heuristic Theories
Amr A. Hassanain, Mohamed A. A. Eldosoky, Ahmed M. Soliman, Yi-Zhang Jiang
Journal of Healthcare Engineering.2023; 2023: 1. CrossRef - A Novel Strategic Approach to Evaluating Higher Education Quality Standards in University Colleges Using Multi-Criteria Decision-Making
Anas A. Makki, Ammar Y. Alqahtani, Reda M. S. Abdulaal, Ayman I. Madbouly
Education Sciences.2023; 13(6): 577. CrossRef - EVALUATION OF MANAGERIAL PERFORMANCE BASED ON 360-DEGREE EVALUATION MODEL IN HEAD NURSES OF SHAHID CHAMRAN HEART TRAINING AND MEDICAL CENTER IN ISFAHAN IN 2021
Moahmmad Reza Shafiei, Mona Saadati, Farimah Shirani, Mohsen Moradi, Reihaneh Niknezhad, Mohammad Akbari
Nursing and Midwifery Journal.2023; 21(5): 366. CrossRef - Application of multi‐criteria decision‐making approach in healthcare surgical management
Bhaskar B. Gardas, Nilesh P. Ghongade, Annasaheb H. Jagtap
Journal of Multi-Criteria Decision Analysis.2022; 29(1-2): 92. CrossRef - Evaluation of service quality using SERVQUAL scale and machine learning algorithms: a case study in healthcare
Serkan Altuntas, Türkay Dereli, Zülfiye Erdoğan
Kybernetes.2022; 51(2): 846. CrossRef - Healthcare service quality evaluation: An integrated decision-making methodology and a case study
Ali Karasan, Melike Erdogan, Melih Cinar
Socio-Economic Planning Sciences.2022; 82: 101234. CrossRef - Utilizing Multi-Criteria Decision Making to Evaluate the Quality of Healthcare Services
Mohammed Al Awadh
Sustainability.2022; 14(19): 12745. CrossRef - Pay for performance in hospital management: A case study
Mohammad Haji Aghajani, Saeed Manavi, Ali Maher, Sima Rafiei, Ali Ayoubian, Ali Shahrami, Raziyeh Ronasiyan, Pooneh Maziar
International Journal of Healthcare Management.2021; 14(2): 484. CrossRef - An integrated approach for evaluating hospital service quality with linguistic preferences
Xiaobing Li, Zhen He
International Journal of Production Research.2021; 59(6): 1776. CrossRef - HASTANE HİZMETLERİ SEKTÖRÜNÜN CRITIC TEMELLİ TOPSIS YÖNTEMİ İLE FİNANSAL PERFORMANSININ DEĞERLENDİRİLMESİ
Cemre Eda ERKILIÇ
Pamukkale University Journal of Social Sciences In.2021;[Epub] CrossRef - Identifying and Ranking the Factors Affecting the Choice of Nursing Discipline Among Nursing Students in Iran: A Fuzzy Hierarchical Analysis
Zohreh Hosseini MARZNAKI, Khatere KHANJANKHANI, Waliu Jawula SALISU, Fatemeh HAJIHOSSEINI, Saeed BARZEGARI
Journal of Nursing Research.2021; 29(5): e171. CrossRef - Assessment of Quality of Services Delivered to Iranian Patients with Cataract
Zahra Hashemi Dehaghi, Soad Mahfoozpour, Mahmoud Modiri, Fateme Alipour
Iranian Red Crescent Medical Journal.2020;[Epub] CrossRef - Fuzzy Multicriteria Modelling of Decision Making in the Renewal of Healthcare Technologies
Sergio Domínguez, María Carmen Carnero
Mathematics.2020; 8(6): 944. CrossRef - Evaluation of healthcare service quality factors using grey relational analysis in a dialysis center
Erdal Aydemir, Yusuf Sahin
Grey Systems: Theory and Application.2019; 9(4): 432. CrossRef - Pathology the Process of Accreditation of Educational Institutions and Therapeutic Centers and Presentation an Appropriate Model
MM Chehrzad, AH Mahmoodi, K Fathivajargah, A Khorshidi, SM Samimi-Ardestani
Research in Medical Education.2019; 11(1): 37. CrossRef - Managerial competencies of head nurses: a model and assessment tool
Nader Markazi Moghaddam, Sanaz Zargar Balaye Jame, Sima Rafiei, Ali Asghari Sarem, Ashraf Ghamchili, Milad Shafii
British Journal of Nursing.2019; 28(1): 30. CrossRef - Application of decision making and fuzzy sets theory to evaluate the healthcare and medical problems: A review of three decades of research with recent developments
Abbas Mardani, Robert E. Hooker, Seckin Ozkul, Sun Yifan, Mehrbakhsh Nilashi, Hamed Zamani Sabzi, Goh Chin Fei
Expert Systems with Applications.2019; 137: 202. CrossRef - Construction and application of service quality evaluation system in the preclinical research on cardiovascular implant devices
Yongchun Cui, Fuliang Luo, Boqing Yang, Bin Li, Qi Zhang, Gopika Das, Guangxin Yue, Jiajie Li, Yue Tang, Xin Wang
BMC Medical Informatics and Decision Making.2019;[Epub] CrossRef - Developing strategies for patient safety implementation: a national study in Iran
Ali Maher, Ali Ayoubian, Sima Rafiei, Donya Sheibani Tehrani, Farnaz Mostofian, Pooneh Mazyar
International Journal of Health Care Quality Assur.2019; 32(8): 1113. CrossRef - Sağlık Sektöründe Hizmet Kalitesinin Çok Ölçütlü Karar Verme Yöntemleri İle Değerlendirilmesi: Ankara’da Bir Uygulama
Leman İnci Çanakçı Yüksel, Murat Arıkan
Uludağ University Journal of The Faculty of Engine.2019; : 13. CrossRef - Service Quality Evaluation of Container Terminals through AHM and Membership Degree Transformation
S. Hemalatha, Lingaraju Dumpala, B. Balakrishna
Materials Today: Proceedings.2019; 18: 155. CrossRef - Konya İlinde Bulunan Özel Hastanelerdeki Hizmet Kalitesinin Ölçülmesi: Akademik Personele Yönelik Araştırma
Büşra Güler, Saadettin Erhan Kesen
Selçuk Üniversitesi Sosyal Bilimler Meslek Yükseko.2019; 22(2): 526. CrossRef - Sağlık Otelciliğinde Hizmet Kalitesinin Marka Performansı Üzerine Etkisi
Çiğdem UNURLU
Anadolu Üniversitesi Sosyal Bilimler Dergisi.2019; 19(4): 61. CrossRef - Multicriteria decision analysis (MCDA) in health care: a systematic review of the main characteristics and methodological steps
Talita D. C. Frazão, Deyse G. G. Camilo, Eric L. S. Cabral, Ricardo P. Souza
BMC Medical Informatics and Decision Making.2018;[Epub] CrossRef - Service quality evaluation and ranking of container terminal operators through hybrid multi-criteria decision making methods
S. Hemalatha, Lingaraju Dumpala, B. Balakrishna
The Asian Journal of Shipping and Logistics.2018; 34(2): 137. CrossRef - Identification of Key Success Factors in the Marketing of Cosmetics Based on Knowledge, Attitude and Practice (KAP) Analysis Using Topsis Technique (The Case of Iran)
Mehdi Mohammadzadeh, Shirin Hashemi, Faranak Salmannejad, Tayebeh Ghari
Pharmaceutical Sciences.2017; 23(3): 222. CrossRef - Evaluation and Ranking of Service Quality in Four Public Hospitals in Iran using “Multi-Criteria Decision Making Methods”
Mohammad Ali Beheshtinia, Ahmad Torkzad
Journal of Health Promotion Managment.2017; 7(2): 34. CrossRef
- Developing a comprehensive service quality model for online to offline e-commerce platforms using a hybrid model
- The Mediating Role of Organizational Learning in the Relationship of Organizational Intelligence and Organizational Agility
- Mohammad Amin Bahrami, Mohammad Mehdi Kiani, Raziye Montazeralfaraj, Hossein Fallah Zadeh, Morteza Mohammad Zadeh
- Osong Public Health Res Perspect. 2016;7(3):190-196. Published online June 30, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.04.007
- 3,565 View
- 25 Download
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
Organizational learning is defined as creating, absorbing, retaining, transferring, and application of knowledge within an organization. This article aims to examine the mediating role of organizational learning in the relationship of organizational intelligence and organizational agility.
Methods
This analytical and cross-sectional study was conducted in 2015 at four teaching hospitals of Yazd city, Iran. A total of 370 administrative and medical staff contributed to the study. We used stratified-random method for sampling. Required data were gathered using three valid questionnaires including Alberkht (2003) organizational intelligence, Neefe (2001) organizational learning, and Sharifi and Zhang (1999) organizational agility questionnaires. Data analysis was done through R and SPSS 18 statistical software.
Results
The results showed that organizational learning acts as a mediator in the relationship of organizational intelligence and organizational agility (path coefficient = 0.943). Also, organizational learning has a statistical relationship with organizational agility (path coefficient = 0.382).
Conclusion
Our findings suggest that the improvement of organizational learning abilities can affect an organization's agility which is crucial for its survival. -
Citations
Citations to this article as recorded by- Comparing Promotability Outlooks: Industry Professionals vs. MBA Student Perspectives
Vicente E. Montaño, Myrna S. Viado
European Journal of Contemporary Education and E-L.2024; 2(1): 112. CrossRef - Survey-Based Studies of the Agility Construct in the Healthcare Sector: A Systematic Literature Review
Jorge Flavio Sarmiento Falla, Waldemar Karwowski
Applied Sciences.2024; 14(3): 1097. CrossRef - Structural Equation Modeling: Effects of Master Adaptive Learner and Clinical Learning Environment Attributes on Career Satisfaction and Intention to Stay
Raine Osborne, Chloe Bailey, Daniel Dinsmore, Emily Lyter, Judy Burnfield, Holly Medearis, Amanda Roura
Physical Therapy.2024;[Epub] CrossRef - Social Media Engagement, Organizational Agility and Digitalization Strategic Plan to Improve SMEs’ Performance
Hasan Abdul Rozak, Ardian Adhiatma, Olivia Fachrunnisa, Tina Rahayu
IEEE Transactions on Engineering Management.2023; 70(11): 3766. CrossRef - Differential impact of work-based learning on employee agility, ambidexterity and proactive goal generation
Charles Hanu, Hayford Amegbe, Monica Dede Tekyi Ansah Yawson, Philip Mensah
Journal of Workplace Learning.2023; 35(1): 92. CrossRef - Understanding the role of organizational agility in the context of digital transformation: an integrative literature review
Cheng Gong, Vincent Ribiere
VINE Journal of Information and Knowledge Manageme.2023;[Epub] CrossRef - Learning Organization and Innovation Coaching Model Organizational Agility Approach: A Case Study
Samet GÜRSEV
European Journal of Science and Technology.2023;[Epub] CrossRef - Sağlık Kurumlarında Örgütsel Çeviklik: Kavramsal Bir Çerçeve
Pelinsu Buket DOĞANYİĞİT
Türkiye Sağlık Bilimleri ve Araştırmaları Dergisi.2023; 6(2): 66. CrossRef - Does learning culture enhance organizational performance? A serial mediator with knowledge management and organizational intelligence
Jamini Ranjan Meher, Rohita Kumar Mishra, Rashmi Ranjan Panigrahi, Gokulananda Patel, Lalatendu Kesari Jena
Knowledge Management Research & Practice.2023; : 1. CrossRef - Teachers' intrinsic and extrinsic motivation as mediators of the effect of principals' perceived distributed leadership on organizational learning capability
Izhak Berkovich, Tahani Hassan
International Journal of Educational Management.2023; 37(6/7): 1552. CrossRef - SAĞLIK KURULUŞLARINDA BİLGİ SİSTEMLERİ KULLANIMININ ÖRGÜTSEL ÇEVİKLİK VE ÇALIŞAN MEMNUNİYETİ ÜZERİNE ETKİSİ
Mustafa ALTINTAŞ, Musa ÖZATA
Anadolu Üniversitesi İktisadi ve İdari Bilimler Fa.2023; 24(4): 333. CrossRef - Why do I contribute to organizational learning when I am ostracized? A moderated mediation analysis
Muhammad Kashif Imran, Jawad Iqbal, Tehreem Fatima, Syed Muhammad Javed Iqbal, Warda Najeeb Jamal, Muhammad Shahid Nawaz
Journal of Management & Organization.2022; 28(2): 261. CrossRef - Examining the role of knowledge sharing on employee performance with a mediating effect of organizational learning
Jamini Ranjan Meher, Rohita Kumar Mishra
VINE Journal of Information and Knowledge Manageme.2022; 52(2): 205. CrossRef - Influence of workforce agility on crisis management: Role of job characteristics and higher administrative support in public administration
Pradeep Kumar Raut, Jyoti Ranjan Das, Jyotiranjan Gochhayat, Kalyan Prasad Das
Materials Today: Proceedings.2022; 61: 647. CrossRef - Organisational agility, environmental knowledge and green product success
Jose Rabal-Conesa, Daniel Jiménez-Jiménez, Micaela Martínez-Costa
Journal of Knowledge Management.2022; 26(9): 2440. CrossRef - Towards Examining the Link Between Workplace Spirituality and Workforce Agility: Exploring Higher Educational Institutions
Imran Saeed, Jawad Khan, Muhammad Zada, Rezwan Ullah, Alejandro Vega-Muñoz, Nicolás Contreras-Barraza
Psychology Research and Behavior Management.2022; Volume 15: 31. CrossRef - A qualitative analysis and a conceptual model for organizational stupidity
Samaneh Karimi-Ghartemani, Naser Khani, Ali Nasr Isfahani
Journal of Organizational Change Management.2022; 35(3): 441. CrossRef - ENDÜSTRİYEL ÇEVİK İŞLETME İÇİN DENGELENMİŞ BAŞARI GÖSTERGELERİ
Alperen Ekrem ÇELİKDİN
Çukurova Üniversitesi Sosyal Bilimler Enstitüsü De.2022; 31(1): 38. CrossRef - Organizational learning culture and business intelligence systems of health-care organizations in an emerging economy
Md. Shamsul Arefin, Md. Rakibul Hoque, Tareq Rasul
Journal of Knowledge Management.2021; 25(3): 573. CrossRef - Investigating the role of social networking technology on the organizational agility: a structural equation modeling approach
Shadi Ahmadi, Mohammad Javad Ershadi
Journal of Advances in Management Research.2021; 18(4): 568. CrossRef - Mediating Effect of Organizational Learning Capacity on the Relationship between Relational Embeddedness and Innovation Performance in Freight Logistics Service
Pengxia Bai, Qunqi Wu, Qian Li, Chenlei Xue, Lei Zhang, Zhihan Lv
Complexity.2021; 2021: 1. CrossRef - Creating a Work Environment Conducive to Organizational Learning
Bret Lyman, Marisa E. Biddulph, V. Grace Hopper, Morgan K. Horton, Camille R. Mendon, Kylie C. Thorum, Emily L. Smith
The Journal of Continuing Education in Nursing.2021; 52(6): 281. CrossRef - Organizational Intelligence and Market Expansion in Jordanian Pharmaceutical Companies
Najm A. Najm, Amany A. H. Alfaqih
Organizations and Markets in Emerging Economies.2021; 12(1): 222. CrossRef - Modeling organizational intelligence, learning, forgetting and agility using structural equation model approaches in Shiraz University of Medical Sciences Hospitals
Zahra Kavosi, Sajad Delavari, Mohammad Mehdi Kiani, Peivand Bastani, Mohebat Vali, Marzieh Salehi
BMC Research Notes.2021;[Epub] CrossRef - KESAN INTEGRASI KELAKUAN KUMPULAN PENGURUSAN ATASAN KE ATAS KETANGKASAN ORGANISASI DI MALAYSIA: KAPASITI PENYERAPAN SEBAGAI PEMBOLEH UBAH PENGANTARA (The Effects of Top Management Team Behavioural Integration on Organisational Agility in Malaysia: Absorp
Khairul Naziya Kasim, Sofiah Md Auzair, Amizawati Mohd Amir, Nor Liza Abdullah
International Journal of Management Studies.2021;[Epub] CrossRef - Estudio bibliométrico de la relación del Cambio Organizacional con el Aprendizaje Organizacional
Luis Alberto Bellon Álvarez, Francisco Javier López Cerpa, Margarita Isabel Islas Villanueva
Vinculatégica.2021;[Epub] CrossRef - Dynamic talent management capabilities and organizational agility—A qualitative exploration
Katharina Harsch, Marion Festing
Human Resource Management.2020; 59(1): 43. CrossRef - Study of the impact mechanism of inter-organizational learning on alliance performance—with relationship capital as the mediator
Lu Shan, Li Dan, Yu-mou Qiu
Neural Computing and Applications.2020; 32(1): 117. CrossRef - Workforce agility and its links to emotional intelligence and workforce performance: A study of small entrepreneurial firms in India
Deepanjana Varshney, Nirbhay Krishna Varshney
Global Business and Organizational Excellence.2020; 39(5): 35. CrossRef - Love your mistakes!—they help you adapt to change. How do knowledge, collaboration and learning cultures foster organizational intelligence?
Wioleta Kucharska, Denise A.D. Bedford
Journal of Organizational Change Management.2020; 33(7): 1329. CrossRef - ÖRGÜT KÜLTÜRÜ ALGISININ ÖRGÜTSEL ÇEVİKLİK ÜZERİNDEKİ ETKİSİNİN İNCELENMESİ
Suzan BASRI, Kürşad ZORLU
Sosyal Ekonomik Araştırmalar Dergisi.2020; 20(39): 147. CrossRef - Investigating the Impact of Using Knowledge Management on Organisational Agility through Competitive Intelligence and Strategic Thinking
Hossein Sayyadi Tooranloo, Sepideh Saghafi
Journal of Information & Knowledge Management.2019; 18(02): 1950016. CrossRef - The effect of knowledge management, e-learning systems and organizational learning on organizational intelligence
Zeynab Soltani, Batool Zareie, Leila Rajabiun, Ali Agha Mohseni Fashami
Kybernetes.2019; 49(10): 2455. CrossRef - Knowledge management infrastructures and organizational intelligence in Iranian research centers
Hamid Keshavarz, Mohammad Reza Esmaili Givi, Mohammad Reza Shekari
Data Technologies and Applications.2018; 52(1): 2. CrossRef - Örgütsel Çeviklik Ölçeğinin Türkçeye Uyarlanması: Geçerlik ve Güvenirlik Çalışması
Bülent AKKAYA, Akif TABAK
İş ve İnsan Dergisi.2018; 5(2): 185. CrossRef - Evaluating indicators of the agility of the green supply chain
Hossein Sayyadi Tooranloo, Masoume Alavi, Sepideh Saghafi
Competitiveness Review.2018; 28(5): 541. CrossRef - Design thinking is ambidextrous
Dan-Ling Zheng
Management Decision.2018; 56(4): 736. CrossRef
- Comparing Promotability Outlooks: Industry Professionals vs. MBA Student Perspectives
- Competitive Strategy for Successful National University Hospital Management in the Republic of Korea
- Munjae Lee
- Osong Public Health Res Perspect. 2016;7(3):149-156. Published online June 30, 2016
- DOI: https://doi.org/10.1016/j.phrp.2016.02.002
- 2,772 View
- 18 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study provides information to aid decision making for managers and the staff of national university hospitals through analyzing their financial statements.
Methods
In order to analyze the finances of national university hospitals, this study used the report of final accounts announced by each hospital from 2009 to 2012 as baseline data. The research participants were 10 national university hospitals.
Results
According to the results of the analysis, most hospitals (except for a few) had medical expenses exceeding their medical revenues, resulting in a net deficit; however, there were significant differences amongst the hospitals. The result of adjustments based on a standard size of 100 beds showed that most hospitals had medical revenue deficits, and there were significant differences between hospitals in terms of medical revenues and medical costs.
Conclusion
It is not clear whether an expansion of national university hospitals is always beneficial for increasing net revenues, and it is necessary to establish a differentiation strategy to increase profitability by securing financial soundness instead of externally-oriented growth. -
Citations
Citations to this article as recorded by- Internal Quality Process Management Evaluation in Higher Education by Students
Lucie Vnoučková, Hana Urbancová, Helena Smolová
Danube.2018; 9(2): 63. CrossRef - What Would Be a Better Strategy for National University Hospital Management?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2016; 7(3): 139. CrossRef
- Internal Quality Process Management Evaluation in Higher Education by Students
- Role of Organizational Climate in Organizational Commitment: The Case of Teaching Hospitals
- Mohammad Amin Bahrami, Omid Barati, Malake-sadat Ghoroghchian, Razieh Montazer-alfaraj, Mohammad Ranjbar Ezzatabadi
- Osong Public Health Res Perspect. 2016;7(2):96-100. Published online April 30, 2016
- DOI: https://doi.org/10.1016/j.phrp.2015.11.009
- 3,562 View
- 18 Download
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objective
The commitment of employees is affected by several factors, including factors related to the organizational climate. The aim of this study was to investigate the relationship between organizational commitment of nurses and the organizational climate in hospital settings.
Methods
A cross-sectional study was conducted in 2014 at two teaching hospitals in Yazd, Iran. A total of 90 nurses in these hospitals participated. We used stratified random sampling of the nursing population. The required data were gathered using two valid questionnaires: Allen and Meyer's organizational commitment standard questionnaire and Halpin and Croft's Organizational Climate Description Questionnaire. Data analysis was done through SPSS 20 statistical software (IBM Corp., Armonk, NY, USA). We used descriptive statistics and Pearson's correlation coefficient for the data analysis.
Results
The findings indicated a positive and significant correlation between organizational commitment and organizational climate (r = 0.269, p = 0.01). There is also a significant positive relationship between avoidance of organizational climate and affective commitment (r = 0.208, p = 0.049) and between focus on production and normative and continuance commitment (r = 0.308, p = 0.003).
Conclusion
Improving the organizational climate could be a valuable strategy for improving organizational commitment. -
Citations
Citations to this article as recorded by- Organizational Commitment in Kermanshah University of Medical Sciences Faculty Members
Mehdi Mirzaei-Alavijeh, Farzad Jalilian
Educational Research in Medical Sciences.2024;[Epub] CrossRef - Status and related factors of professional growth among young nursing talents: a cross-sectional study in China
Xiuwen Chen, Liqing Yue, Bingyu Li, Jun Li, Xiuying Wu, Bin Peng, Ziwei Cao
BMC Nursing.2024;[Epub] CrossRef - Clima institucional y desempeño laboral de los servidores del SIS- UDR en Amazonas
Casimiro Eulogio Carlos Ramos, Freddy Manuel Camacho Delgado, Roxana Mabel Sempértegui Rafael, Luz Angélica Ríos Pérez
Alpha Centauri.2023; 4(1): 02. CrossRef - Beyond the global attachment model: domain- and relationship-specific attachment models at work and their functions
Katarína Greškovičová, Elena Lisá
Frontiers in Psychology.2023;[Epub] CrossRef - Measuring Nurses’ Organizational Well-Being: A Systematic Review of Available Instruments
Giovanni Gioiello, Francesco Zaghini, Valerio Della Bella, Jacopo Fiorini, Alessandro Sili
Evaluation & the Health Professions.2023;[Epub] CrossRef - Employee Affiliation and Presenteeism in Health-care Settings
Jasmina Starc, Tanja Regina Fabjan
Open Access Macedonian Journal of Medical Sciences.2023; 11(E): 338. CrossRef - Organisational Commitment and Turnover Intentions: Does Self-Efficacy Matter?
Julius Samuel Opolot, Charles Lagat, Stanley Kipsang
SEISENSE Journal of Management.2023; 6(1): 123. CrossRef - Mapping the Research Landscape of Organizational Climate and Performance Using Bibliometric Analysis
S.I. Amalou, B. Brahimi
Modelling and Data Analysis.2023; 13(3): 7. CrossRef - Investment sector employees’ career adaptability and organisational commitment
Felicity Nyathi, Rudolf M. Oosthuizen
SA Journal of Industrial Psychology.2023;[Epub] CrossRef - Development and validation of an improved DeLone-McLean IS success model - application to the evaluation of a tax administration ERP
Godwin Banafo Akrong, Shao Yunfei, Ebenezer Owusu
International Journal of Accounting Information Sy.2022; 47: 100579. CrossRef - Distributed leadership and organizational commitment: moderating role of confidence and affective climate
Sinda Ben Sedrine, Amel Sabra Bouderbala, Myryam Hamdi
European Business Review.2021; 33(4): 597. CrossRef - The Effect of Perceived Organizational Climate on the Performance of Nurses in Private Hospitals
Abbas Shahnavazi, Hamid Bouraghi, Mehdi Fadaei Eshkiki, Hossein Shahnavazi
Journal of Clinical Research in Paramedical Scienc.2021;[Epub] CrossRef - Measuring organizational climate via psychological networks analysis
Igor Menezes, Ana Cristina Menezes, Elton Moraes, Pedro P. Pires
International Journal of Organization Theory & Beh.2021; 24(3): 229. CrossRef - Development and testing of an evidence-based model of mentoring nursing students in clinical practice
Kristina Mikkonen, Marco Tomietto, Giancarlo Cicolini, Boris Miha Kaucic, Bojana Filej, Olga Riklikiene, Erika Juskauskiene, Flores Vizcaya-Moreno, Rosa M. Pérez-Cañaveras, Paul De Raeve, Maria Kääriäinen
Nurse Education Today.2020; 85: 104272. CrossRef - El clima y la satisfacción laboral del capital humano: factores diferenciados en organizaciones públicas y privadas
Norma Angélica Pedraza
Innovar.2020; 30(76): 9. CrossRef - Correlates of Organisational Commitment Among University Teachers in India: An Empirical Investigation
Barooj Bashir, Abdul Gani
Asia-Pacific Journal of Management Research and In.2020; 16(1): 7. CrossRef - Factors Affecting the Organizational Commitment of Nurses in Comprehensive Health Services: A Systematic Review
Erfan Rofiqi, Rahayu Tri Nuritasari, Pipit Festi Wiliyanarti
Jurnal Ners.2020; 14(3): 195. CrossRef - La relación del clima organizacional y el desempeño laboral en educación superior
Norma Angélica Pedraza-Melo, Lisseth Marlene Álvarez-de León, Isaí Rodolfo Cruz-Fuentes
Vinculatégica EFAN.2020; 6(1): 476. CrossRef - Factors Affecting the Family Physicians' Intention to Leave the Job: A Case of Iran
Rita Rezaee, Pegah Shoaahaghighi, Najmeh Bordbar, Karam Tavani, Ramin Ravangard
The Open Public Health Journal.2019; 12(1): 482. CrossRef - The effect of collegial solidarity among nurses on the organizational climate
E. Kılıç, S. Altuntaş
International Nursing Review.2019; 66(3): 356. CrossRef - Fostering employee commitment through work engagement: The moderating effect of job satisfaction in a developing-country setting
Jeremy Mitonga-Monga
Journal of Psychology in Africa.2019; 29(6): 546. CrossRef - An analysis of the relationship between occupational stress and employee job performance in public health care institutions: A case study of public hospitals in Harare
Tawaziwa Wushe, Jacob Shenje
SA Journal of Human Resource Management.2019;[Epub] CrossRef - Can work-related stress and job satisfaction affect job commitment among nurses? A cross-sectional study
Mahdi Eskandari, Mohammad Ali Heidari Gorji
F1000Research.2018; 7: 218. CrossRef - Role of Organizational Climate in Job Involvement: A Way to Develop the Organizational Commitment of Nursing Staff
Rohollah Kalhor, Omid Khosravizadeh, Saeideh Moosavi, Mohammad Heidari, Hasan Habibi
Journal of Evidence-Based Integrative Medicine.2018; 23: 2515690X1879072. CrossRef - The Quintessence of Organizational Commitment and Organizational Cynicism
Aida Margelytė-Pleskienė, Jolita Vveinhardt
Management of Organizations: Systematic Research.2018; 80(1): 67. CrossRef - Influence of organizational culture and leadership style on employee satisfaction, commitment and motivation in the educational sector in Qatar
Maryam Al-Sada, Bader Al-Esmael, Mohd. Nishat Faisal
EuroMed Journal of Business.2017; 12(2): 163. CrossRef - Job Motivating Potential Score and Its Relationship with Employees' Organizational Commitment among Health Professionals
Mohammad Amin Bahrami, Ali Aghaei, Omid Barati, Arefeh Dehghani Tafti, Mohammad Ranjbar Ezzatabadi
Osong Public Health and Research Perspectives.2016;[Epub] CrossRef
- Organizational Commitment in Kermanshah University of Medical Sciences Faculty Members
- Financial Analysis of National University Hospitals in Korea
- Munjae Lee
- Osong Public Health Res Perspect. 2015;6(5):310-317. Published online October 31, 2015
- DOI: https://doi.org/10.1016/j.phrp.2015.10.007
- 3,188 View
- 20 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This paper provides information for decision making of the managers and the staff of national university hospitals.
Methods
In order to conduct a financial analysis of national university hospitals, this study uses reports on the final accounts of 10 university hospitals from 2008 to 2011.
Results
The results of comparing 2008 and 2011 showed that there was a general decrease in total assets, an increase in liabilities, and a decrease in total medical revenues, with a continuous deficit in many hospitals. Moreover, as national university hospitals have low debt dependence, their management conditions generally seem satisfactory. However, some individual hospitals suffer severe financial difficulties and thus depend on short-term debts, which generally aggravate the profit and loss structure. Various indicators show that the financial state and business performance of national university hospitals have been deteriorating.
Conclusion
These research findings will be used as important basic data for managers who make direct decisions in this uncertain business environment or by researchers who analyze the medical industry to enable informed decision-making and optimized execution. Furthermore, this study is expected to contribute to raising government awareness of the need to foster and support the national university hospital industry. -
Citations
Citations to this article as recorded by- Türkiye’de 2009-2021 Yılları Arasında Sağlık İşletmelerinde Gerçekleşen Finansal Performans Analizi
İzzet AYDEMİR
MANAS Sosyal Araştırmalar Dergisi.2024; 13(1): 186. CrossRef - Financial and non-financial determinants of the indebtedness of hospitals. The case of Poland
Katarzyna Miszczyńska, Elżbieta Antczak
Journal of Management Analytics.2024; 11(1): 26. CrossRef - The Hospital Cost Reduction Strategies from the Managers’ Point of View: A Qualitative Study in Iran
Hesam Seyedin, Mona Moghimi, Salime Goharinezhad, Mohamad Azmal, Rohollah Kalhor
Health Scope.2024;[Epub] CrossRef - Financial Performance and Profile of Brazilian Hospitals
Mariana Guerra, Beatriz Fátima Morgan, Micael Conoring D’Assumpção Alves
Journal of Health Management.2022; 24(2): 175. CrossRef - Covid-19 Pandemisinin Sağlık İşletmelerine Finansal Etkisi: MLP Sağlık Grubu Örneği
Aydın ŞENOL, Mehmet Halit METİN
Bucak İşletme Fakültesi Dergisi.2022; 5(2): 233. CrossRef - Debt, Ownership, and Size: The Case of Hospitals in Poland
Katarzyna Miszczyńska, Piotr Miszczyński
International Journal of Environmental Research an.2021; 18(9): 4596. CrossRef - Financial Performance of Public Hospitals: A Cross-Sectional Study among Polish Providers
Katarzyna Dubas-Jakóbczyk, Ewa Kocot, Anna Kozieł
International Journal of Environmental Research an.2020; 17(7): 2188. CrossRef - Social Responsibility, Communication and Financial Data of Hospitals: A Structural Modelling Approach in a Sustainability Scope
Judit Creixans-Tenas, Dolores Gallardo-Vázquez, Núria Arimany-Serrat
Sustainability.2020; 12(12): 4857. CrossRef - The thinking process of the theory of constraints applied to public healthcare
Jéssica Mariela Bauer, Andrea Vargas, Miguel Afonso Sellitto, Mariane Cásseres Souza, Guilherme Luís Vaccaro
Business Process Management Journal.2019; 25(7): 1543. CrossRef - Corporate social responsibility and financial profile of Spanish private hospitals
J. Creixans-Tenas, G. Coenders, N. Arimany-Serrat
Heliyon.2019; 5(10): e02623. CrossRef - What Would Be a Better Strategy for National University Hospital Management?
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2016; 7(3): 139. CrossRef - The impact of Value Incentive Program (VIP) on the quality of hospital care for acute stroke in Korea
Ju Hyun Yang, Sun Min Kim, Seung Jin Han, Meredith Knaak, Gi Hwa Yang, Kyoo Duck Lee, Young Hee Yoo, Guja Ha, Eun Jung Kim, Myung Sook Yoo
International Journal for Quality in Health Care.2016; 28(5): 580. CrossRef - Competitive Strategy for Successful National University Hospital Management in the Republic of Korea
Munjae Lee
Osong Public Health and Research Perspectives.2016; 7(3): 149. CrossRef
- Türkiye’de 2009-2021 Yılları Arasında Sağlık İşletmelerinde Gerçekleşen Finansal Performans Analizi
- Assessment of Intensive Vaccination and Antiviral Treatment in 2009 Influenza Pandemic in Korea
- Chaeshin Chu, Sunmi Lee
- Osong Public Health Res Perspect. 2015;6(1):47-51. Published online February 28, 2015
- DOI: https://doi.org/10.1016/j.phrp.2014.11.007
- 2,711 View
- 17 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
We characterized and assessed public health measures, including intensive vaccination and antiviral treatment, implemented during the 2009 influenza pandemic in the Republic of Korea.
Methods
A mathematical model for the 2009 influenza pandemic is formulated. The transmission rate, the vaccination rate, the antiviral treatment rate, and the hospitalized rate are estimated using the least-squares method for the 2009 data of the incidence curves of the infected, vaccinated, treated, and hospitalized.
Results
The cumulative number of infected cases has reduced significantly following the implementation of the intensive vaccination and antiviral treatment. In particular, the intensive vaccination was the most critical factor that prevented severe outbreak.
Conclusion
We have found that the total infected proportion would increase by approximately six times under the half of vaccination rates. -
Citations
Citations to this article as recorded by- Modeling influenza transmission dynamics with media coverage data of the 2009 H1N1 outbreak in Korea
Yunhwan Kim, Ana Vivas Barber, Sunmi Lee, Roberto Barrio
PLOS ONE.2020; 15(6): e0232580. CrossRef - Doing Mathematics with Aftermath of Pandemic Influenza 2009
Hae-Wol Cho, Chaeshin Chu
Osong Public Health and Research Perspectives.2015; 6(1): 1. CrossRef
- Modeling influenza transmission dynamics with media coverage data of the 2009 H1N1 outbreak in Korea
- Improving Service Quality in Long-term Care Hospitals: National Evaluation on Long-term Care Hospitals and Employees Perception of Quality Dimensions
- Jinkyung Kim, Woosok Han
- Osong Public Health Res Perspect. 2012;3(2):94-99. Published online June 30, 2012
- DOI: https://doi.org/10.1016/j.phrp.2012.04.005
- 2,764 View
- 16 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
To investigate predictors for specific dimensions of service quality perceived by hospital employees in long-term care hospitals.
Methods
Data collected from a survey of 298 hospital employees in 18 long-term care hospitals were analysed. Multivariate ordinary least squares regression analysis with hospital fixed effects was used to determine the predictors of service quality using respondents’ and organizational characteristics.
Results
The most significant predictors of employee-perceived service quality were job satisfaction and degree of consent on national evaluation criteria. National evaluation results on long-term care hospitals and work environment also had positive effects on service quality.
Conclusion
The findings of the study show that organizational characteristics are significant determinants of service quality in long-term care hospitals. Assessment of the extent to which hospitals address factors related to employeeperceived quality of services could be the first step in quality improvement activities. Results have implications for efforts to improve service quality in longterm care hospitals and designing more comprehensive national evaluation criteria. -
Citations
Citations to this article as recorded by- The assessment of quality of care in the Indian healthcare industry: the employees’ and patients’ perspectives
Karthik Padamata, Rama Devi Vangapandu
Benchmarking: An International Journal.2023;[Epub] CrossRef - The perception of health care quality by primary health care managers in Ukraine
Valentyna Anufriyeva, Milena Pavlova, Tetiana Stepurko, Wim Groot
BMC Health Services Research.2022;[Epub] CrossRef - Primary Health Institutions and Service Quality in China: Implications for Health Policy
Junfang Xu, Yuyin Zhou, Ruyu Liu, Feng Cheng, Wannian Liang
International Journal of Environmental Research an.2022; 19(19): 12063. CrossRef - Lean Healthcare Readiness Evaluation among Staff in Private Hospital
Nihayatul Munaa, Faizatul Ummah, M.I. Kartasurya, N. Lisnawati, A.F. Asna, N. Handayani, D.Z. Nuridzin
BIO Web of Conferences.2022; 54: 00015. CrossRef - A tool to assess the quality perception of healthcare employees
Ajayan Kamalasanan, Gurumoorthy Sathiyamurthi, Arun Vijay Subbarayalu
International Journal of Health Care Quality Assur.2020; 33(4/5): 291. CrossRef - Dimensions of service quality in healthcare: a systematic review of literature
Iram Fatima, Ayesha Humayun, Usman Iqbal, Muhammad Shafiq
International Journal for Quality in Health Care.2019; 31(1): 11. CrossRef - Using the Importance–Satisfaction Model and Service Quality Performance Matrix to Improve Long-Term Care Service Quality in Taiwan
Shun-Hsing Chen, Fan-Yun Pai, Tsu-Ming Yeh
Applied Sciences.2019; 10(1): 85. CrossRef - Jurnal Kualitas Pelayanan Kesehatan (Studi Analitik Terhadap Pasien Rawat Jalan di RSUD Makassar)
Andi Alim, Novagita Tangdilambi, Adam Badwi
Jurnal Manajemen Kesehatan Yayasan RS.Dr. Soetomo.2019; 5(2): 165. CrossRef - Manufacturers’ perceived quality of electricity service and organizational performance in Nigeria
Abdulrahman Muhammed, Lamidi Yusuf
Journal of Transportation and Logistics.2016; 1(2): 143. CrossRef - Public Health Services for Foreign Workers in Malaysia
Normah Awang Noh, Haris Abd. Wahab, Siti Hajar Abu Bakar Ah, M. Rezaul Islam
Social Work in Public Health.2016; 31(5): 419. CrossRef
- The assessment of quality of care in the Indian healthcare industry: the employees’ and patients’ perspectives



 First
First Prev
Prev


